Physio noteliilbnkljklj;ihlihilgilgilylihlihilguk
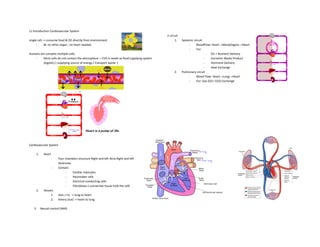
- 1. L1 Introduction Cardiovascular System single cell -> consume food & O2 directly from environment - Bc no other organ , no heart needed Humans are complex multiple cells. - Most cells do not contact the atmosphere. = CVS is needs as food supplying system (logistic) ( supplying source of energy / transport waste ) Cardiovascular System 1. Heart - Four chambers structure Right and left Atria Right and left Ventricles - Contain: - Cardiac myocytes - Pacemaker cells - Electrical conducting cells - Fibroblasts ( connective tissue hold the cell) 2. Vessels 1. Vein ( in) -> lung to heart 2. Artery (out) -> heart to lung 3. Neural control (ANS) 2 circuit 1. Systemic circuit - BloodFlow: Heart→ManyOrgans→Heart - For: - O2 + Nutrient Delivery - Excretion Waste Product - Hormone Delivery - Heat Exchange 2. Pulmonary circuit - Blood Flow: Heart→Lung→Heart - For: Gas (O2+ CO2) Exchange
- 2. EVOLUTION OF CIRCULATORY SYSTEM Circulation in Animals sponges & cnidarians Invertebrates flatworms & other platyhelminthes short distance for nutrients to diffuse to the outer cell layer. have either a gastrovascular cavity or a circulatory system for internal transport. ( use water ) no cell is >a few mm away from the body surface. Open Circulatory System Closed Circulatory System ● Hemolymph acts as both blood and interstitial fluid ● Relaxation of the heart draws hemolymph into the vessel. ● Insects, arthropods,mollusks • Blood is in vessels and interstitial fluid is present • Heart (or hearts) pumps blood into large vessels • Major vessels branch into smaller ones which supply blood to organs • In the organs, materials are exchanged between the blood and the interstitial fluid bathing the cells. • Annelids and vertebrates Open - blood can go out to tissue Closed - cannot
- 3. Fish: 2-Chambered Heart Amphibians & Reptile : 3-Chambered Heart Birds & Mammals : 4-Chambered Heart - start to have atrium & ventricle - Only 1 circuit - As blood flows through a capillary bed, blood pressure drops substantially - Blood flow to the tissues and back to the heart is aided by swimming motions. - Two atria and One ventricle - Blood flows in a double circulation scheme through: 1. Pulmonary circuit (to lungs and skin) 2. Systemic circuit (to all other organs) - Blood flow pattern: ventricle→lungs & skin→left atrium→ventricle→all other organs→right atrium - Double circulation: 1. systemic circulation 2. pulmonary circulation - Complete septum = no mixing of oxygenated & deoxygenated blood - Separation greatly increases the efficiency of O2 delivery to the cells mix blood -> not enough O2 supply Both amp & reptile = not enough energy /can’t do work long [ tired easily] Crocodile -> 4 chamber
- 4. Cardiac muscles - Heart is the origin of pressure in the circulatory system - Pressure in the heart is generated by contraction of cardiac muscles CARDIOMYOCYTES - Components : - Sarcomere ( contractile unit ) - Thick filament ( myosin) - Thin filament ( actin) - Cardiac vs skeletal m. - Skeletal m. - multi- nucleus work as single unit - Myocytes fuse together called myofibril. - Cardiac muscle - single cell -> 1 cell 1 nucleus - Myocytes are working separately. - Myocytes talk via gap junction (intercalated disc) - The difference in cellular arrangement leads to variation in stimulating contraction. EXCITATION-CONTRACTION COUPLING - SKELETAL MUSCLE 1. Ach release from n. Terminal ( neuromuscular junction) to m. 2. action potential is generated and propagates along the sarcolemma and into the transverse tubules. 3. The voltage sensor DHPR ( voltage-sensitive protein ) detects the depolarization of sarcolemma (action potential) - DHPR is physically linked to RYR ( a calcium release channel located on the sarcoplasmic reticulum) 3. When the DHPR sensed the depolarization, DHPR conformational change triggered the opening of RYR to release Ca 2+ stored in SR into the sarcoplasm. 4. The released Ca2+ then binds to troponin on thin filaments in the sarcomere , moves the tropomyosin away from the myosin-binding site on actin, permitting cross-bridge cycle initiation muscle contraction. 4. Removal of Ca 2+ from the cytoplasm by Ca 2+ ATPase results in the recovery of tropomyosin to its blocked position and relaxation occurs.
