Personal Health Informatics Patient Participation In Precision Health Peiyun Sabrina Hsueh
Personal Health Informatics Patient Participation In Precision Health Peiyun Sabrina Hsueh
Personal Health Informatics Patient Participation In Precision Health Peiyun Sabrina Hsueh
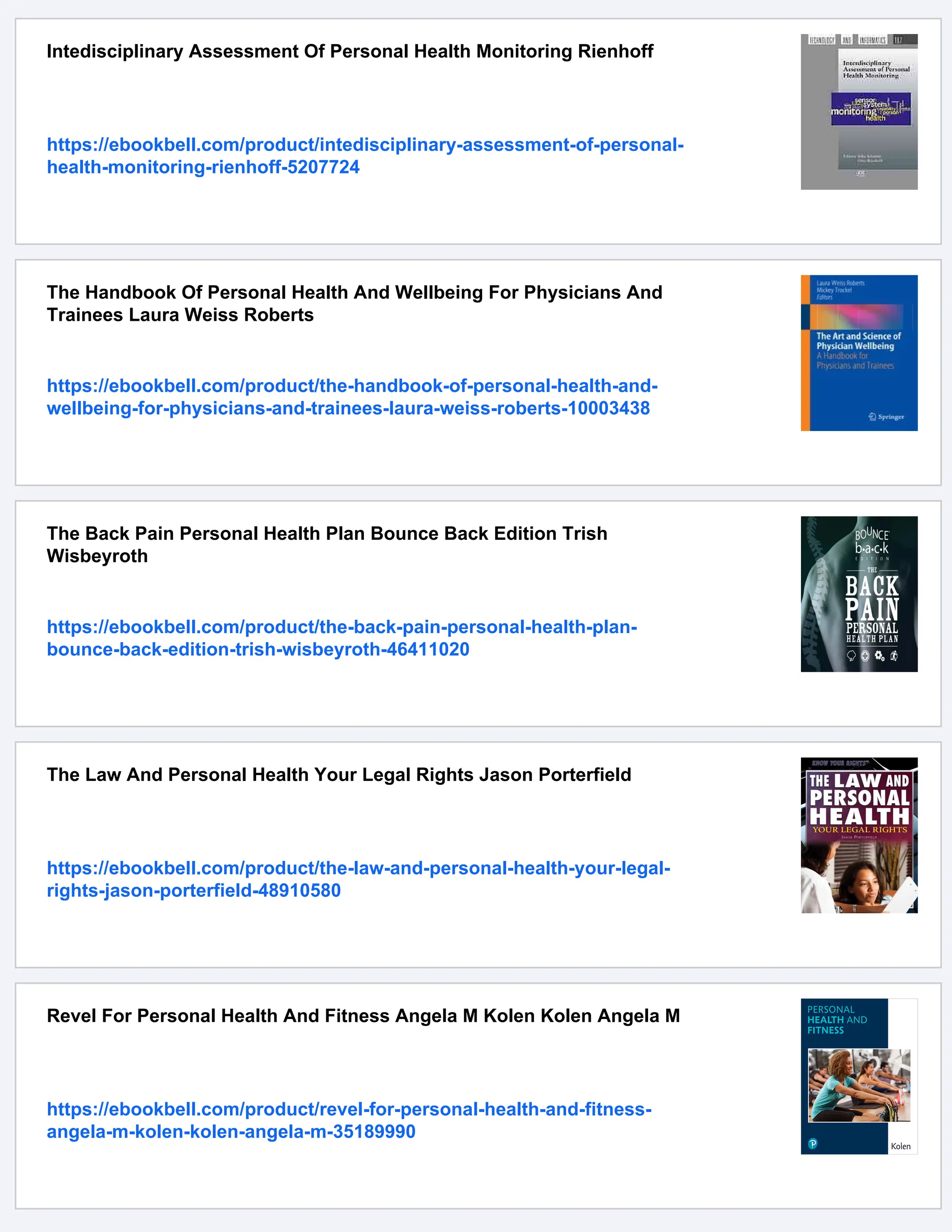
























![xxv
About the Editors and Contributors
About the Editors
Pei-Yun Sabrina Hsueh, PhD is an elected Fellow of the American Medical
Informatics Association (FAMIA), the co-Chair of AMIA AI Showcase 2023, the
Vice Chair of AMIA SPC 2022, and the Past-Chair of the Consumer Health
Informatics Work Group at AMIA. She is also currently serving on the Practitioner
Board of ACM. She is a global health AI leader and innovator, specializing in trans-
lating real-world problems into data science formulations and developing AI/ML
solutions to decode individual biology and behavior for precision healthcare deliv-
ery applications. She has a decade of experience leading cross-functional teams to
productize and evaluate health AI applications in practice. Previously at IBM
Research, she co-chaired the Health Informatics Professional Community and was
elected as an IBM Academy of Technology Member. Dr. Hsueh has been a pioneer
in Health AI, focusing on real-world evidence strategy and the development of plat-
forms to deliver clinical studies and actionable insights at the point of care. Her
achievements have won her a series of awards, including the AMIA Distinguished
Paper Award, invention, research achievement, manager choice awards, Eminence
and Excellence Award, and the Google Anita Borg Scholar Award. In addition, she
authored 20+ patents and 60+ technical articles in computational linguistics and
health informatics. Her expertise in the emerging areas and industry solutions makes
her a sought-after speaker and consultant, a thought leader in real-world evidence,
and chairs of applied data science events at major conferences such as AMIA,
