Rational Antibiotic Therapy.pptx - Copy.ppt
- 1. RATIONAL ANTIBIOTIC THERAPY Dr S.KIRAN KUMAR, M.D.(ped) Assistant Professor SVIMS,SPMC(W)
- 2. OBJECTIVES To know what is irrational drug use Harms of irrational use What is rational prescribing Interventions needed for rational prescribing
- 3. Antibiotics are one of the most commonly prescribed drugs today. Rational use of antibiotics is extremely important as injudicious use can adversely affect the patient, cause emergence of antibiotic resistance and increase the cost of health care.
- 6. Antibiotic Era Antibiotics were hailed as “miracle drugs” after their initial introduction in 1940s. Penicillin, the wonder drug, saved millions of lives in the 2nd world war and many mothers were saved from puerperal sepsis. Their widespread availability and success led to such dramatic reduction in the morbidity and mortality caused by infectious diseases that many thought it was time to “close the book” on infectious diseases.
- 7. Introduction As if proving Darwin’s theory of “Survival of the fittest”, the bacteria underwent a rapid hitherto unprecedented evolution to circumvent this menace to their survival. Being single celled and endowed with the ability to multiply rapidly, the change was almost natural and spontaneous. RESISTANCE !!!
- 8. Antimicrobial Resistance (AMR) Indiscriminate use of antibiotics - the single most important factor responsible for the menace of AMR. Antibiotics are frequently prescribed for indications in which their use is not warranted, or an incorrect or suboptimal antibiotic is prescribed.
- 9. WHY WORRY about antibiotic misuse? Bacteria are increasingly becoming resistant to treatment with antibiotics. •There are no new antibiotics to fight the resistant bacteria. We are RE ENTERING a pre antibiotic era. •With a danger of losing the fight against infections to bacteria. We need to conserve antibiotics. •We need to use them rationally and Judiciously.
- 10. ANTIBIOTIC PARADIGM Excessive / inappropriate antibiotic use Failure of antibiotic treatment Antibiotic resistance
- 12. What is irrational use of antibiotics (IUA) ? IUA means use of wrong antibiotics, in wrong dose, by wrong route of administration, for wrong interval and duration and in wrong dosage form…
- 13. Determinants of irrational use of antibiotics On the part of pharmacist/dispenser ◦ Economic incentives ◦ Lack of regulations and enforcements ◦ Unclear role as health providers On the part of patients ◦ Lack of access to proper health care ◦ Beliefs and traditions ◦ Over the counter usage ◦ lack of public awareness about antibiotic misuse complications
- 14. Determinants of irrational use of antibiotics On the part of policymakers, regulators and pharmaceutical industry ◦ Lack of rational drug policy, regulations ◦ Uncontrolled marketing tactics ◦ Lack of infrastructure ◦ laxity of regulatory bodies in approval of antibiotics
- 15. Causes of irrational use of antibiotics Physician related Fear of secondary infection. Fear of missing serious bacterial infection,its dire consequences. Pressure from pharma industry. Fear of legal actions – many physicians prefer an error of commission to error of omission. Lack of investigation facilities. Mind set –prescription should have antibiotic
- 16. Consequences of Irrational use of antibiotics Antimicrobial resistance Adverse Drug Reactions Increased cost burden. Suppress but not control infection ,increased morbidity and risk of mortality.
- 17. What is Rational Use of Drugs? Requires that patients receive medicines appropriate to their clinical needs, in doses to meet individual requirements, for an adequate period of time, at the lowest cost to them and their community. (WHO 1985) Correct Drug; Correct Dose; Correct Duration !!!
- 18. General Principles Of Antimicrobial Therapy
- 19. Antibiotics are prescribed for Treating bacterial infections Prophylaxis of bacterial infections
- 20. Antibiotic Prescription Antibiotic prescription should ideally comprise of the following phases: ◦ Perception of need - is an antibiotic necessary? ◦ Choice of antibiotic – which is the most appropriate antibiotic? ◦ Choice of regimen : What dose, route, frequency and duration are needed? ◦ Monitoring efficacy : is the antibiotic effective?
- 21. Make a precise clinical diagnosis from the symptoms, signs and investigations e.g., in a case of pyogenic meningitis the diagnosis could be suspected as follows: ◦ Symptoms: Fever, irritability, altered sensorium, refusal of feeds, vomiting. ◦ Signs: Febrile, irritable child with altered sensorium, signs of raised intracranial tension, signs of meningeal irritation, variable neurological signs. ◦ Investigations: CSF examination, WBC count, sugar, protein, CSF culture. Consider possible etiologic agents - H. Influenzae, S. Pneumoniae, N, Meningitides rare. Target the most likely ones after consideration of age, h/o trauma, h/o neurosurgical procedure etc.
