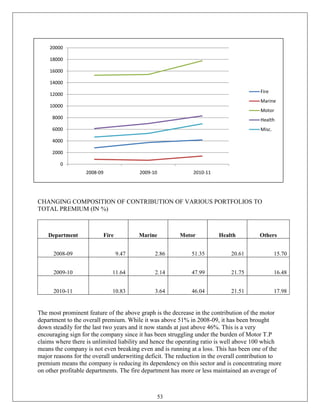
The document is a project report submitted by Anand Vinodkumar for his summer internship at New India Assurance Company Limited, fulfilling the requirements for a postgraduate diploma in management. It covers the evolution and competition within the Indian general insurance industry, detailing a 22% growth in premium income and highlighting the challenges of profitability amidst intense competition. The report combines industry analysis, company insights, and recommendations for improving profitability based on an internship experience and research findings.














![Pricing-
A fundamental principle of insurance pricing is that if insurers are to sell coverage willingly,
they must receive premiums that
( 1) are sufficient to fund their expected claim costs and administrative costs and
(2) provide an expected profit to compensate for the cost of obtaining the capital necessary to
support the sale of coverage."[Harrington 1999]
The pricing of insurance products starts from the pure premium calculation of the actuaries. It
includes the amount needed to cover expected losses and loss adjustment expenses. It is then
loaded for operating expenses including sales commission and other marketing costs, taxes and
the cost of handling claims. This component varies from one line of business to another. The law
of large numbers principle works while pricing a product i.e determining the premium. The
premium is based on rates. There are basically three recognized rating methods.
Judgment rating is used when the risk proposed to be bought is so unusual that little or no
statistical information about similar risk is available. Each exposure is individually evaluated,
and the rate is determined largely by the underwriter's judgment. When the judgment rating is
used, each premium is unique and is based on the opinion of the person making it.
Class rates are the most common rate in insurance business. Insured risks are classified on the
basis of one or several important features and all that belong to the same class are subject to the
same rate per unit of exposure. The rate charged reflects the claims experience for the class as a
whole. It is based on the assumption that future losses to insured will be determined largely by
the same set of factors.
Merit rating is a modification of the class rating. It modifies the class rate of a particular class
insured based on individual loss experience.
Promotion Strategy-
The aim of the company is to design the products from customer feedback to suit their specific
needs. The company focuses on delivering outcome rather than merely products. The company is
ramping up its knowledge database and is focusing on the customer base with a view to building
long term relationships. The role of field personnel is imperative for the promotion of the various
insurance covers and it is their responsibility to scout for these covers.
Electronic media, outdoor media and print media were utilized for publicity purpose. Hoardings
and glow signs were placed at many major road junctions, highways, railway stations and
airports. Advertisements were also displayed on transit media like buses, trains, baggage trolleys
and barricades.
Banner display at local events helped the company in brand building in rural areas.
The company participates in fairs, exhibitions and road shows and also sponsors various social
gatherings, sports and cultural events.
The company recently forayed into television and radio activities. The company also sponsored
the Mumbai Indians IPL T-20 team which has given tremendous visibility to the customers of all
ages and various groups not only nationwide but also global-wise.
The internet affords widespread access to a pool of new customers. Beyond the traditional means
of radio, print and television ads, the internet opens up the audience that insurers might reach.
This dimension has to do with delivering a marketing message to more customers than before.
Also the internet is an advertising vehicle. A website offers the insurer an opportunity to shape
20](https://image.slidesharecdn.com/sipreport-120508133046-phpapp01/85/SIP-report-20-320.jpg)