- 5. - CARDIAC MUSCLE - Cardiomyocyte Contraction is triggered by electrical signals from neighboring myocytes. - one direction (No reverse) - Electrical Conduction ( cell-to-cell signal) via Gap Junction (Intercalated disc) - Gap Junction composed : - two hexametric connexons. - Major connexon protein “Connexin43”. Intracellular Ca2+ and Force of Contraction Ca2+-binding to Troponin C⬆️ actin-myosin interaction⬆️ force of contraction⬆️ - At rest our heart used only 25 of available Ca2+ to get 50% of force contraction. The rest of them are needed when the body needs more pumps. Q: During Exercise, cardiac muscle cells contract stronger. Does the number of contracting cells increase from resting? Ans: No, every cell in the heart contracts every time but with a small force. Skeletal m. can increase the # of cell to contract stronger Regulation of intracellular Ca2+ 1. Extracellular Ca2+ concentration 2. L-type Ca2+ channel opening (permeability) ⬆️ 3. Ryanodine receptor opening (permeability) ⬆️ 4. SR Ca2+ available - SR Ca2+ reuptake (rate)⬆️ - SERCA/phospholamban ⬆️ - Rate of Ca2+ detach from troponin C⬆️ 5. Mitochondria Ca2+ turnover Sympathetic stimulation ( faster heartbeat )= ⬆️
- 6. Excitation-contraction coupling (ECC) for cardiac contration - mechanical changes of electrical signal to chemical and then to mechanical action. 1. Opening of Na+(funny) channels. 2. Na+ ions enter, MP in the AV nodal cell ( peace maker) depolarizes, activating T-type Ca2++ channel 3. activating L-type Ca2+ channels leading to the sustained depolarization 4. Ions then travel through gap junctions to the contractile cells 5. influencing the opening of Na+ channels, allowing Na+ to enter, depolarizing the cell, and reaching the threshold-> action potential initiated 6. K+ channels are activated once the membrane potential reaches a positive value / AP, allowing K+ to move out, resulting in hyperpolarization. 7. As the action potential propagates along the sarcolemma and reaches the T-tubules, it activates the L-type Calcium channel in T-tubules - Hyperpolarization ( and as K+ moves out) leads to the opening of L-type Ca2+ channels, Ca2+ moves in to maintain electrochemical balance (Net = 0). 8. The influx of calcium through L-type channels opens RYR-2 and triggers the release of additional calcium from SR initiating muscle contraction. ** CA2+ induced CA2+ release 9. Excess Ca++ is then transported back into the SR -> muscle relaxation - calcium release and reuptake allows the heart to contract and relax in a coordinated manner with each heartbeat
- 7. VASCULAR SYSTEM / Blood Vessels Artery Capillary Vein Blood vessels that take blood away from the heart to one or more parts of the body. [Aorta > Large artery > Small artery > arteriole] Small blood vessels located in the tissue. blood vessels that carry blood from part of the body towards the heart. Thick Wall Single layer Wall Endothelium Thinner Wall High Pressure Low Pressure Low Pressure Low Compliance - high compliance ( ability to expand) Low Capacitance Solvent & Solute Exchanging Valves Cardiovascular-Neuronal Coordination Abnormalities of cardiovascular system - Heart Diseases - Vascular Disorders Signs and Symptoms – Fatigue or tiredness / Weakness – Dizziness or lightheadedness – Rapid heartbeat ( tachycardia ) -> heart prob. – Shortness of breath – High ( vascular disorder ) / low ( heart disease) blood pressure at rest
- 8. Human Cardiovascular Parameters At Rest **memorize** - Heart rate: 60-70 beat/min - Cardiac output: 5-6 Liters/min (Amount of blood passes through the heart /min. - BP: 120 and 80 mmHg (Pressure in the artery at highest and lowest points) *Each parameter will change during exercise. BLOOD - Volume: 7% of body weight - 55% of blood is “plasma” and 45% is red blood cells (Depending on gender and age) Plasma - Composition: water, Na+, Cl-, K+, proteins, antibodies, vitamins, hormones, gasses. - Protein: Albumin, Globulin, Fibrinogen RBC ( Erythrocyte) - no nuclear , 7 micron in diameter - Production : - location : Bone marrow, - stimulation: Erythropoietin ( prod. From kidney) - Even no erythropoietin -> Red blood cells are turnover 1% each day - Age: 120 days - Major component: Hemoglobin - Function: Carry O2, CO2 and Buffering Hemoglobin - Effective respiratory pigment in most animals - Fe2+ porphyrin compound (heme group) and protein (globin ; varies in different species ) - 4 heme groups & carry 4 O2 Abnormality of Red Blood cells Anemia - # RBC lower than normal. - Prob. W/ hemoglobin protein Signs and Symptoms - Fatigue / Weakness - pale skin - Dizziness / lightheadedness - Rapid heartbeat ( tachycardia ) - Shortness of breath
- 9. L2 Cardiac Electrophysiology 1. Describe the sequence of ionic currents throughout the action potential of cardiac myocytes. - Excitable cell characteristic: - electrochemical gradients btw intracellular & extracellular. - bc plasma membrane permeability - PM has many specific ion channels. - allow ions moving between intracell & extracell change MP - Ion Channels = membrane proteins as gates between inside & outside of the cell. - ( do not open all the time; most are specific) - Na+, Cl- and Ca2+ -> extracellular = want to move in - K+ -> intracellular = want to move out - At rest MP = -70 : - K+ channels have higher permeability ( always open ) - Na+, Cl- and Ca2+ channels closed. Membrane potential - If Na+ channels are only opened. - move in until equilibrium ( Na+ in=out ) - equilibrium potential represents the “Membrane potential” of the cell during Na+ channel open. - MP = + 62 mV - Positive value = +Ion Outside < Inside - If the cell opens only K+ channels. - move out until equilibrium. - MP = - 80 mV - Negative value = +Ion Outside > Inside “However, one cell is permeable not only 1 ion.” Question: Q1 : Why does Ca2+ influx need during phase 2, which is not needed in muscle or nerve AP? - Ca2+ influx induces Ca2+ releases from sarcoplasmic reticulum (SR) to further activate myofilament contraction. Q2: Where do neighboring cells get the electrical signal? - From SA node via gap junction 2. Describe the sequence of ionic currents throughout the action potential of cardiac pacemaker cell (SA-nodal cell). Action Potential - self- regenerating wave of electrochemical activity by changing the membrane permeability to the specific ions - 2 Mj phase - Depo & repolarize Compared the AP of nerve and cardiac myocyte Conductance = amount of ion movement (influx or efflux)
