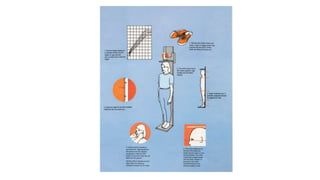
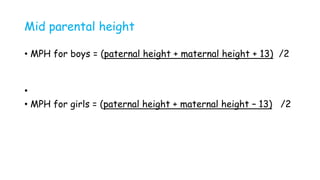
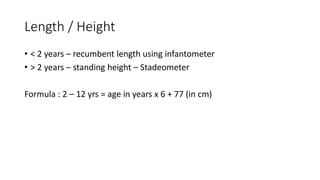
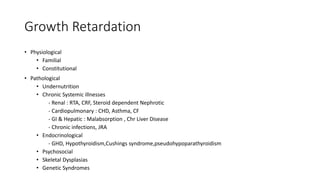
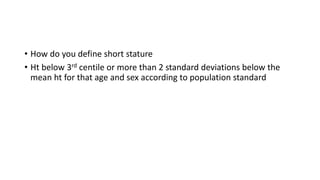
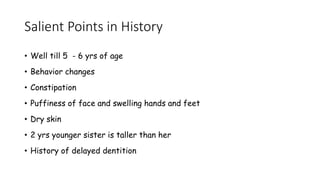
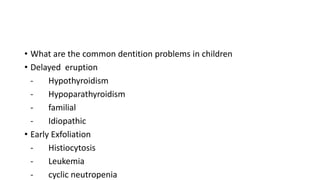
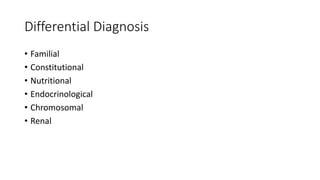
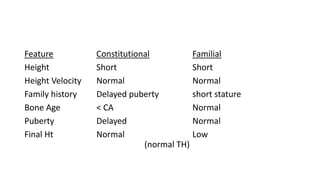
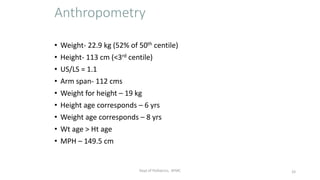
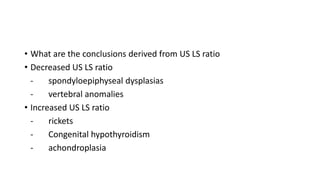
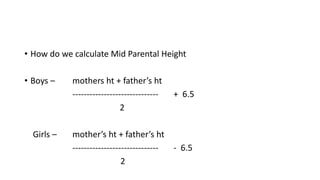
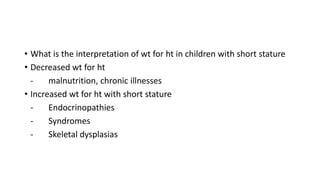
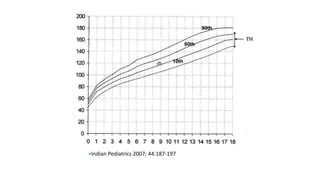
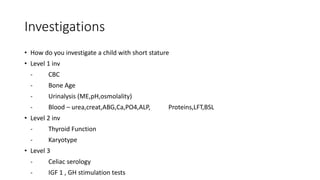
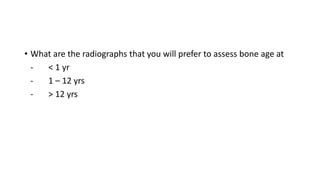
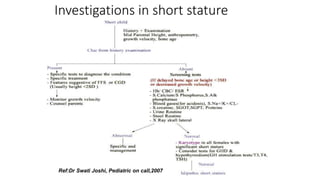
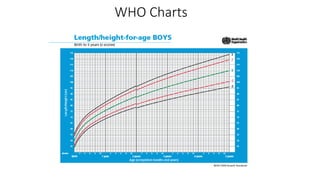
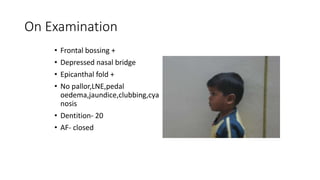