- 22. Specify the therapeutic objectives. ◦ Eradication of bacteria and sterilization of CSF at the earliest by use of bactericidal drugs • Clinical Cure • Prevention of relapse • Prevention of early and late complications, sequel and mortality. Consider the seriousness of illness. Make an inventory of effective group of drugs. Bactericidal agents penicillins, Chloramphenicol, 3rd generation cephalosporins, vancomycin etc.
- 23. Choose the most appropriate and effective group based on the criteria of efficacy, safety, suitability and cost. Choose an appropriate antibiotic from the chosen group. Decide route of administration, dosage schedule and standard prescribed duration. Write a legible prescription with name, age, sex, weight, diagnosis, drug's generic name, dose, route frequency and duration of treatment with other supportive drugs and treatment measures with signature and date.
- 24. Give relevant information, instructions and warnings. (Before food or after food, need for greater intake of water, alerting or danger signals of progression of infection and when to report again etc. Monitor and review the therapeutic response and choose an alternative in case of intolerance, allergy or other adverse drug reactions or poor in vivo response (midcourse correction).
- 25. Case 1 •5y Krishna •Fever 2 days •No other complaints •Clavam 1tsp BID •Temp 98.6 All infections are not bacterial – more often viral than bacterial Antibiotics are not antipyretics, let us respect them Fever the most common reason for prescribing antibiotics Antibiotics shouldn’t be started in hurry Confirm fever by thermometer Ac infections present with fever Some bacterial infections resolve without antibiotics Keep temp record Paracetamol Explain why is the child having fever Fever - a defence What to observe and when to follow up
- 26. Diagnosing Acute Bacterial Infection If few principles are strictly followed antibiotic misuse can be minimized to a great extent. Fever is the hallmark of acute bacterial infection and hence antibiotic therapy is not justified in any acute symptom that is unaccompanied with fever.
- 27. Exceptions : Neonate and shock state may be any exception to this rule. Fever may not represent every time an acute bacterial infection. Causes of fever Infection - Bacterial,viral,parasitic Non-infective - malignancy, collagen vascular disease, central fever, heat fever, drug fever
- 28. Approach to fever FEVER Is there a fever? Is there infection? Is it bacterial or viral ? Is there urgency to start antibiotic ?
- 29. Clinical differentiation between Viral infections Acute bacterial infections Sudden onset high fever Moderate onset Gets better by day 3 or day four Gradually increases and peaks on day three or 4. Comfortable not sick during interfebrile period Continues to be sick ever during interfebrile period Multi systems disseminated Tends to be localized Contact history+ Contact history +/-
- 30. It is important to realize that definitive diagnosis of acute bacterial infection is generally not possible for the first 2-3 days with the exception of tonsillitis, otitis media, acute lymphadenitis and bacillary dysentery.
- 31. Do no harm Harm ? •Diagnostic dilemma in partially treated meningitis Delay in diagnosis of a potentially fatal illness Adverse effect on outcome •Can have life long morbidity Fever • 1 y boy shiva • Fever 2 – 3days • Vomiting • Augmentin • Vomiting persists • Convulsion and referred • Fever ++ • Admitted • WBC – 18,400 • CSF – 102 cells, N 30
- 32. In absence of definitive diagnosis,serious bacterial infections (meningitis, pneumonia, diphtheria and sepsis ) MUST BE RULED OUT- as delay would result in poor outcome. In case of suspicion, appropriate tests and hospitalization are to be done prior to antibiotics therapy.
- 33. Every paediatrician must document absence of physical signs of these serious infections and observe further course of the febrile illness without antibiotic therapy.
- 34. If fever persists beyond three to four days without any localization one must consider urinary tract infection or typhoid fever. Its important to do relevant laboratory tests before instituting antibiotic therapy. Delay in starting an antibiotic by a day or two does not harm the patient.
- 35. Routine urine analysis may point to UTI and ideally urine culture must be done before starting treatment. It is important not to miss diagnosis of UTI as it may cause irreversible renal damage. Typhoid fever demands reasonable definite diagnosis as treatment has to be giver longer period to cure.
- 36. Diagnosing chronic bacterial infections Like tuberculosis, chronic UTI, sinusitis are not easily diagnosed clinically. These need investigations. There are not likely to worsen on the next few days, So there is enough time to confirm diagnosis then start antibiotics. Antibiotic trial is not rational here.