- 10. 4 phase: 4 ( Resting phase) : - [Inward Rectifier] K+ channels open, K+ slowly efflux.[ -90 mV ] 0 (Depolarization phase): - Fast Na+ channels open, Na+ largely influx [ -90 mV to almost +20 mV ] 1 (Early repolarization phase) : - More [Transient outward] K+ channels open, more K+ efflux. [ +20 mV to 0 mV ] 2 (Plateau phase): - [Delay Rectified slow] K+ channels and [L-type] Ca2+ channels open, K+ efflux is equal to Ca2+ influx. [ 0 to > 0 mV ] 3 (Repolarization phase) : - Only K+ channels open ( Delay Rectified rapid and slow , Inward Rectified ) , more K+ efflux. [ 0 to -90 mV ] Diastolic Phase ( restoration to resting state ) : - Active Na+ - K+ Pump , efflux 3 Na+ exchange of 2 K+ influx Refractory Period - it won’t be stimulated in a period of time - underlies by Inactive fast Na+ channels
- 11. How does a pacemaker cell generate its own action potential? - pacemaker cell in SA node gen. Electrical signal @ highest signal frequency. - Many cells can generate electrical signals by themselves as well. - Electrical impulse from the SA node spreads out from the right atrium→left atrium→atrio-ventricular node (AV) and→ventricular septum→ventricular walls consequently. - If right atrium damaged = pacemaker damage -> heart go slow Excitability of Nodal Cells Action Potential of Sino-Atrial Node (Nodal cell / cardiac pacemaker cells ) - Slow Response Action Potential Phase 4: Non-stable Resting membrane potential / slow diastolic depolarization Phase 0: Depolarization Phase Phase 3: Repolarization Phase IK: K+ efflux early of phase 4 & phase 3 [ slow rate ] If: funny current ; Na+ or Ca2+ influx phase 4 - Funny channel activated ( NA+ move in ) - If occurs when membrane become hyperpolarization -60/-70 mV ICa(T): Ca2+ transiently influx at the end of phase 4 ICa(L): Ca2+ largely influx causing active depolarization or phase 0 - L type Ca2+ channel activated after the MP reach threshold
- 12. 3. Compare and contrast ionic currents of action potential between cardiac myocytes and cardiac pacemaker cells. Similarities - Na+ influx = Depolarization - K+ Efflux = Repolarization Differences - Cardiac Myocytes: - Rely on electrical signals from neighboring cells - Fast Na+ channel open, Na+ largely influx during depolarization phase - L-type Ca2+ channel plays a significant role in plateau phase ( K+ efflux is equal to Ca2+ influx ) - True resting phase and true diastolic phase - 7 ion channels [ Fast Na+ channel , 4 type of K+ channel ( Delay Rectified rapid and slow (2) , Inward Rectified , Transient outward), L-type Ca2+ channel] - Cardiac pacemaker cells - Automaticity via funny current contributing spontaneous depolarization - Have T type Ca2+channel contribute to depolarization phase ( opening of L type Ca2+ channel ) - non-stable resting membrane potential due to ongoing slow diastolic depolarization - 4 ion channels [ Funny channel , Ca2+ channel ( L and T type ) , K+ channel ] Sympathetic ( fast ) and Parasympathetic ( slow current ) activation on Nodal cell Parasympathetic (Ach): - Hyperpolarization - Decreased phase 4 slope - Causing more time to reach threshold of phase 0 Sympathetic (Adrenergic): - Increased phase 4 slope - Causing short time to reach threshold of phase 0
- 13. 4. Describe electrical conduction along heart Heart contract by itself: 1. Once action potential is initiated in the sinoatrial node 2. It is propagated between atrial cells via gap junctions, as well as through specialized conduction fibers in the atria. [ Atrial myocardium ] 3. it pass through the atrioventricular node to reach the ventricle 4. pass throughout the ventricle via the bundle of His [ AV bundle & branches ] and the Purkinje system / network ) and gap junctions in the intercalated disks of adjacent cardiac myocytes. [ Ventricular myocardium ] Action potential of Pacemaker Cell & Physiological Heart Rate - Intrinsic property of the pacemaker cell at SA node has an AP frequency about 100 times/min. - At rest (no activity) there is parasympathetic activation to the heart that suppresses the heart rate to be 60- 70 times/min - During exercise - parasym activation shut down - sympathetic activation ⬆️ - Heart Rate ⬆️accordance with the degree of sympathetic Action Potential Propagation - There are 2 types of AP in the heart, the AP of each cell is not exactly similar. - They vary in degree and duration in order to have proper contraction of the whole heart.
- 14. L3 Electrocardiography (ECG) 1. Explain the basic concept of electrocardiography (ECG) - ECG Measurement - Many electrodes will be placed on skin in specific locations Electrodes ( locations ) • 3 Standard limb leads - basic ECG recording. - potential difference measured between skin of arm and leg. • 3 Augmented leads • 6 Chest leads [more precise ] Basic concept: - P wave = atrial depolarization - QRS = ventricular depolarization - T wave = ventricular repolarization - Atrial repolarization could not be seen because it overlaps with ventricular depolarization but smaller amplitude. Q: Why does the wave of ventricular repolarization have the same direction of ventricular depolarization? - Concept of depolarize first repolarize last creating the potential difference. repolarize slower = lesser amplitude
- 16. 3. For ECG, explain the action or phase of the heart in the following intervals and segments: RR-interval, PR-interval, QT-interval and ST-segment. RR-interval ( R wave to another R peak ) - One complete cardiac cycle (atrial and ventricular depolarization and repolarization) PR-interval ( Duration between the start of P wave to the start of QRS complex ) - P wave = atrial depolarization ( from SA node to right atrium and Left atrium) - Depolarization spread from SA node to right atrium ( follow lead II direction) causing the potential different generating a small positive rise - When both atrium depolarizes ( Right to left atrium), the potential difference becomes zero resulting in a downward curve. - The current then passes through the AV node ( depolarization of the AV node ) to give a flatline on the ECG graph. QT-interval ( Duration between the start of QRS to the end of T wave) - Entire ventricular activity - [ QRS = ventricular depolarization , T wave = ventricular repolarization ] - The current from the AV node moves along the bundle of his ,on the septum. Though the left branch has a faster rate of conduction than the right