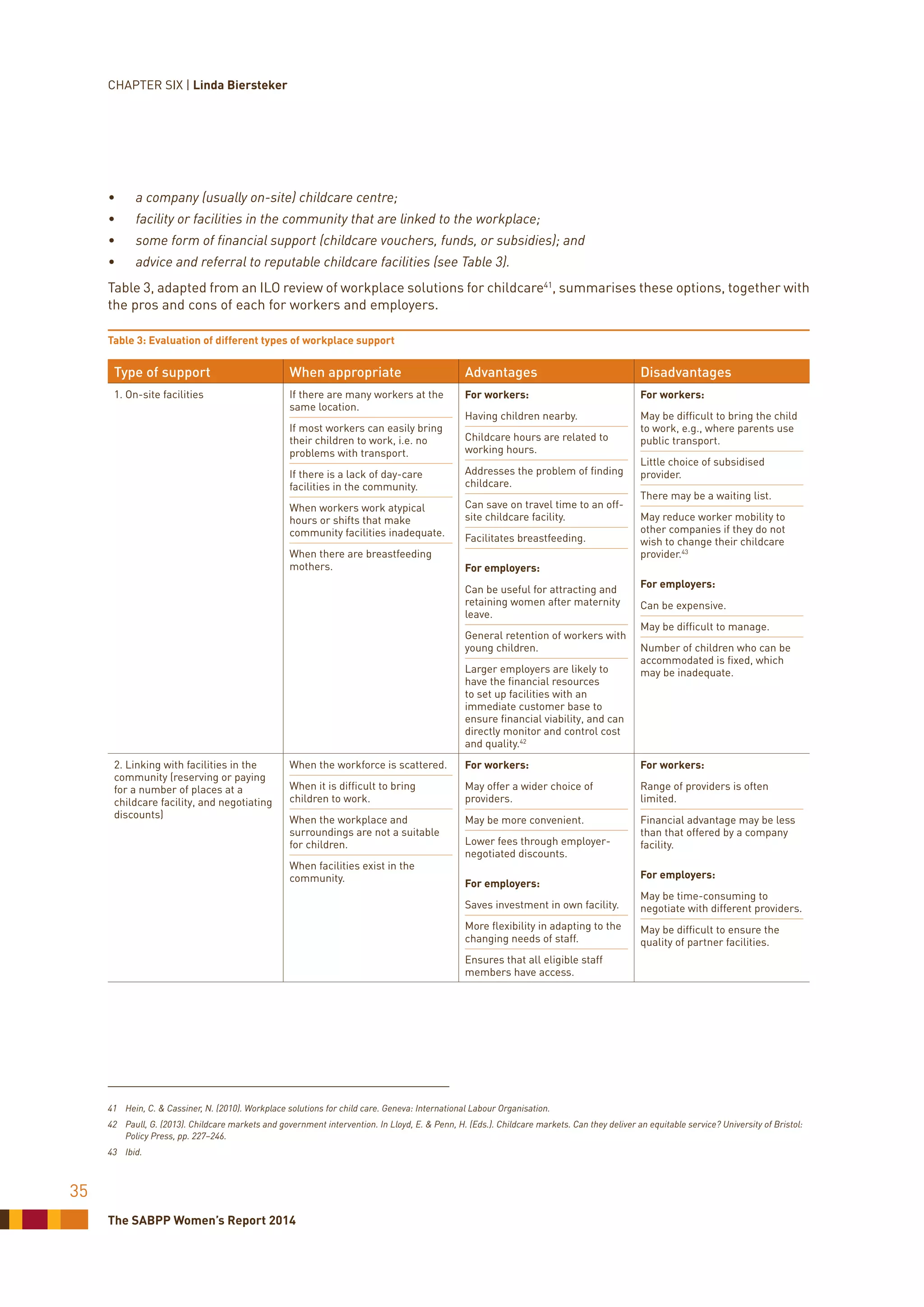
This chapter discusses how women's reproductive health and roles are often seen as "other" compared to the male norm in workplaces. Workplaces are typically structured around the "ideal worker" who is always available without responsibilities of childcare or pregnancy. While medical technologies now allow for options like delayed pregnancy, a woman's fertility declines sharply after age 35. Having children often means women are responsible for childcare, limiting their work and career opportunities. Better support for breastfeeding and childcare in workplaces could help create a more level playing field for women.