- 37. Antibiotics are also used for prophylaxis of bacterial infections in selective situations. It is important to strictly follow the standard protocols for prophylaxis for rational use. Routine prophylaxis by broad spectrum antibiotics is irrational and leads to development of drug resistant organisms. PROPHYLACTIC ANTIBIOTIC THERAPY
- 38. When can I use antibiotics empirically ? • Ac. Suppurative lymphadenopathy • Acute bacillary dysentery Clinically obvious bacterial infection • UTI on routine urinalysis • Clinical pneumonia Clinically probable bacterial infection but after sending the tests • Flu like illness which was improving, develops fever, creps • Measles develops fever during recovery Atypical progression of a viral infection
- 39. Empirical Antibiotic therapy Indications : Young infants < 3months of age with high fever. undiagnosed fever in an immunocompromised patient. Fever in patient in intensive care unit unaccounted fever in a child with heart defect probability of subacute bacterial endocarditis) are high risk situations for bacterial infections and should be treated with antibiotics but only after relevant investigations(CBC, Urinalysis, blood culture and chest X-ray) sent to laboratory.
- 40. Empirical use is based on personal observation and practical experience. Empirical use of antibiotics is scientifically acceptable if few prerequisites are judicially met with. Therefore, it should be an endeavour of every physician to justify antibiotic prescription in general and specially in case of empirical use.
- 41. Choice of Antibiotic Most of the community-acquired infections would respond to almost any antibiotics. It is important to choose an antibiotic, which has low potential to develop resistance such as amoxicillin for oral use or cefotaxime for parenteral use.
- 42. Route : Oral drug is always preferred unless patients condition demands use of parenteral drug. In such a case, antibiotic available with both formulations may be the best choice, So that one could shift to oral therapy with same drug, once patients condition stabilizes. Change from one parenteral drug to another is not ideal.
- 43. In stable conditions, there would always be time available to monitor response to an antibiotic and hence choice of antibiotic should be restricted to first line of drugs. First line of antibiotics is adequate for most of the common community acquired infections and other antibiotics should be reserved for specific usage such as nosocomical infections.
- 44. Broad-spectrum antibiotics are not best for the simple community acquired infections and infact ,narrow-spectrum antibiotics hits the organism the hardest.
- 45. What’s the harm ? (In giving antibiotics) Fever • 6 y, boy sagar • Fever 5 days • Amox- clav , no response • Cefixime • Better for 2 -3 days • Fever again • Cefixime and falcigo • No response in 3 days • Ciplox • Finally referred • Investigations delayed Partial response misleads • Delay in diagnosis Interferes with proper interpretation of tests • TB, Leukemia, KD, SOJIA, SLE Commonly missed or delayed •Investigations - ALL
- 46. CHANGE OF ANTIBIOTIC In case of failure of anticipated response, change of antibiotic may be considered after adequate trial for 3-4days. Second antibiotic must be rationally chosen, as it should widen the bacterial cover beyond that offered by the first antibiotic. If second antibiotic fails, it is best to review the diagnosis. Invariably wrong diagnosis is the cause of antibiotic failure and not the drug itself.
- 47. Addition of another antibiotic when the first one fails is not rational in acute bacterial infection. If first one has failed, it should be replaced.
- 48. COMBINATION ANTIBIOTIC THERAPY It is irrational to use two antibiotics for a single infection. It may be necessary only in selective situations. Rationality of combination -constituents act by different mechanisms -pharmacokinetics-almost same -targets organisms causing a single disease -no supra-additive toxicity
- 50. When to use combination therapy - Life-threatening conditions - Mixed infections - To prevent drug resistance development. - True synergistic combinations
- 51. Case Fever • 10 y girl Padmini • High Fever 1 day • Cefixime 1 ½ tsp BD x 3 d • Chloroquine 1tspBD x 3 days Practice Pearls Don’t use poly therapy – antimalarial and antibiotic Don’t use antimalarial without definite diagnosis irrational use of Chloroquine over the time has led to resistance to chloroquine Let us use new antimalarial judiciously Paracetamol and counseling Try and differentiate viral from bacterial Wait for it to evolve if there are no red flags Ask to keep temp. record
- 52. Common complaints for which antibiotics are prescribed FEVER Cough cold fever Fever loose motions vomiting dysentery Cough fever difficulty in breathing Skin infections cellulitis boils ABSCESS, Impetigo
- 53. Case 4 year old Anusha LM and vomiting since a day Watery motions and passing adequate urine Febrile, no dehydration Which of the following will you prescribe ? Normetrogyl Taxim O Ciplox TZ Lomotil None Practice Pearls Most diarrheas in under 5 are viral Amebic dysentery is Extremely uncommon (< 2%) • ORS to prevent and correct dehydration • Oral Zinc for 14 days • (20mg in >6m, 10mg in <6m) Rational treatment
- 54. ORS remains the mainstay of therapy during acute diarrhea and zinc as an adjunct as an additional modest benefit in reducing the stool volume and duration of diarrhea.
