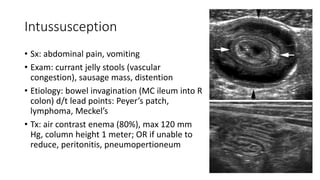
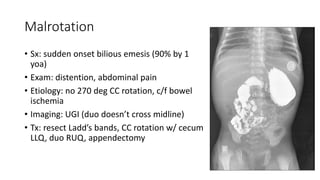
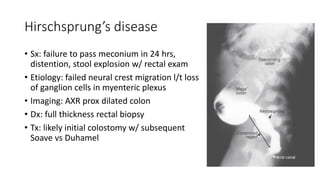
The document outlines pediatric surgical management related to fluids, electrolytes, and several conditions including hypertrophic pyloric stenosis, intussusception, malrotation, gastroschisis, omphalocele, Hirschsprung's disease, umbilical and inguinal hernias, and cryptorchidism. Each condition details symptoms, examinations, diagnostic imaging, and treatments, emphasizing fluid resuscitation, surgical interventions, and specific management approaches tailored to pediatric patients. Key topics include differences in fluid maintenance and electrolyte handling between children and adults, as well as surgical techniques suitable for various congenital and acquired conditions.