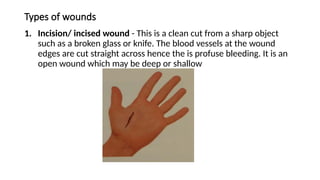
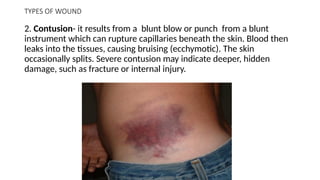
The document provides an overview of skin integrity and wound care, detailing types of wounds, the healing process, and factors influencing healing. It categorizes wounds into several types (such as incised, contusion, abrasion, etc.) and describes the three phases of healing: inflammatory, proliferative, and maturation. Additionally, it discusses complications of wound healing and factors that impair the healing process, particularly in older adults, emphasizing the importance of nutrition, blood flow, and immune response.