- 55. 10 month old Vani, brought with Illness 2 days Started with vomiting 6-7/day Fever Frequency of stool 12-15/day, watery, large quantity On BF + Weaning diet Case - Vani
- 56. Ill look Depressed AF Dry skin and mucous membrane Sunken eyeballs Rapid, low volume pulse How will you manage? Vani on examination....
- 57. Child with Acute Diarrhea Watery Diarrhea without blood in stool Diarrhea with macroscopic blood in stool in stool Diarrhea with Systemic infection Assess dehydration Severe dehydration Mild to moderate dehydration IV fluids ORS(10) Zinc (11) Continued frequent feeding - including BF ORS (10) Zinc (11) Continued frequent feeding - including BF Pallor, Purpura, Oliguria Hosptalise No antibiotics
- 58. Antimicrobial drugs are not required for routine treatment of acute diarrhea because most episodes are caused by pathogens for which antimicrobial drugs are not effective. Etiology of acute diarrhea Pathogen incedence Rotavirus 25-30% Enterotoxigenic E.coli (ETEC) 20% Shigella 5-10% Enteropathogenic E. Coli (EPEC), Locally adherent E.coli Campylobacter,salmonella 5-7% G.lambia, E.histolytica <2% V. Cholerae 5-10%
- 59. When should Antimicrobials be given for acute diarrhea ? The only specific clinical indications for use of antimicrobial agents where they have been found useful include : • Suspected cholera with severe dehydration • Blood diarrhea (probably shigellosis) • Seriousness associated non gastrointestinal infections. e.g. Pneumonia, septicemia, meningitis, urinary tract infection etc.
- 60. Anti diarrheal Agents Motility suppressants decrease intestinal peristalsis and delay the elimination of causative organisms. Their use in infants can be particularly dangerous causing paralytic ileus respiratory depression abdominal distension bacterial overgrowth and sepsis.
- 61. Combination therapy Several combinations of antibacterial agents and of antibacterials with antidiarrheals are available. They offer no extra benefits. Combination therapy can promote over growth of harmful resistant bacteria and the anti motility agents that are often a part of delay excretion of invasive pathogens.
- 62. Probiotics Insufficient evidence to recommend probiotics in the treatment of acute diarrhea.
- 63. Enteric fever is an important cause of morbidity .Resistance in salmonella is very dynamic and changes with changing patterns of drug use Empirical therapy is started in clinically suspected but cultures not sent, or results not available or culture negative. It is important to send blood cultures so that diagnosis is unequivocal,antimicrobial susceptibility of isolate and local resistance patterns will be available.
- 64. SITUATION Local susceptibility patterns FIRST LINE 2ND LINE SEVERE ILLNESS/ INPATIENT/ COMPLICATION S High prevalence of nalidixic acid resistance and Low prevalence CEFTRIAXONE (75-100 mg/kg/day-BD- IV)- Cefotaxime, Aztreonam, Ampicillin, chloramphenicol OUTPATIENT THERAPY of resistance to amp/chloram/ cotrimox CEFIXIME(15- 20 mg/kg/day) AZITHROMYCI N(10- 20mg/kg/day)- 5-7 days chloramphenicol Amoxicillin Cotrimoxozole High dose quinolones Duration- 14 DAYS ,course may be completed with oral third generation cephalosporins once complications resolved and oral intake is satisfactory.
- 65. Frank Tally, the chief scientific officer of Cubist Pharmaceuticals who played a major role in bringing cefixime
- 66. Combination therapy not recommended. When failure to respond,if blood cultures positive –check antimicrobial susceptibility and modify drug acc,. Look for –coinfections ,complications phlebitis, drug fever, hemophagocytic syndrome Relapse-right dose for right duration.