MEDINFO, MIE, and KDD. She is also an editor of Machine Learning for Medicine
and Healthcare (Springer Nature), a guest editor of special issues in Sensors Journal,
Public Health, Journal of American Medical Informatics Association [JAMIA
OPEN], and the Frontier of Public Health.
Thomas Wetter is a Medical Informatics scholar with 12 years of experience in
industry research and 30 years of experience in academic research and teaching in
Biomedicine. He is a graduate and PhD in Mathematics from Aachen Technical](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-28-2048.jpg)






























![This ebook is for the use of anyone anywhere in the United
States and most other parts of the world at no cost and with
almost no restrictions whatsoever. You may copy it, give it away
or re-use it under the terms of the Project Gutenberg License
included with this ebook or online at www.gutenberg.org. If you
are not located in the United States, you will have to check the
laws of the country where you are located before using this
eBook.
Title: The Philosophy of Fine Art, volume 3 (of 4)
Author: Georg Wilhelm Friedrich Hegel
Translator: Francis Plumptre Beresford Osmaston
Release date: September 25, 2017 [eBook #55623]
Most recently updated: October 23, 2024
Language: English
Credits: Produced by Laura Natal Rodriguez and Marc D'Hooghe
at
Free Literature (online soon in an extended
version,also
linking to free sources for education worldwide ...
MOOC's,
educational materials,...) Images generously made
available
by the Internet Archive.)
*** START OF THE PROJECT GUTENBERG EBOOK THE PHILOSOPHY
OF FINE ART, VOLUME 3 (OF 4) ***](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-60-2048.jpg)



![of the aspects identical in all. The origins of art. Grace, Charm,
and severe or agreeable Style] 3
DIVISION OF THE SUBJECT
[The principle of differentiation as determined by the sensuous
aspect of the subject-matter, and the relation thereto of the
human senses of Sight, Hearing, and intellectual Conception.