branch, the muscle on the right is very thin so it depolarizes faster than the left side resulting in current to oppose the Lead II so the ECG graph falls a little bit negative. - The ECG graph then significantly increased due to the potential difference of endocardium and epicardium. The wall endocardium wall depolarizes first making the potential different to be at peak as the epicardium is not yet depolarized. However ,as the epicardium starts to depolarize from endocardium, the potential difference starts to be lesser resulting in the downward trend of the ECG graph. Once both ventricles depolarize, the line falls to zero. - The current then moves from the apex to the base ,with the anatomical structure of the heart, there is a little curve on the edge between left atrium and ventricle so the current reverse as it goes from the left to the right make the ECG graph line lower than the baseline. ST-segment ( end of QRS wave to the start of T wave) - All ventricular myocardium is depolarized so there is no potential difference given flatt line on the ECG graph
- 17. 2. Discuss the common pathological finding by ECG measurement ECG interpretation - Higher amplitude -> higher depolarization which is a result of higher mass [cell / muscle tissue ] (Hypertrophy). [ Heart become bigger ] - Prolonged P-Q interval = delay electrical conduction from atrium to ventricle (AV-block) - Reversed QRS means the axis of the ventricle moving away from the normal axis. (e.g. Hydro-pericardium) -> ภาวะกล ้ามเนื้อหัวใจบวม ** prolong action potential = blockage of Ca2+ [ งูกัด ] 4. How does tachycardia affect the heart contraction and relaxation? Tachyarrhythmia - Fast heart rate , Irregular heart rhythms and often exceeding the normal range with a ventricular rate of 100 or more per minutes - Shorten Time for contraction ( systole) and relaxation ( diastole ) phase - Resulting: - Low pressure develop in left ventricle - Low blood ejection from the heart - Low arterial blood pressure - Low tissue blood supply - Non- synchronized heart contraction between atrium and ventricles. - Atrial flutter - Fast P wave ( high rate ) , loss of consequent QRS - Rapid contraction in atrium ( left or right ) prevent the chamber filling blood completely - Atrial contraction may not followed by ventricular contraction - Atrial Fibrillation - Similar to atrial flutter but beat Irregularly showing irregular small fast wave ( high rate ) , loss of consequent QRS - Irregular rapid contraction of atrium - Atrial contraction may not followed by ventricular contraction - Ventricular Tachycardia - Ventricles generate their own fasting signals without follow signals from the atrium or SA node, no P wave is seen. - Ventricular Fibrillation - Irregular QRS , no P wave is seen
- 18. L4 HEMODYNAMICS 1. Discuss the relationship between pressure gradient, fluid flow, and resistance to flow Flow= Movement of particle from high energy state to low energy state Bernoulli’s theory - Pressure energy: Pressure - Potential energy: Gravitational energy - supine position = no g energy - standing position Heart need to pump more blood ( pressure ) against gravity Giraffe ( head far from heart ) -> heart needs to pump more p. - Kinetic energy: Energy moving mass
- 19. 2. Describe factors determining the blood flow in terms of the Poiseuille’s equation Hemodynamics ⬆️length & Viscosity -> ⬆️# of attaching each other & wall surface -> ⬆️Increases in fiction Q: Among these three factors affecting vascular resistance, which factor plays the highest or least physiological effectiveness? Why? Highest: r bc power of 4 Least : length bc when ppl grew up the length is constant Summary: Hw: Does Anemia affect blood flow? 3. Explain the properties of the vascular wall and ventricular wall on internal pressure. Radius ( most important factor determining resistance.) Mechanisms helping blood flow in small vessel 1. High Capillary Area ( ⬇️P , ⬆️P distribution) 2. Parallel circuit arrangement - ( ⬆️branches = ⬇️total resistance flow) 3. Low viscosity in small vessel (capillary) -> go faster r ⬇️viscosity ⬇️= faster rate
- 20. Pattern of blood flow ( * remember factor effect pattern flow ) 1. Lanmina : all molec in same direct , most same speed 2. Turbulent : blood from very small r ( expand ) Properties of Tubular Wall 1. Circulatory Pressure - Internal pressure - External pressure - Circumference tension - force that counteracts the difference between internal and external pressure. What is the effect of high wall tension? - if tension > wall strength = break - ANEURYSM ( no need to remember name ) - High wall tension causes high risk of vascular rupture. - - Q: How much does the vessel handle the high wall tension?
- 21. 1. Wall compliance ( ability to expand ) Distribution of blood
- 22. L5 cardiodynamic Heart gen pressure like piston pump Ventricular contraction [ vital role in contraction ] Rt. = Lt. Ventricular Contraction Blood ejects from ventricles to aorta or pulmonary artery Ventricular Relaxation Blood flows back from vein and atria to ventricles. 1. Define the cardiac cycle and describe its events. Explain the contractile events underlying pressure generation. Cardiac cycle [ remember what open/close in what phase ] H P -> L P
- 23. What BP in the RV < LV - Bc Left ventricle supply blood to the whole body - Right ventricle has a thinner m. wall thickness and it supply to the lung 2. Explain the relationship between ventricular pressure and ventricular volume This relationship can be described by using a pressure-volume loop. During diastole, the opening of the mitral valve initiates ventricular filling, leading to a gradual rise in both volume and pressure. The transition to isovolumic contraction occurs when the mitral valve is closed, marking the start of systole. During isovolumic contraction, ventricular volume remains constant while pressure steadily rises to the optimal point for ejection. As systole progresses, the aortic valve opens, allowing blood to be ejected into the aorta. This phase is characterized by a continuous rise in pressure as volume decreases due to blood ejection. At the peak of systole, pressure begins to decline as the heart continues to contract, and the aortic valve eventually closes. The ensuing isovolumic relaxation phase sees a significant drop in pressure while ventricular volume remains constant, completing the loop and preparing for the next cardiac cycle.
