The document provides an overview of the male and female reproductive systems, including definitions of key terms related to puberty, menstruation, and reproductive development. It describes the anatomical structures and functions of the male and female reproductive organs, highlighting their roles in reproduction and hormonal regulation. The document emphasizes the complexity of reproductive processes, from gamete production to fertilization and gestation.
















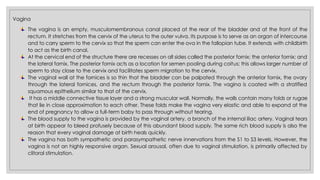


![Hypothalamus
(synthesize and release)
Gonadotropin-releasing Hormone
(GnRH)
(triggers)
Anterior pituitary
(release)
Luteinizing Hormone
Follicle-stimulating Hormone
[Gonadotropin Hormones]
(triggers)
Ovarian Follicle
Excrete high level of Estrogen
Development of the uterus, fallopian tubes,
and vagina; typical female fat distribution;
hair patterns; breast development; also
closes the epiphyses of long bones.
The Role of Estrogen
The start of breast
development is referred
to as thelarche, which
typically starts 1 to 2
years before
menstruation.](https://image.slidesharecdn.com/p3-reproductive1-250120003626-d7cd3d83/85/POWERPOINT-REPRODUCTIVE-SYSTEM-22-320.jpg)