- 67. Fever and cold, cough • 1yr Shiva • High fever 2 days • Cold, cough 2 days • What will you use? • Cefixime • Amox-clav • Clav pod • None Remember Most of the URI seen in OPDs are viral Symptomatic treatment •Counseling •Self limiting nature of the illness •Signs to observe for fu
- 68. Case • 3 ½ yr old girl renuka • Cough cold and fever 2 days • Mother says this is the 4th episode in last 5 months and he gets better only with antibiotics • Every episode for 2 -3 days, child doing well otherwise Up to 6 episodes/yr of URI not uncommon in a healthy child “Child better with antibiotics” and not because of antibiotics”
- 69. Most upper respiratory tract infections are viral and do not merit antibiotics. Antibiotics do not prevent bacterial superinfection. Antibiotics are indicated for acute bacterial sinusitis,ASOM and streptococcal sore throat. Amoxicillin is the drug of choice for all ; In severe or non responsive sinusitis and otitis media coamoxiclav may be used. Third generation cephalosporin's should be used sparingly.
- 70. RHINOSINUSITIS Symptoms : Nasal/post nasal discharge Daytime cough for more than 10days less than 30 days. Temperature of 102 Fahrenheit. Purulent nasal discharge for 3 to 4 consecutive days.
- 71. Acute sinusitis Antibiotics first line Treatment failure 48- 72hrs Non severe Amoxycillin (45mg/kg/day BD) Co-amoxiclav Severe Coamoxiclav (30-40mg/kg/day TID) Ceftriaxone (75mg/kg/day for 3days) For patients who are allergic to amoxicillin, Cefdinir Cefuroxime Cefopodoxine In cases of serious allergic reactions, Clarithromiycin Azithromycin.
- 72. Case 1: sagar sagar 2 yrs old male, Brought with history of fever and cough with rhinorrhoea of two days red eyes, diarrhea, No exanthema, cough ++ H/o Similar case in family O/E Throat congested How will you manage? Your thoughts……………
- 73. Clinically diagnosed : Viral URI - seasonal (pharyngotonsillitis) Management: ◦ General & Symptomatic Therapy ◦ Antibiotics : Not needed
- 74. 41/2 year old Sai - brought to your clinic with 2 days history of high spiking fever and mild cough From history and examination: Has no red eyes or rhinorrhea No exanthema Difficulty in swallowing, No history of similar case in the family He looks sick even when afebrile 2nd Case: Sai
- 75. Sai on examination…… RR 28, HR 110 perfusion and B.P normal Rt tonsil showed a purulent discharge with inflammation of both tonsils Bilateral tender cervical LN++ Ear and Nose – Normal Other system examination – normal How will you manage?......
- 76. sagar and Sai– what difference? sagar Acute onset, Red eyes, rhinorrhea, cough++, diarrhea No rashes Pharyngeal congestion but no or scanty exudates and no cervical lymphadenopathy Age less than 3 years Most probably viral Sai Acute onset, throat pain, rapid progression, very little cough/cold Pharyngeal congestion more, thick exudates or follicles, purulent patchy lesions on tonsils with tender enlarged LN Toxicity ++ Age more than 3 years Most probably bacterial
- 77. PHARYNGITIS causes Viral Bacterial Rhinovirus Strep pyogenes(15-20%) Coronavirus gpC/G strep Adenovirus N gonorrhoea HSV Corynbackterium diphheriae Parainfluenza Arcannobacterium haemolyticum Influenza Mycoplasma coxasackie virus C pneumoniae EBV Yersinia enterocolitica Group A B haemoglytic streptococcal pharyngitis is the only commonly occuring form of ba Pharyngitis for which antibiotic therapy is definitely indicated.
- 78. GABHS Conjunctivitis, Cough, Coryza, Viral exanthema Fever higher than 100f, Tonsillar swelling or excudates, Tender cervial lymphadenopathy, Absence of cough Viral pharyngitis Symptomatic treatment. Response No response bacterial Antibiotics
- 79. Case 3: murali murali, a 15 month otherwise healthy boy had rhinorrhea, cough and fever of 1020F for two days On day 3, he became fussy and woke up crying multiple times at night WHAT COULD BE WRONG? HOW DOES ONE EVALUATE THIS CHILD ?
- 80. MURALI HAS ACUTE OTITIS MEDIA RIGHT EAR On examination of Rt ear: Erythema Fluid Impaired mobility Acute symptoms MANAGEMENT ?