- 24. Q: Does the pressure-volume curve always the same ? - NO ; changes in various conditions such as under exercise or hypertension conditions - example 1. Increase preload: Increased atrial pressure leads to more blood filling into the ventricle (= Increase EDV) 2. Increased muscle contraction leads to higher pressure in the ventricle, so more blood is injected out (= decrease ESV). 3. Increase afterload
- 25. 3. Discuss the determinants of cardiac stroke volume and heart rate. - Blood flow is determined by pressure gradient - Flow (Q)∝P(A) – P(B) - To keep constant blood flow, Body must maintain high pressure at Aorta - How gen. Pressure at aorta? - Heart muscle contraction squeezes blood in the heart chamber to the arterial system making high pressure in the aorta. - CO = amount of blood ejecting out of the heart per minute - SV = amount of ejecting blood per beat - VR = amount of blood turning back to the heart. - ABP ⬆️CO ⬆️ - CO = HR x SV = VR - CO at resting state in adult = 5-6 L/min - CO changes during exercise and is exciting. - How does CO change? - ANS: 1. Symp ->. ⬆️HR 2. Parasymp -> ⬇️HR 3. Cathecholamines -> ⬆️HR - HR created by pacemaker cell @ SA node - Freq of pacemaker AP determine HR - SV = EDV - ESV - EDV [ End Diastolic vol] = How much in ( vol beginning ) = Amt of blood in ventricle just bf systole Factor affecting EDV: 1. Venous Return ⬆️( VP ⬆️) - Change in VP is a major determinant of VR ⬆️ 2. Filling time ⬇️(Diastolic period) ( ⬆️1/HR) - Increased HR will decrease the diastolic time and then decreased filling time. 3. Heart distensibility (cardiac compliance) - Ability to expand without change in pressure influences flow. When is blood filling stopped? - Blood flow into the heart is dependent on the pressure gradient between venous pressure and pressure in the heart chamber. - Blood filling stops when pressure in the ventricle is overpressure in the atria or vena cava. - This pressure in the heart is a factor called “Preload” *Resistance in the pulmonary system is relatively low, so the effect of pulmonary circulation in a normal heart is generally ignored. - ESV = How much blood left after ejection (End Systolic vol ] Factor affecting ESV 1. Contraction Force ⬆️ESV ⬇️ 2. Pressure in Aorta ⬆️ESV ⬆️[ Difficult to eject ] - Aortic pressure counteracts the blood ejection. 3. Valvular Stenosis ESV ⬆️[ Valve can’t open / difficult to open ] - Similar to aortic pressure, stenosis causes high resistance to flow. When is blood ejection stopped? - Stopped when pressure in the ventricle is lower aortic pressure - Then the pressure in the aortic is a factor that known as “Afterload” - Afterload = pressure that drain fluid out of the heart
- 26. Contraction Force ( systole ) Cardiac muscle generally increase the force contraction by two mechanisms 1. Heterometric Autoregulation [ various length ] = the automatic mechanism that enhances in force contraction when preload (EVD) increases. - The underlying mechanism is the Frank- Starling mechanism. - Increased blood volume (EDV) in the heart chamber will stretch the muscle fibril to the better length for actin-myosin interaction. - Length-tension relationship 2. Homeometric Regulation / Contractility mechanism [ same length ] = the mechanism that directly increases the number of actin- myosin interaction without change in sarcomere length. - The underlying mechanism is by increasing the Ca2+ bind to the regulatory protein on the myofilament (troponin complex). - Mechanism that activates in intracellular Ca2+ activation is sympathetic stimulation. - * no parasym for cardiac m. - At resting condition, Ca2+ used for contraction just only 25% of total Ca2+ in sarcoplasmic reticulum Summary: - Pressure in the cardiovascular system is generated by the heart. - Many mechanisms contribute to maintaining proper cardiac output. - Many factors include factors inside of the heart (contractility) as well as factors from outside of the heart (preload/afterload). - Since CO generates arterial pressure, what happens to the arterial pressure during diastole (No blood ejection)? 4. Discuss the determinant of mean arterial pressure.
- 27. L6 Vascular physiology Components of cardiovascular system Vascular Pressure [ No P = No blood flow ] **** Heart generates Pressure, Vessel then maintains Pressure!!!* 1. Discuss the basic relationship between cardiac output ( CO ), systemic arterial pressure ( ABP ) and total peripheral resistance ( TPR ) - blood flows easily in the vessel = no blood left over and arterial pressure will drop. - flow difficult = more blood remaining in the artery, and keeps high arterial pressure to drive blood flow - Vessel resistance ( peripheral resistance ) ⬆️ABP ⬆️ CO ⬆️; TPR = total peripheral resistance “ ABP CO • TPR ” ∝
- 28. 2. Discuss the relationship between stroke volume, pulse pressure, and vascular compliance. Compliance - Each v.v. -> different ability to handle pressure. - determined by volume-pressure relationship - adding fluid in a tube, pressure will increase. ** a. Has low compliance -> P remains @high lv. Driving energy in a. - P is a driving F exerted against the wall of v.v. 1. Hydrostatic Energy 2. Dissipation Force ( friction energy) [ some energy loss ] 3. Recoil Force ( rebound ; energy ) Arterial recoil - What is significant? - Prevent pressure in aorta from dropping to fast - If drop fast -> ⬇️blood flow to tissue = only get blood during systole - If no recoil force -> pattern of arterial P will follow LVP - Occur during diastolic phase causing a rebound of arterial vessel - The spring back of v.v make pressure in artery inducing blood flow - *** Arterial recoil makes continuous flow of blood all through systolic and diastolic phase.
- 29. Factor affecting arterial pressure - Systolic pressure ⬆️Amount of blood in the vessel during systole⬆️: - VP determines SV ⬆️; SP ⬆️ - Diastolic pressure ⬆️ Amount of blood in the vessel during diastole ⬆️ - TPR determines how easy blood can flow out, while elastic recoil generates the pressure. - (*Systolic pressure will determine recoil energy*) - TPR ⬆️DP ⬆️ Arteriole: a resistance vessel - Arteriole vessels have effective smooth muscle. - tonic contraction and relaxation in order to control resistance and consequently blood flow. - Contraction or relaxation is dependent on tissue and body requirements. SUMMARY Arterial Functions: • Deliver blood throughout the entire body. • Maintain the pressure by using compliance/recoil and controlling total peripheral resistance. • Total peripheral resistance is regulated by vasoconstriction/ dilation of arterioles. • Constriction/Dilation is regulated by vascular smooth muscles • Blood pressure is varied by the amount of blood in the artery as well as compliance. Regulation of Arterial blood flow / Controlling system of Arteriole resistance 1. Neural and hormonal factors [ Extrinsic control ] - Effecting site: Vascular smooth muscle ( contraction / relaxation ) 2. (local) Metabolic factors [Intrinsic control] 3. Myogenic ( autoregulation ) factor [Intrinsic control] 4. Physical ( external ) factors [Intrinsic control] - Extravascular compression - Systole : myocardial compression ( squeezed effect ) on coronary artery - Very few blood flows into the coronary a. = can't pass and supply heart - Diastole: no compression = flow very high; easy to supply heart
