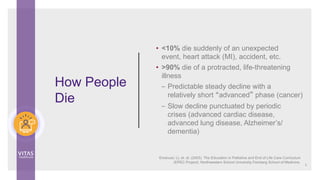
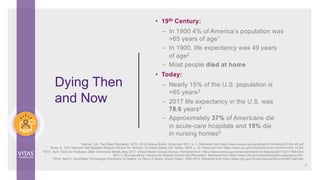
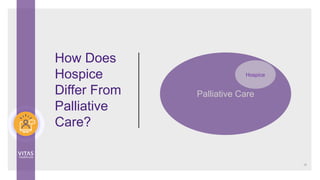
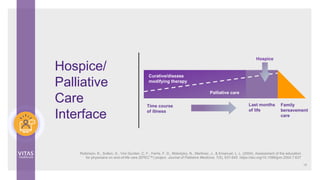
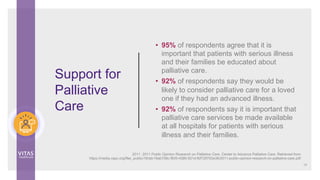
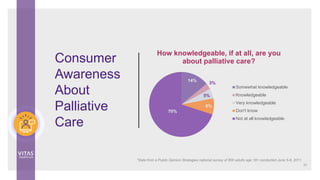
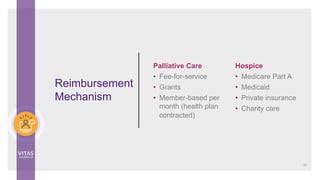
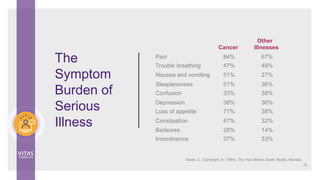
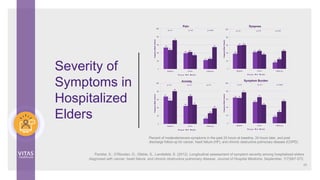
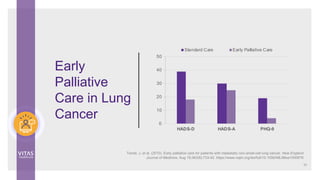
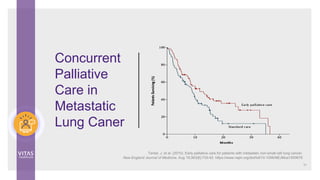
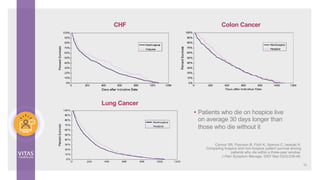
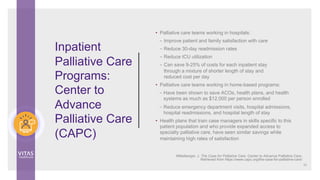
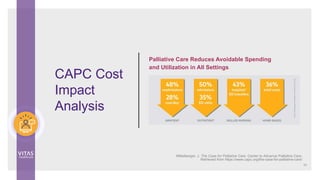
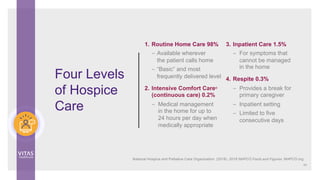
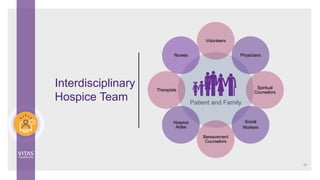
The document outlines the distinctions and benefits between palliative care and hospice care, detailing education and continuing education credits provided by VITAS Healthcare for various healthcare professionals. It highlights the rise in serious health-related suffering projected by 2060, emphasizing the need for palliative care to improve quality of life and patient satisfaction across all health systems. Additionally, it discusses the evolving history of hospice care, its increasing importance in global health, and the significant gap in palliative care accessibility for those in need.