![South African Board for People Practices (SABPP)
Women’s Report 2014
Published and distributed by the SABPP
1st Floor, Rossouws Attorneys Building
8 Sherborne Road, Parktown
PO Box 2450, Houghton 2041, South Africa
T: +27 11 482 8595 F: +27 11 482 4830
E: hrri@sabpp.co.za www.sabpp.co.za
Copyright © 2014 SABPP and University of Johannesburg
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any
form or by any means, whether electronic or mechanical, photocopied or otherwise recorded or reproduced, without the
express, written permission of the copyright holders.
SABPP and the University of Johannesburg make every effort to ensure the accuracy of all the information (the “Content”)
contained in its publications. However, the SABPP, University of Johannesburg, and its agents and licensors make no
representation or warranties whatsoever as to the accuracy, completeness, or suitability for any purpose of the Content,
and disclaim all such representation and warranties, whether express or implied to the maximum extent permitted by
law. Any views expressed in this publication are the views of the authors, and are not necessarily the views of the Editor,
SABPP, or the University of Johannesburg.
Printed in South Africa, August 2014.
Other publications in the range: SABPP Women’s Reports 2011, 2012 and 2013.
How to reference information contained in this publication:
[Insert surname and initials of the chapter author]. (2014). [Insert the title of the chapter]. In A. Bosch (Ed.), South
African Board for People Practices Women’s Report 2014, pp. [insert page numbers of the chapter]. Parktown,
South Africa: SABPP.](https://image.slidesharecdn.com/womensreportsabpp2014-140809040935-phpapp02/75/SABPP-Women-s-Report-2014-2-2048.jpg)












![The SABPP Women’s Report 2014
17
The delicate balance between work and
becoming a single mother
Once the decision to proceed has been made, one of the
toughest challenges woman wanting to conceive alone
have to face is how to manage the process and not let
it impact on their work. It can be a lonely and private
journey, accompanied by feelings of uncertainty and
anxiety. These are feelings she might not want to share
at work, because of the nature of her position in the
workplace. This can further exacerbate these feelings
and emotions.
To help her through this process, the company’s human
resource practitioner should help her consider the
following points:
• Whether the woman’s relationships with her boss
and co-workers are amiable and supportive;
• What would she be prepared to reveal about her
individual situation?
• How would she cope with questions and comments
that will inevitably arise?
• Who would provide support at work?
• How will her treatment impact on her ability to
perform her job effectively?
• If she needs to be away from the office, is someone
available to cover for her?
Considering the above factors allows her to be proactive
in terms of developing a plan to walk the tightrope of
balancing the workplace and treatment. The human
resource practitioner needs to inform her of the
workplace’s protocols and policies in this regard, such
as time off, maternity benefits, and sick leave.
She needs to take into account that she works within the
context of an organisation with its own expectations and
demands. To retain her identity in the workplace, she
would need to adhere to these expectations in the same
manner as she did in the past.
Conclusion
The decision to become a single mother
by choice, in some ways, is seen as a
continuation of the changing norms for
women in our society today. “While their
achievements in the workplace became
a symbol of equality and progress, these
women did not give up on motherhood,
[one of] the oldest expectation and
centrally defining identity for woman.”16
Choosing to become a single mother can
enhance a woman’s perception of her
own identity, fulfilling the need to nurture
and care for a child, and opening areas
for growth that are vastly different from
those in the workplace.
16 Hertz, R (2006). Single By Chance, Mothers By Choice. Oxford University Press.
New York.
CHAPTER THREE | Bernice Lits and Tanya Rubin](https://image.slidesharecdn.com/womensreportsabpp2014-140809040935-phpapp02/75/SABPP-Women-s-Report-2014-20-2048.jpg)