- 81. Management AOM – Under 2 Yrs Analgesia ◦ Paracetamol in adequate doses as good as Ibuprofen Antibiotics in divided doses for 10 days ◦ Choice - first line Amoxycillin / Co- amoxyclav ◦ Second line Second generation cephalosporins e.g. Cefaclor, cefuroxime. Co amoxyclav – if not used earlier Decongestants no role
- 82. ACUTE OTITIS MEDIA AOM is defined as presence of middle ear effusion plus the presence of symptoms or sign. It can be with perforation or without perforation. Indications for Antibiotics. •Children less than 2yrs with bilateral AOM. •Children >2y with severe infection. •Children who have AOM with perforation. •Children at high risk of complication. •Children who didn't improve after 48 hrs of watchful waiting.
- 83. AcuteOtitisMedia Antibiotics first line Treatment failure 48- 72hrs Non severe Amoxycillin(45mg/kg/ day BD) coamoxiclav Severe Coamoxiclav(30- 40mg/kg/day TID) Ceftriaxone(75mg/kg/ day for 3days)
- 84. Case • 7 month Madhu • Fever, cough and rapid breathing x 2 days • Febrile, RR 66/m • Nasal flaring, grunt, Crepts+ • What is it ? Severe pneumonia What is recommended ? Refer to Pediatrician
- 85. Pneumonia is the leading cause of mortality and common cause of morbidity in children below five years of age. In developing countries bacterial infections are the most common cause of pneumonia ,streptococcus pneumoniae and hemophilus influenzae being common bacterial pathogens identified. Administration of appropriate antibiotics in the early course of pneumonia alters the outcome of illness
- 86. In view of better outcome of pneumonia by early administration of antibiotics and inability to clinically differentiate between bacterial and viral pneumonia, antibiotics are administered to all children with pneumonia.
- 87. Treatment for pneumonia Treat a severe pneumonia Below 3 months Above 3months severe 3m to 5y Co amoxiclav if no response amoxicillin Amoxicillin +/- Azithro Refer for hospitalization Non severe Above 5yrs
- 88. Treatment of pneumonia Children less than 3 months: Hospitalized- intravenous antibiotics 3rd gen cephalosporins and aminoglycoside.
- 89. DISEASE PNEUMONIA Setting DOMICILLARY- ORAL Age First line Second line Suspected staphylococcal disease 3mo to 5y of age Amoxycillin Cotrimoxazole Co-amoxy Clavulanic acid Cefuroxime Cefpodoxime Cefdinir Amoxycillin + Cefuroxime Co-amoxy Clavulanic acid 5y plus Amoxycillin Macrolide Co-amoxy Amoxycillin + Cefuroxime Co-amoxy Clavulanic acid cloxacillin
- 90. DISEASE SEVERE PNEUMONIA Setting IN PATIENT -INTRAVENOUS Age First line Second line Suspected staphylococcal disease 3mo to 5y of age Inj ampicillin Inj co-amoxy Clavulanic acid Inj ceforoxime Inj co-amoxy Clavulanic acid Inj 3rd gen cephalosporins Cefotaxime/ceftriaxone Inj 3rd gen cephalosporins Cefotaxime/ceftriaxone + Cloxacillin inj cefuroxime Inj co-amoxy Clavulanic acid Secondline : vancomycin/teicoplanin +inj 3rd gen cephalosporins 5y plus Inj ampicillin Inj co-amoxy Clavulanic acid Macrolides Inj co-amoxy Clavulanic acid Inj 3rd gen cephalosporins Cefotaxime/ceftriaxone Macrolides Inj 3rd gen cephalosporins Cefotaxime/ceftriaxone + Cloxacillin inj cefuroxime
- 91. Fever in infants Need for urgent investigations for acute bacterial infection. Consider UTI,pneumonia,meningitis before specific therapy Treatment without diagnosis leads to complications with permanent sequelae
- 92. RED FLAGS Age <3 months Not able to to drink or feed Lethargic or unconcious Respiratory distress Convulsions Sick looking when afebrile present absent Observe and record temperature Use only paracetamol Rule out serious illness Look for localization Reasses and investigagate HOSPITALISATIO N
- 93. Don’t miss UTI UTI is a common cause of fever in children Antibiotic without ruling out UTI may lead to partial or incomplete treatment and renal scarring Urinalysis and Culture essential before Abx case • ganesh 4y, is a k/c/asthma on inhaled salbutamol and budesonide • Fever with chills x 2d • No cough cold • Given Amoxicillin • Urine R – 18-20 pc/hpf Urinary symptoms may not be there in young children Think of UTI in all cases of FWF
- 94. For suspected severe acute UTI- antimicrobial therapy should be started immediately after urine culture is sent.
