This document discusses several common causes of childhood intestinal obstruction including:
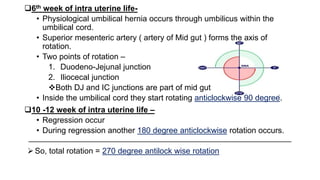
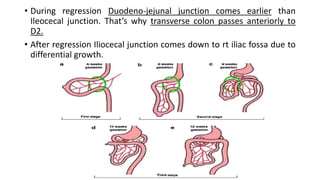
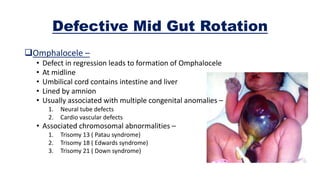
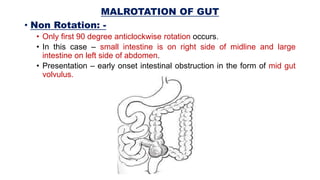
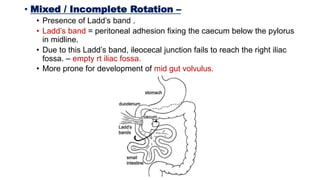
1. Rotation defects that can cause midgut volvulus like malrotation or incomplete rotation.
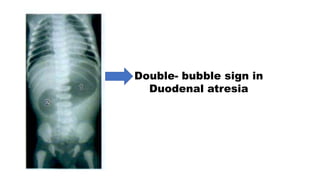
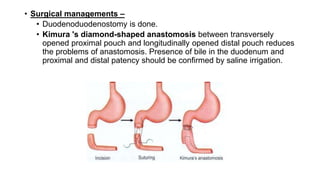
2. Duodenal atresia which presents with jaundice and bilious vomiting in newborns.
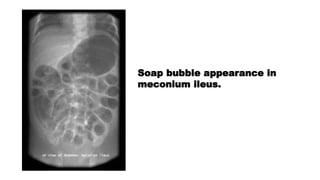
3. Meconium ileus which is thick meconium causing ileal obstruction in cystic fibrosis patients.
4. Congenital hypertrophic pyloric stenosis causing projectile vomiting in infants.
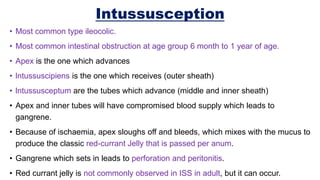
5. Intussusception where one segment of bowel slides into another causing obstruction.
6. Hirschsprung disease where absence of ganglion cells in a segment of colon causes constipation.