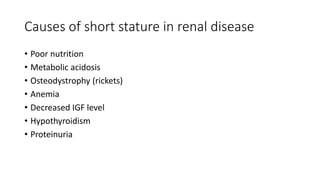
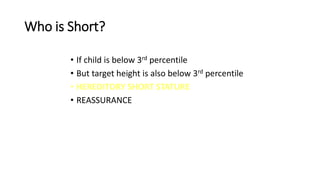
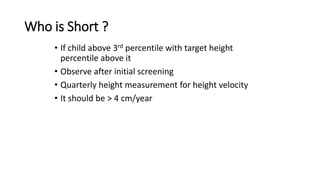
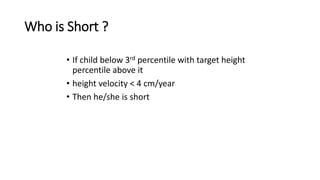
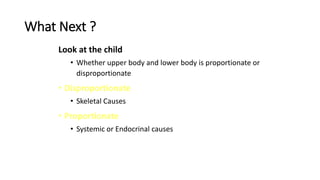
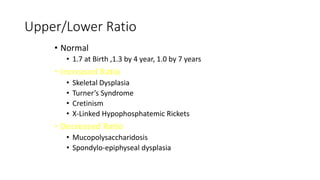
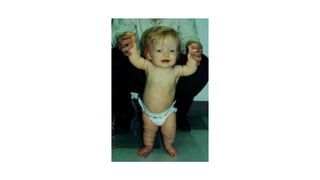
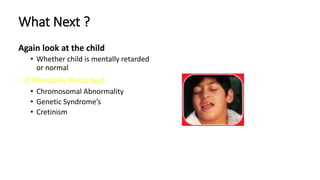
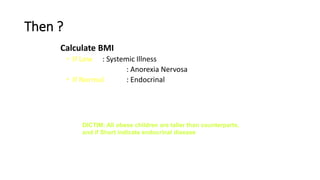
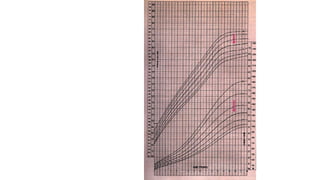
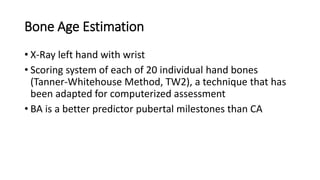
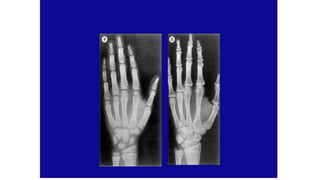
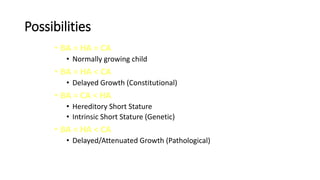
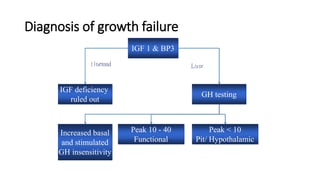
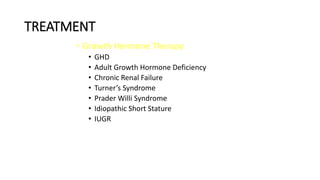
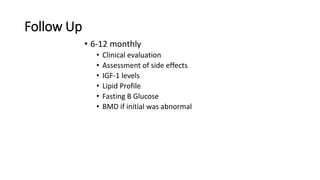
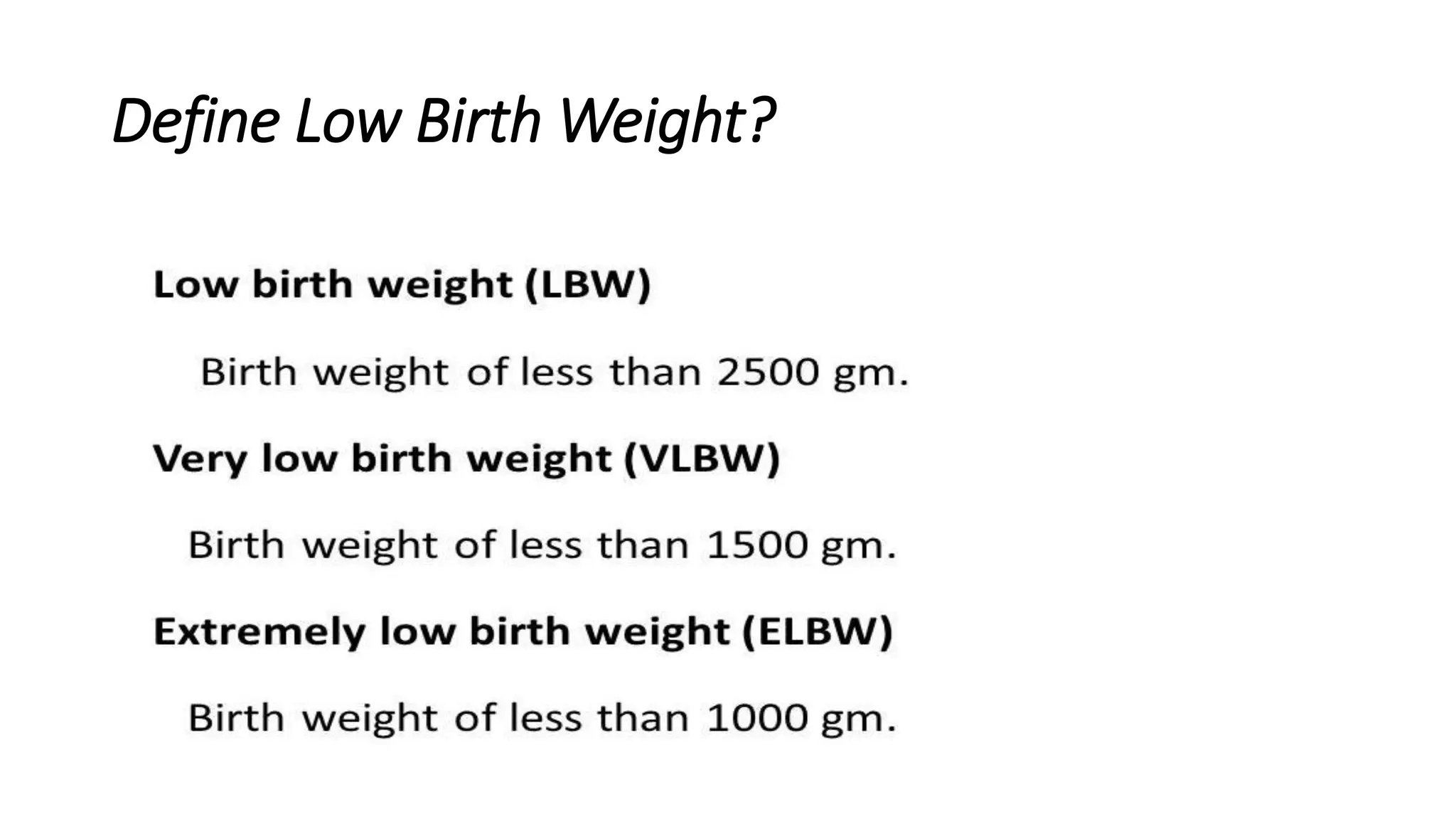
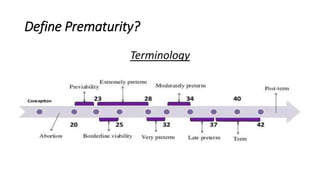
This document provides information on defining and interpreting various growth parameters in children, including low birth weight, prematurity, weight formulas, normal heights and head circumferences at different ages, mid-parental height calculation, and causes of growth retardation. It also discusses evaluating a child with short stature, including anthropometry, bone age assessment, differential diagnosis, and initial investigations. Key areas of focus are nutritional status, endocrine and systemic illnesses, skeletal dysplasias, and familial or constitutional growth patterns.
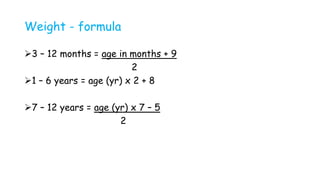
![Simple weight calculation
2-12 years = [Age (years)+3]x5 /2
7-12 years = Age(years)x3
2](https://image.slidesharecdn.com/shortstaure-231216055405-d9835078/85/Short-staure-Paeds-2-pptx-4-320.jpg)