Insufficiency of such a principle of classification. Alternative
principle discussed and illustrated of more concrete nature, in
which the evolution of truth as the reality of the Idea itself is
presented] 14
SUBSECTION I
ARCHITECTURE
INTRODUCTION
[Of the beginnings of human art, and that of building in
particular. Of the nature of the subordinate classification of
architecture viewed as symbolic, classical and romantic] 25
Division of Subject 26
CHAPTER I
INDEPENDENT AND SYMBOLIC ARCHITECTURE
Introduction and Subdivision 32
1. Works of architecture erected in order to unite peoples 36
2. Works of architecture intermediate between the arts of
building and sculpture 38](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-64-2048.jpg)

![(a) Buildings of wood and stone. The question of their historical
priority 66
(b) The specific forms of the parts of a temple-dwelling. 68
[(α) Features of support. The column 69
(β) The thing supported. The entablature, in its architecture,
cornice, etc. 72
(γ) That which encloses. The walls and partitions] 74
(c) The classical temple in its entirety 77
[(α) The horizontal rather than soaring-up character 78
(β) The simplicity and proportion 78
(γ) The nature of its elaboration] 79
3. The different constructive types of classical architecture
(a) The Doric, Ionian, and Corinthian types, compared
and contrasted 80
(b) The Roman type of building. The vault 86
(c) General character of Roman architecture 88
CHAPTER III
ROMAN ARCHITECTURE
1. General Architecture 89
2. Particular architectural modes of configuration 91
(a) As the basic form we have the wholly shut away dwelling-
house 91
[(α) Relation of this form to the ideal character of the Christian
religion 91
(β) Exclusion of light and access to mundane life](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-66-2048.jpg)
![(γ) The aspect of soaring in tower and pinnacle] 92
(b) The form of the exterior and interior 92
[(α) The figure of the square and rectangular roofing not
appropriate. Parallel between the vaulting of a Gothic church
and a roofing of forest trees. Distinction between piers and
columns. The pointed arch. Distinction between choir, transept,
nave, and aisles. The baptismal font and entrance 93
(β) In contrast to the Greek temple decoration and and general
co-ordination of parts determined from within outwards. The
form of Cross. The doors. Flying buttresses, pinnacles, and
towers] 100
(c) The mode of decoration 102
[(α) Importance of ornament to Gothic architecture 102
(β) Lightness and delicacy a prevailing feature, especially on the
outside 103
(γ) Display of romantic imagination therein] 104
3. Different types of building in romantic architecture 104
(a) The pre-Gothic architecture distinct from it. The basilica 105
(b) Genuine Gothic architecture of the thirteenth century 105
(c) Secular architecture of the Middle Ages. The art of garden-
making 106
SUBSECTION II
SCULPTURE
INTRODUCTION
[Sculpture makes a direct use of the human form instead of
accepting a symbolical mode of expression merely suggestive of](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-67-2048.jpg)
![spiritual import. Does not primarily express emotion or spiritual
life in action or the focus of soul-life. Absence of colour] 109
Division of subject 118
CHAPTER I
THE PRINCIPLE OF GENUINE SCULPTURE
1. The essential content of sculpture 121
[(a) The twofold aspect of subjectivity. The province of
subjective life as such to be excluded from sculpture. The Divine
presented in its infinite repose and sublimity 122
(b) Presents a spiritual content only as explicit in bodily shape]
125
2. The beautiful form of sculpture 126
(a) The exclusion of the particularity of the appearance. How far
relative 130
(b) The exclusion of incidental facial expression 130
(c) Substantive individuality 131
3. Sculpture as the art of the classical Ideal 132
CHAPTER II
THE IDEAL OF SCULPTURE
Introduction and division of subject 135
1. The general character of the ideal form of sculpture 137
(a) The free product of the genius of the artist. General content
borrowed from mythology, etc. 139
(b) The animation which results from the plastic perfection of
the integrated coalescence of the whole throughout its definition](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-68-2048.jpg)
![and relief 140
(c) No mere imitation of Nature. The external shape must be
suffused with ideal content] 141
2. The particular aspects of the ideal form of sculpture as such
142
(a) The Greek profile. Contrast of the human mouth with that of
animals. The projection of the forehead. Position of nose.
