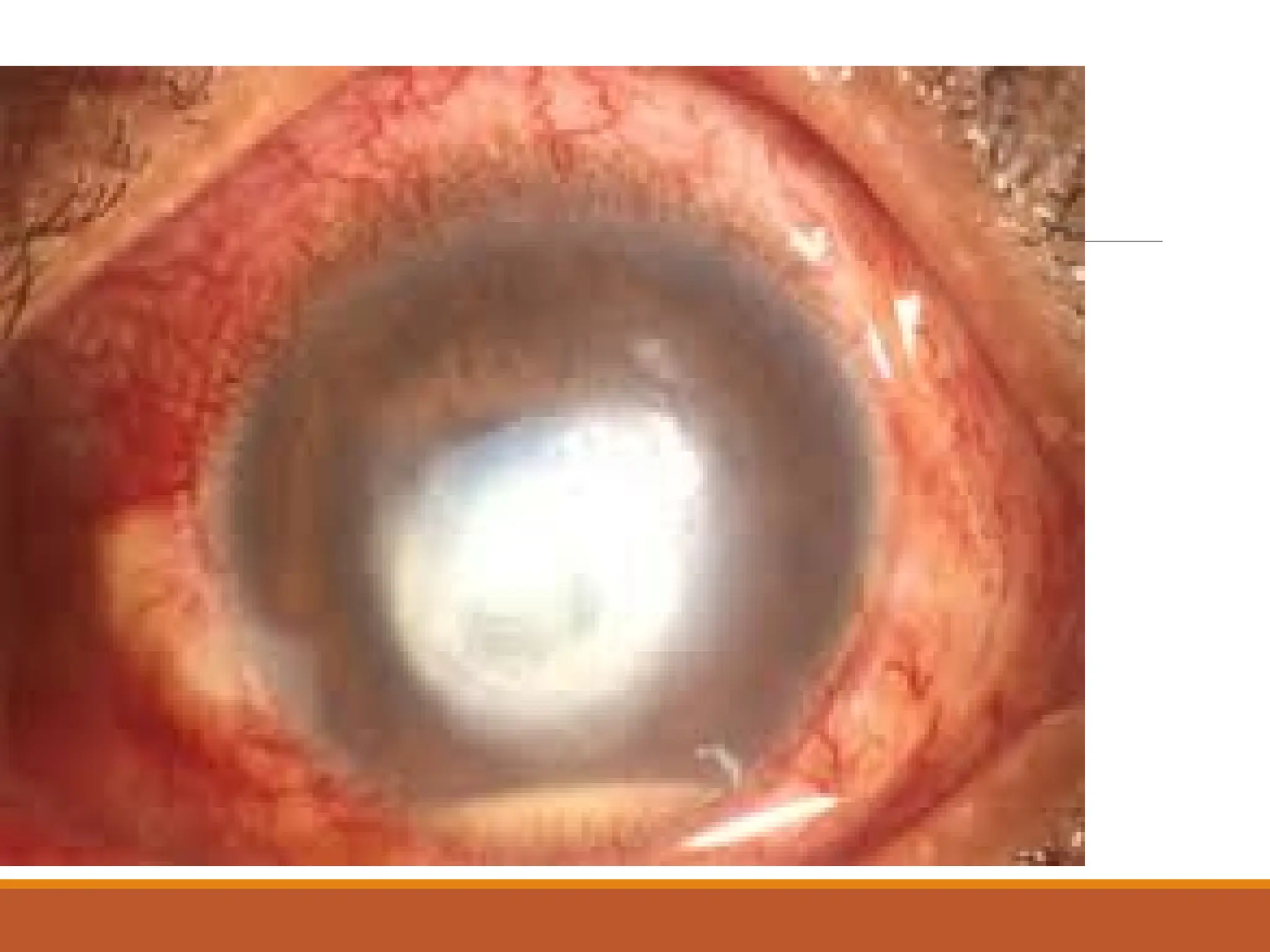
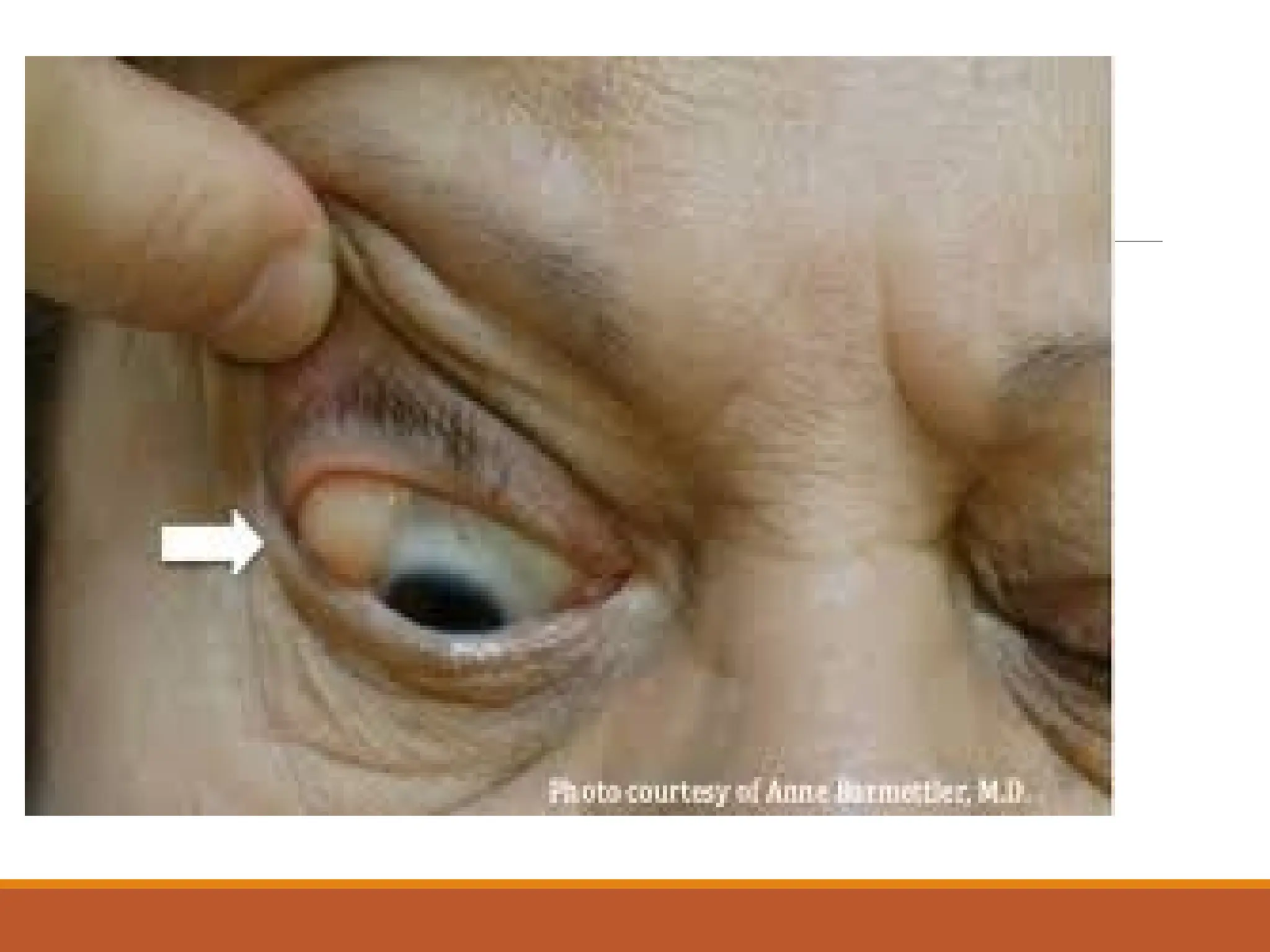
This document provides a comprehensive overview of eye anatomy, normal flora, and various eye infections, including conjunctivitis, keratitis, endophthalmitis, and periocular infections. It details clinical manifestations, routes of infection, and management or treatment options for different types of ocular conditions. Emphasis is placed on the importance of diagnosis and the methods used to evaluate eye infections, alongside common organisms involved.