- 30. L7 Common Heart Disease 1. Explain common causes of heart failure and its consequences. Heart failure = inability to produce cardiac output CO = HR x SV Changes result: HR : Rhythmic -> Arrhythmia ( Rhythm abnormal ) SV: 1. Systolic Dysfunction - ⅔ HF patients - Decrease Myocardial contraction ability - This leads to an inadequate ejection of the blood to tissue. - Cause: 1. Myocardial Ischemia & Infarction - Complete obstruction ( > 20 min ) [ destruction of blood supply myocardial ] -> Irreversible cell death - Infarction -> deposit of many Collagen [ lost of m. cell ] 2. Infection & Myocarditis - Virus : Coxsackie B virus , Adenovirus, SARS-COV2 - Spirochete : Borrelia burgdorferi ( lyme disease ) - Protozoa : Trypanosoma 3. Toxicity - Chronic Alcohol Abuse - Anti-cancer drug - cocaine 2. Diastolic Dysfunction -> This leads to the decrease in ventricular compliance. - ⅓ HF patients - Decrease in Ventricular relaxation and blood filling ability - Cause: heart or other 1. Extra-myocardial Abnormality - Mitral Valve Defect - Pericardial Diseases - Pericardial sac around heart ( effect the expansion of the heart during relaxation) - Low Blood Volume (Severe Hemorrhage) - Low blood return to heart 2. Myocardial Abnormality - Myocardial Infarction [ too much scar ; heart can’t expand ] - Infiltration Disease: Amyloidosis, Sarcoidosis - Chemical that deposit to the cardiac tissue - Effect the expansion of lt. ventricle - Cardiac Hypertrophy (wall thickening→reduced compliance) - Acute Ischemia (reduced blood supply = reduced ATP→ Rigor [ can’t expand ] + No SR Ca2+ reuptake) - Cardiac m. contract stiffly w/o relax Myocardial Ischemia & Infarction Loss of blood supply to the heart cause→Oxygen shorten →Cell Death Risk factors: - Old age - Tobacco - Diabetes - High Cholesterol ( plaque obstruct ) - Hypertension - Alcohol Consumption ( vascular func ) - Cocaine & Methamphetamine - High chronic stress - Male > Female Myocardial Infarction -> Common ECG Defects - Elevation / Depression of ST segment - It occurs due to some pt. Of ventricle do not depolarization during ST segment
- 31. Valvular Disorders - mostly found congenital - also found in adults ( most occur on lt. Side of heart ) - Valvular stenosis ( valve open narrow & blood cannot flow normal ) - Aortic stenosis -> SV ⬇️CO ⬇️mABP⬇️ - the aortic valve narrows and blood cannot flow normally. - Mitral stenosis -> EDV ⬇️SV ⬇️CO ⬇️mABP⬇️ - Valvular insufficiency (regurgitation) [ not close completely ] - Aortic insufficiency - blood in the aorta return to the left ventricle during diastole ( fine during systole) - the ventricle must accommodate not only the blood returning from the body but also the blood leaking back from the aorta. - EDV⬆️ESV ⬆️CO ⬇️mABP ⬇️ - Reduced CO as some blood return back = less blood flow to tissue - Mitral insufficiency - blood in the Lt. Ventricle return to Lt. atrium - SV ⬇️CO ⬇️mABP⬇️ -
- 32. 2. Explain characteristics of cardiac hypertrophy and its cause. Cardiac hypertrophy ( increase in cell size) = a cellular response of the heart to physiological insult Classified into 2 concept Anatomical Hypertrophy Patho-physiological Hypertrophy 1. Concentric ( ventricle thick ) 2. Eccentric ( thin wall, bigger chamber ) 1. Physiological - Cell enlargement - Normal contractile func - No fibrosis 2. Pathological - Cell enlargement - Impaired contractile func - Cardiac fibrosis ( m. increase/ replace w/ collagen) Causes: - Chemical Stimulation : Hormone , Drug ( e.g Adrenergic ) - Mechanical stimulation: Stretching ( e.g. Hypertension ) Effect of cardiac Hypertrophy on cardiovascular func - Increase in contraction Force ( more m. fiber ) - Pathological -> contractility is mostly decrease - Reduce myocardial compliance ( diff of m. to relax ) 3. Discuss the body compensation after heart failure Defect: - Decreased myocardial contractility - Decreased stroke volume (Ejection) Consequences: - Lung congestion ( blood leak ) - Low blood pressure ( less blood go to aorta ) - Tissue hypoxia Increased heart rate - Increased sympathetic activation - Increased plasma catecholamine - Reserve plasma volume (body water) Cardiac Biomarker of Myocardial Damage ( check through blood ) - H-FABP (heart-type fatty acid binding protein) - Myoglobin - CK-MB (creatine kinase myocardial band) - Cardiac troponinT - Cardiac troponin I Cardiac Abnormalities: - Chest pain - Headache and Feeling faint (presyncope) - Hypotension - Tachycardia - Decreased ventricular contractility [ Ejection Fraction = SV/EDV ] - ECG abnormality - Tissue edema (lung congestion) - High level of plasma epinephrine - Cardiac biomarker
- 33. L8 Common Vascular disease 1. State the criteria of hypertension, sign and symptom and risk factors. Hypertension - SBP >139 mmHg - DBP > 89 mmHg Cause: - Sedentary lifestyle - Obesity ( body mass index greater than 25) - Salt (sodium) sensitivity - Alcohol - Smoking - Family history of cardiovascular diseases Risk Factors: - > 65 age - Male > female - HR resting > 80 BPM - High LDL-C/Triglyceride - Menopause - Psychological stress - Chronic kidney disease Pathophysiology 1. ⬆️TPR 2. ⬆️BP - Inability of the kidneys to excrete sodium - An overactive renin-angiotensin system, vasoconstriction and retention of sodium and water → hypertension - An overactive sympathetic nervous system Consequence of Chronic Hypertension - Vascular remodeling (thickening)→artery diseases Endothelial Dysfunction( loss dilation ability) - Left Ventricular Hypertrophy - Impaired Kidney Functions Treatment and Prevention - Vasodilators: ACE inhibitor, Angiotensin II receptor blocker - Low sodium consumption - Low fat consumption - Regular aerobic exercise (avoid static resistance) Major symptoms of hypertension are light headedness, dizziness or nausea. - How are these symptoms developed?