- 95. Treatment Therapy should be prompt to reduce the morbidity of infection, minimize renal damage subsequent complications. Indications for hospitalization- For IV rehydration and IV Antibiotic therapy in Children who are dehydrated, are vomiting, are unable to drink fluids, Less than 3 months of age, With complicated UTI
- 96. The choice of antibiotic should be guided by local sensitivity patterns. A third generation cephalosporin is preferred. Therapy with a single daily dose of an aminoglycoside may be used in children with normal renal function. Intravenous therapy is given for the first 2-3 days followed by oral antibiotics once the clinical condition improves.
- 97. Antimicrobial treatment Medication Dose , mg/kg/day PARENTERAL Ceftriaxone 75-100,in 1-2 divided doses iv Cefotaxime 100-150,in 2-3 divided doses Amikacin 10-15,single dose iv or im Gentamicin 5-6,single dose iv or im coamoxiclav 30-35 of amoxicillin,in 2 divided doses iv
- 98. Children with simple UTI and those above 3 months of age are treated with oral antibiotics. With adequate therapy, there is resolution of fever and reduction of symptoms by 48- 72 hours. Failure to respond may be due to presence of resistant pathogens, complicating factors or noncompliance; these patients require reevaluation.
- 99. ORAL Medication Dose , mg/kg/day oral Cefixime 8-10,in 2 divided doses Coamoxiclav 30-35 of amoxicillin,in 2 divided doses Ciprofloxacin 10-20,in 2 divided doses Ofloxacin 15-20,in 2 divided doses Cephalexin 50-70,in 2-3 divided doses
- 100. The duration of therapy -14 days for infants and children with complicated UTI - 7-10 days for uncomplicated UTI. • Following the treatment of the UTI, prophylactic antibiotic therapy is initiated in children below 1 year of age, until appropriate imaging of the urinary tract is completed.
- 101. Newborn with fever Practice Pearls • Well looking neonate with fever can have serious bacterial infections Document fever • Environmental or dehydration fever is a diagnosis by exclusion Never give antibiotics without proper work up Seek pediatrician’s opinion Case • 15 d baby of aruna • Fever x 2 days • Baby looks well • What antibiotic ? • Amxo clav • Inj Gentamycin • Cefixime • Referred to pediatrician • Critical and in ICU
- 102. WHAT WE CAN DO ????? DONT LISTEN, I wanna grow
- 103. Problem of drug resistance is a result of our own wrong doing and before the situation gets out of control, we need to act seriously. Following Protocols and guidelines formulated by an official scientific organization will help in rational use of antibiotics ,would serve the community best and also protect physicians from legal hassles.
- 104. Every physician should document probable diagnosis and basis for such a diagnosis before writing a prescription. Fostering awareness about antimicrobial resistance and rational antibiotic practice is to be done which is a part of the IAP ICMR call to action declared this year-2014.And it is ACTION time now!
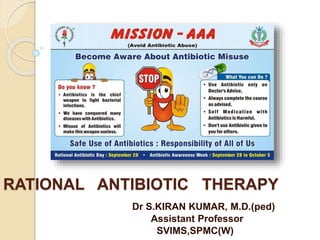
- 106. As a commitment to reduce antibiotic misuse, September 28 will be observed as Rational Antibiotic Day and the week (Sep 28 – Oct 4) as Antibiotic Awareness Week. September 28 has been selected in commemoration with Sir Alexander Fleming's discovery of penicillin. Awareness campaigns, rallies, talks in media, webinars, and sensitizing the family practioners on rational antibiotic practices through lecture, CMEs to be done.