Consideration of the human eye and ear. Beauty of the human
mouth. Treatment of the chin in sculpture, also the hair 143
(b) Position of other parts of the human body and the motion
thereof 147
[(α) The nature of the relation under which the limbs are
associated in their contribution to spiritual ideality. The upright
position 156
(β) The motion and repose of the same in their freedom and
beauty 159
(γ) The type of position and motion adapted to a situation
(habitus) or bodily habit under which the Ideal is expressed] 160
(c) Drapery 160
[(α) Ethical origin and artistic justification of, in sculpture 161
(β) Treatment of it by Greek sculpture 162
(γ) Artistic principle as determining the right emphasis on ideal
significance. Contrast between antique and modern sculpture in
the use of it] 165
3. The individuality of the ideal figures of Sculpture 171
(a) Incidental attributes and style of drapery, armour, etc.,
treated by sculpture. Distinguishing symbolic accessories of
Greek gods 173
(b) Distinctions of age and sex in gods, heroes, human figures,
and animals 177](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-69-2048.jpg)

![[The principle of subjectivity as such. How it is accepted as the
essential principle by romantic art. The contrast presented by
romantic and classical art in the changed point of view. The
effect of such a change on both the subjective side of soul-life
and the external aspect of objective presentment. The process
of the gradual idealization of the external medium of art itself as
illustrated by the particular romantic arts and the necessity
thereof] 217
CHAPTER I
THE ART OF PAINTING
Introduction and division of subject 223
I. General character of Painting 225
(a) Fundamental definition of the art. Combines the subject-
matter of architecture and sculpture. More popular than
sculpture 230
[(α) Individuality must not be suffered to pass wholly into the
universality of its substance. Introduction of accidental features
as in Nature 230
(β) Greatly extended field of subject-matter. The entire world of
the religious idea, history, Nature, all that concerns humanity
included 231
(γ) A revelation further of the objective existence of soul-life.
Vitality of artist imported into his presentation of natural
objects] 231
(b) The sensuous medium of Painting 232
[(α) Compresses the three dimensions of Space into two. Its
greater abstraction, as compared with sculpture, implies an
advance ideally. Its object is semblance merely, its interest that
of contemplation. The nature of its locale 233](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-71-2048.jpg)
![(β) Its higher power of differentiation. Light its medium. This
implies, even in Nature, a movement towards ideality. The
appearance of light and shadow in painting intentional. Form is
the creation of light and shadow simply. This fact supplies
rationale of the removal of one dimension from spatial condition
236
(γ) This medium enables the art to elaborate the entire extent
of the phenomenal world] 240
(c) The principle of the artistic mode of treatment 241
[Two opposed directions in painting, one the expression of
spiritual significance by interfusion with or abstraction from
objective phenomena, the other the reproduction of every kind
of detail as not alien to its fundamental principle. Illustrations of
the two methods and their relative opposition, or reconciliation]
2. Particular modes in the definition of Painting 244
(a) The romantic content 245
[(α) The Ideal which consists in the reconciliation of the soul
with God as revealed in His human passage through suffering.
The religious content. The Love of religion 247
(αα) The representation of God the Father. Generally beyond the
scope of painting. The famous picture of Van Eyck at Ghent 251
(ββ) Christ the more essential object. Modes of depicting him in
his absolute Godhead or his humanity. Scenes of Childhood and
Passion most fitted to express religious aspect. Love of the
Virgin Mary. Contrast with Niobe 253
(γγ) The ideas of devotion, repentance, and conversion as such
affect humanity in general when included in the religious
sphere. The pictorial treatment of martyrdom 260
(β) The pictorial treatment of landscape 266
(γγ) The pictorial treatment of objects in natural or secular
associations. The vitality and delight of independent human](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-72-2048.jpg)
![existence. Art secures the stability of evanescent phenomena.