- 34. 2. Discuss the pathophysiology of atherosclerosis - Atherosclerosis is a condition in which plaque builds up inside the blood vessel resulting in the heart to become hardened. -> less blood flow supply tissue - Cause/risk factor: - High Cholesterol ( major ) - Aging - Hypertension - Diabetes - Smoking - Inactivity - Obesity - First, Hypertension or Hyperlipidemia trigger the production of arterial oxygen free radicals, activating the transcription of endothelial redox-sensitive genes and further expresses VCAM-1, mCSF and MCP-1 in endothelium causing the arterial mononuclear leukocyte recruitment which induces inflammation in the atrial wall. - Other risk factors, smoking , hypertension, diabetes and dyslipidemia contribute to the generation of ROS and UAFR which mainly activate endothelial dysfunction causing inflammation on the vascular wall. After the plaque forms , it completely develops atherosclerosis. - In cellular events, the formation of the plague started by the weakening of endothelial cells , increasing the permeability. The monocyte caught its chance to adhesion and transmigration into the vascular wall, engulfing cholesterol LDL, transforming into foam cells and then generating the many other cell migrations to form plague underneath the vascular endothelial. - The generation of these cells is associated with imbalance of cholesterol influx, esterification and efflux. - Type: 1. Most clinically silence ( no effect ) 2. Complicated plaques - Fissure / Ulcerate ( block to other tissue ): athero-emboli. - Thrombose ( blockage ) : occlude, embolise - Hemorrhage ( rupture ): occlude. - Effect: 1. Stenose -> Ischaemia ( low blood flow to tissue , meaning cells receive less nutrients and may enter atrophy) 2. Occlude ( by thrombose / hemorrhage) giving infarct 3. Aneurysm ( enlargement of endothelial wall) causes the vessel to easily break or rupture. Diagnosis - Angiography - Exercise stress test (coronary a.) TX - Balloon Angioplasty
- 35. 3. Discuss the pathophysiology of varicose vein Venous Abnormalities Venous Obstruction - Effect: Pain, edema, hyperpigmentation, ulceration - leads to venous hypertension & Valvular incompetent ( Superficial Varicose vein ) Normal Obstruction Edema - High PV block blood flow out of capillary bed - Blood remaining in capillary -> High Capillary Pressure ( Pc ) - Resulting ⬆️capillary filtration leading to water remain in tissue
- 36. Treatment - Sclerotherapy ( damaging v. -> Scar ( then take scar out ) ) - Vein stripping Prevention - Regular leg exercise/avoid long-time single posture - Compression garment ( compress superficial v. -> make blood easier to flow ) Risk factor - Pregnancy - Femal - Overweight - Aging Summary - Common vascular diseases - Hypertension and atherosclerosis - Atherosclerosis causes coronary heart disease and cerebral ischemia (storke) - Aging, free radicals, cholesterol are risk factors of both hypertension and atherosclerosis - Common venous abnormality is obstruction and varicose. - All problems can be reduced by regular exercise
- 37. L8 Capillary Circulation. CAPILLARY STRUCTURE - Endothelial cells - Basement membrane - Pericytes [ supporting cell ] - Not part of the tube - Maintain endothelial func, Regulation of Fluid flow across membrane SPECIAL STRUCTURES [ diff organ diff structure ] 1. Describe the significance of capillary flow - Vessel size & flow - Although capillary has a very tiny radius, number of capillary and their arrangement make capillary has very low resistance - Because vascular system arranged in parallel circuit, resistance is lower when number increases - Slow rate of flow help the transportation of nutrient? 2. Blood Viscosity = internal fiction within a moving fluid or shear stress - Blood viscosity is dominated by haematocrit. - Viscosity is very low in capillary. - In capillary, flow is a single file flow (bolus). - Because red cell moving in capillary is very regular uniform, internal friction is eliminated. - Very low viscosity helps lower resistance to flow in capillary.
- 38. Capillary activities: - Capillary Blood Flow - capillary bed formation is in a network, capillary area is very high. - High capillary area causes slow blood flow. - slow flow is very good for nutrient and gas exchange. - Transcapillary Exchange - Diffusion: Fick’s law - Capillary Filtration ( water diffusion ) - Filtration is based on interaction among “Hydrostatic pressures” and “Oncotic pressures” - Four pressures involved in capillary filtration - Capillary hydrostatic pressure (Pc) - Capillary oncotic pressure (c) - Interstitial hydrostatic pressure (Pi) • Interstitial oncotic pressure (i) Capillary Filtration and Reabsorption - Filtration occurs more at first entry to the capillary due to high hydrostatic pressure (Pc). - At the later half of capillary, hydrostatic capillary pressure (Pc) decreases leading to more fluid reabsorption. - fluid left in the tissue -> absorbed by lymphatic system EDEMA = pathological symptom of excessive water accumulation in interstitial space. - occurs when capillary filtration is higher than capillary fluid reabsorption.
- 39. Capillary Hydrostatic Pressure - High Pa increases high blood flow into the capillary bed. - High Pv blocks blood flow out of the capillary bed (remaining in capillary). - In cardiac failure, blood could not pump out of the heart, then blood remains in the venous site causing high Pv→high Pc→and edema. - In liver disease, protein production is decreased & increased in protein degradation, causing low pi c. - Pinocytosis [ big ion pass through w/ this ] - Peptides / Lipid molecule - - Endothelial Functions - Endothelial cells involved in production of: - Nitric Oxide → Vasodilation - Endothelin 1 → Cell growth - Blood clotting regulation - signals stimulate endothelial cells. - Chemical: Ach, ADP, Histamine, etc - Mechanical: Shear stress - Doctor mimics the action of the endothelial cell - by giving “Nitroprusside” which is NO donor to dilate obstructed or stenosed vessels. - ENDOTHELIAL VASOACTIVE - Examples of paracrine released from endothelial cells which affect vascular smooth muscle. - Vasodilation: - NO - Prostacyclin - Endothelial Derived Hyperpolarizing Factor - Vasoconstriction: - Thromboxane AII - Endothelin-1 - Local angiotensin II - ANGIOGENESIS - formation of new blood vessels - migration, growth, and differentiation of endothelial cells, which line the inside wall of blood vessels. - factors: [ can induce ] - Vascular endothelial growth factor (VEGF) - Fibroblast Growth Factor (FGF) - Tumor necrosis factor-alpha (TNFF-α)