- 108. EMERGING AND RE EMERGING INFECTIOUS DISEASES The theme of the world health day – april 7 ,1997 “EMERGING INFECTIOUS DISEASES-GLOBAL ALERT:GLOBAL RESPONSE”
- 109. “The Chennai Declaration” “A Roadmap to Tackle the Challenge of Antimicrobial Resistance - A Joint meeting of Medical Societies in India” was at Chennai on 24th August. This was the first ever meeting of medical societies in India on issue of tackling antimicrobial resistance. We had representatives from most medical societies in India, eminent policy makers from both central and state governments, representatives of WHO, National Accreditation Board of Hospitals, MCI Drug Controller General of India, and ICMR along with well-known dignitaries in the Indian medical field. The meeting consisted of interactive discussion sessions designed to seek experience and views from a large range of health care professionals and included six international experts who shared action plans in their respective regions. The intention was to gain a broad consensus and range
- 110. WHO ADVOCATES 12 KEY INTERVENTIONS TO PROMOTE MORE RATIONAL USE Establishment of a multidisciplinary national body to coordinate policies on medicine use Use of clinical guidelines Development and use of national essentional medicines list Establishment of drug and therapeutics committees in districts and hospitals Inclusion of problem based pharmacotherapy training training in undergraduate curricula
- 111. Continuing in service medical education as a licensure requirement Supervision , audit and feedback Use of independent information on medicines Public education about medicines Avoidance of perverse financial incentives Use of appropriate enforced regulation Suffficient govt expenditure to ensure availability of medicines and staff
- 112. Antibiotic Stewardship Restricting the usage of antibiotics Restricting use of broad spectrum antibiotics Surveillance and auditing of cultures Protocol of antibiotic prescription Infection control committee Improving infection control practices
- 113. Surveillance and Audit Surveillance culture from the unit Audit of processes - Hand hygiene, IV cannulation, procedures - Usage of disinfectants - Availability of disinfectants Audit of cultures - Type of organisms (EOS and LOS) - Sensitivity pattern - 1st line, 2nd line empiric antibiotics
- 115. Educating Consumers No own antibiotic kit Emphasis on dose and duration No self medication
- 116. TAKE HOME MESSAGE
- 117. Golden rules for Judicious use of antimicrobials Golden rule 1 Acute infection always presents with fever; in acute illness, absence of fever does not justify antibiotic Golden rule 2 Infection is the most common cause of fever in office practice, though not always bacterial infection - Viral infection in majority RTI - Viral infection should not be treated with antibiotic
- 118. Golden rule 3 Clinical differentiation is possible between bacterial and viral infection most of the times • Viral infection is disseminated throughout the system (URTI / LRTI) - May affect multiple systems - Fever is usually high at onset, settles by D3-4 - Child is comfortable and not sick during inter febrile state • Bacterial infection is localized to one part of the system (acute tonsillitis does not present with running nose or chest signs) - Fever is generally moderate at the onset and peaks by D3-4 • CBC does not differentiate between acute bacterial and viral infection
- 119. Golden rule 4 Chronic infection may not be associated with fever and diagnosis can be difficult - Relevant laboratory tests are necessary - Antibiotic is considered only after observing progress - There is no need to hurry through antibiotic prescription
- 120. Golden rule 5 Choose single oral antibiotic, either covering suspected gram positive or negative organism, as per site of infection and age of patient • Combination of two antibiotics is justified only in serious bacterial infection without proof of specific organism and can be administered intravenously
- 121. Golden rule 6 At first visit (within 48 hrs of fever) antibiotic is justified only if bacterial infection is clinically certain and that does not call for any tests prior to starting the drug (Acute tonsillitis / acute otitis media / bacillary dysentery / acute suppurative lymphadenitis) • If bacterial infection is clinically strongly suspected but should have confirmative tests prior to starting drug, then order relevant tests and start appropriate antibiotic (Acute UTI) • In absence of clinical clue but not suspected to be serious disease, observe without antibiotic and follow the
- 122. R-Reasoning behind prescription > > - Right dose, route, duration > > A-Academically updated decisions > > T-Training of mind (3 ‘O’s-Organ, Organism, Option) > > -Training of subordinates (Resident doctors etc.) > > -Training parents (not to pressurize the doctor) > > -Training chemists (to refrain from selling without valid prescription) > > I-Instructions to parents > > (reconstitution, administration, completing the course, not to self medicate)
- 123. O-Organism > > ( finding out the causative organism by culture etc.) N-Noting down the diagnosis > > (if you clinically diagnose & write provisional diagnosis as viral, your hands should shake while writing an antibiotic) A-Avoiding double standards > > ( writing one in private OPD , using a different one in a general hospital and speaking totally different in conferences) > > -Avoiding irrational combinations > > -Antibiotic Policy L- Local sensitivity pattern > > (includes our active efforts & research in office practice) E-Ethical considerations > > -Economic condition of the patient
- 124. REFERENCES IAP- ANTIMICROBIAL THERAPY 2013 GUIDELINES Mission:avoid antibiotic abuse-vijay n yewale IAP- vol 51-june15 2014 GUIDELINES Optimize use of antibiotics in nicu- srinivas mukri Prescribing antibiotics in pediatrics-raju shah Antimicrobial resistance-ghafur
- 125. Iap-vol 16 jul-sep 2014 recent advancs in pediatrics –anupam sachdev Rational antibiotic therapy – dr.vijay yewale Rational drug therapy-vikas dua,anupam sachdev
- 126. Thank You !!!