The influence of artistic personality on the interest] 268
(b) The more detailed definition of the material of pictorial
representation 273
[(α) Linear perspective 274
(β) Accuracy of drawing of form. The plastic aspect of a pictorial
work 274
(γ) The significance of colour. Modelling. Of gradations of colour
and its symbolism. Of various schemes of colour. Colour
harmony. The painting of the human flesh. The mystery of
colour The creative impulse of the artist] 275
(c) Artistic conception, composition, and characterization 290
[Painting can only embody one moment of time. Concentration
of interest. The law of intelligibility. Religious subjects, their
advantage in this respect. Historical scenes as appropriate to
particular buildings. Unity of entire effect. Raphael's
Transfiguration. Of the treatment of landscape as subordinate.
The grouping of figures. The form of the pyramid. Comparison
of the characteristic in painting and sculpture. The treatment of
love's expression in religious subjects. The gradual elaboration
of the portrait. The situation which is itself a critical moment in
characterization] 291
3. The historical development of Painting 313
(a) Byzantine painting 315
(b) Italian painting. General review of its spirit in religious and
romantic subject-matter 317
[(α) Characteristic features of early type: austerity, solemnity,
and religious elevation 321
(β) The free acceptance of all that is human and individual. The
influence of Giotto. Later schools mark a still further advance in](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-73-2048.jpg)
![naturalism. Masaccio and Fra Angelico. The pictorial
representation of secular subjects 322
(γ) Further advance in power of emotional expression. Leonardo
da Vinci, Perugino, Raphael, and Correggio.] 327
(c) The Flemish, Dutch, and German schools 330
[(α) The brothers Van Eyck. Innocence, naïveté, and piety of
early Flemish School. Contrast with Italian masters 330
(β) The emphasis by North German painting on ugliness and
brutality 332
(γ) Dutch painting. Historical conditions of its appearance.
General characteristics of Dutch art] 333
CHAPTER II
MUSIC
INTRODUCTION
[Summary. The principle of subjectivity, as realized in painting,
contrasted with its complete emancipation in the art of music.
Annihilation of spatial objectivity. Motion with its resultant effect
in musical tone. Analysis of the twofold negation of externality
in which the fundamental principle of musical tone consists. The
inner soul-life exclusively the subject-matter of music.
Addressed also in its effect to such] 338
Division of subject 344
1. The General Character of Music 345
(a) Comparison of music with the plastic arts and poetry
[(α) Both affiliated to and strongly contrasted with architecture.
It resembles architecture in the nature of the configuration of its
content as based on rigorously rational principles directed by
human invention. It supplies the architectonic of the extreme of](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-74-2048.jpg)
![ideality as architecture supplies that of the external material of
sense. The quantitative or measure relation is the basis of both
345
(β) Music further removed from sculpture than painting. This is
not merely due to the greater ideality of latter, but also to its
treatment of its medium. The unity realized by a musical
composition of a different kind to that realized by the plastic
arts. In the former case subject to the condition of a time-series
347
(γ) Most nearly related to poetry. Employ the same medium of
tone. Poetry possible without speech-utterance. Ideal objectivity
of poetry as contrasted with the independence of musical tone
as the sensuous medium of music. Music as an accompaniment
of the voice] 352
(b) Musical grasp and expression of Content 357
[(α) Primarily must not minister to sense-perception. Must make
soul-life intelligible to soul. This abstract inwardness
differentiated in human feeling, of every description 358
(β) Natural interjections not music. They are the point of
departure. To music belongs intelligible structure, a totality of
differences capable of union and disunion in concords, discords,
oppositions and transitions. The nature of its relation to positive
ideas] 359
(c) Effect of music 361
[(α) The evanescent character of the objectivity of music. It
seizes on conscious life where it is not confronted with an
object. Its effect due to an elementary force. Appeal to man as
a particular person. The soul made aware of its association with
Time. Analysis of the notion of Time 361
(β) Must also possess a content. Orpheus. Incentive to martial
ardour and enthusiasm 365](https://image.slidesharecdn.com/24336823-250521114739-e3cec0ce/75/Personal-Health-Informatics-Patient-Participation-In-Precision-Health-Peiyun-Sabrina-Hsueh-75-2048.jpg)