- 40. L9 Venous Circulation 1. Describe the function of the venous system as the blood reservoir. Characteristics - Receive blood from tissues and pass them to the heart. - Deep and superficial veins (No superficial artery) - Thin wall - Venous valves - High compliance -> Low pressure , no pulse - VP ⬆️V. become rounder - Blood reservoir - Low pressure - Suitable for blood collection - But, easy to be compressed Due to high compliance, venous pressure is very low and no pulse. Vp⬆️V become rounder 2. Explain the factors influencing venous return. Venous return ⬆️ Pb⬆️: Venous & Rt. HP ∆ Factor affect venous return: 1. Central venous pressure = 2 mmHg 2. Right ventricular Pressure = 0 mmHg during diastole (relaxation). 3. Time of ventricular relaxation 3 systemic v. return to heart 1. Coronary sinus 2. Inferior vena cava 3. Superior vena cava Venous Blood Flow - Flow in Unidirectional flow due to Bicuspid valve - Velocity depend on size ( 7-20 cm/s ) Regulation of Venous Return - Effective venous return requires: - Central pump [ ventricle relax ] - Pressure gradient [ V. Pressure ⬆️] - Peripheral venous pump [ gen. V. Pressure ] - Competent venous valves Regulatory Mechanisms - Sympathetic tone (Splanchnic & Cutaneous) / Venomotor tone - Increased by sym stimulation causes smooth muscle in venous wall contraction and decreases venous diameter. - P in v. Higher? - Thoracoabdominal pump - Full inspiration causes low pressure in the thoracic cavity. - compress diaphragm - P chest ⬇️, P diaphragm ⬆️ - Blood from the abdominal vein can move to the chest and heart easier. - Skeleton Muscular pump - Muscle contract -> squeeze v. Size -> blood flow back to heart -
- 41. - calf m. Pump Eff of gravity - During standing -> Gravity draws blood down to feet. - Lay drown -> p? - E = P( pressure energy )+ ρgh(potential) + 1⁄2 ρV^2 ( kenetic) Venous valves - Bicuspid valve - Unidirectional flow - Abnormality >> varicose vein Venous Obstruction SUMMARY Venous Functions: - Deliver blood return to the heart. - Preserve blood volume due to high compliance. - Venous pressure is regulated by sympathetic –induced venomotor tone / external force such as muscle pump, gravity. - Unidirectional valves lead to unidirectional flow
- 42. L10 VASOMOTOR CONTROLS 1. Explain the concept in cardiovascular homeostasis - Neural and Hormonal systems work together maintaining arterial blood pressure, blood volume, PO2 and PCO2. - Parasym and sym activation regulate the cardiac function. - Sympathetic activation ( no parasym in blood v.v. ) and most hormones stimulate vasoconstriction and venomotor tone ( v. Contraction ) - Tissue metabolic control supplies more blood to the active tissues. - Myogenic autoregulation helps maintain blood flow to the important organs. 2. Describe three major systems that regulate cardiovascular function - three system works together to: - Increase blood supply to active tissues: such as to active muscle during exercise - Redistribution of blood under different conditions: such as increased heat lost. - Maintain blood volume and blood pressure under stresses: such as change in position - Maintain adequate blood flow to vital organs: brain, heart, kidneys 1. Neuronal control/ system - Major aim of cardiovascular system: To supply energy and O2 to whole body Cardiovascular Receptors 1. Baroreceptors: Special cells located at the aortic arch and carotid sinus detect blood pressure. - Sensitivity: Amplitude & Frequency 2. Atrial Stretch receptors: Myelinated veno atrial mechanoreceptors. (low pressure receptors) - Sensitivity: Central Blood Volume 3. Chemoreceptors: Special cells detect chemical change dividing into two locations: - Sensitivity: Central: CO2 & H+ (brain) Peripheral: O2, CO2 & H+(Aortic body & Carotid body) 4. Renal Perfusion sensors: Special cell complex (Juxtaglomerular apparatus) detects perfusion pressure of renal artery. Cardiovascular Center*** - = Medulla Oblongata (Brain stem) - mainly controlled by reflexes and central command Cardiovascular Controls 1. Parasympathetic: Ach - SA node = decrease HR - AV node = slow conduction velocity - Ventricles = Inhibit Sympathetic activity 2. Sympathetic Adrenergic: NE - SA node = increase HR - AV node = increase conduction - Ventricles = B1-AR = Contractility
- 43. Cardiac Action ( จําแค่2อันแรก) - Chronotropic action: Change in heart rate - Inotropic action: Change in contraction force - Dromotropic action: change in electrical conduction rate - Bathmotropic action: change in cardiac excitability - Lusitropic action: change in rate of myocardial relaxation Example: - Positive chronotropic effect = increased heart rate (Tachycardia) - Negative inotropic condition = decreased myocardial contractility (heart failure) 2. Humoral control - Vasopressin ( Antidiuretic hormone) -> vasoconstriction - Atrial natriuretic peptide ( AND ) -> Vasodilation - Bradykinin -> vasodilation of skin , saliva gland & gut circulation Plasma Electrolyze & Vasomotor Activity - vasoconstriction : Calcium - vasodilation - K+ - Proton (H+) - CO2 - Hyperosmolarity (such as glucose) - Mg2+ Example: - Hyperkalemia (high plasma K+) -> vasodilation. - Acidosis (high plasma H+) -> vasodilation. 3. Local control - Fluid flow: high pressure→low pressure Role of vasodilator metabolites - Accumulation→Increased blood flow - Vasodilation - ⬆️K+ ( high AP ) - ⬆️lactate ions - ⬆️adenosine - ⬆️pCO2 - ⬇️oxygen tension - ⬇️pH - ⬆️temperature Role of Substances released by endothelium 1. Prostaglandin and Thromboxane A2 - Prostacyclin → Vasodilation - Thromboxane A2 →Vasoconstriction 2. Endothelin Derived Relaxing Factor (EDRF) [Nitric Oxide] ( จําแค่นี้) - Vasodilation - Stimulate cGMP → Relaxation of vascular smooth muscle by decreasing intracellular Ca2+. 3. Endothelin 1→ Vasoconstriction
- 44. 3. Discuss mechanisms that regulate blood supply via coronary and cerebral arteries. - Coronary Circulation ( Supply to → Cardiac Muscle ) Cardiac Muscle : Pump blood -> 8-10 ml O2/min/100g - Regulation of Coronary Blood Flow - Metabolic factors - Local metabolic factor is the major regulatory mechanism controlling coronary blood flow. - The mechanism is directly associated to the myocardial activity - Physical Factors: Extravascular Compression - systole -> muscle contraction compresses coronary circulation (Squeezing effect) - Very small blood flow in the left coronary artery - Diastole -> Blood flow in the coronary artery is highest - Cerebral Blood Flow ( supply to -> tissue ) - Regulation of Brain Blood Flow - Myogenic Autoregulation