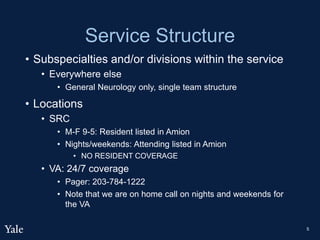
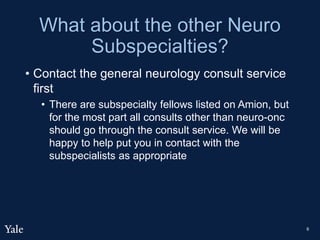
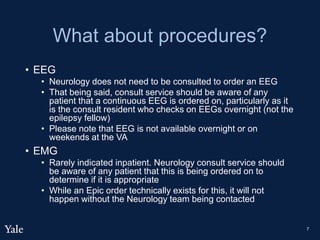
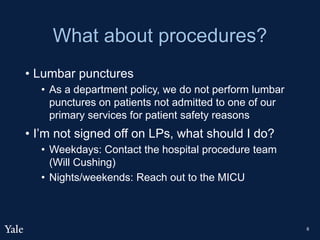
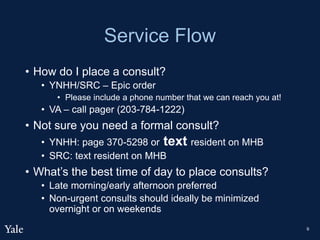
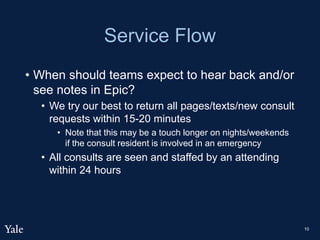
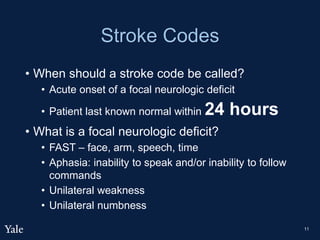
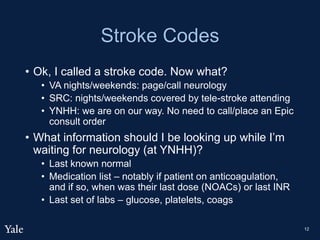
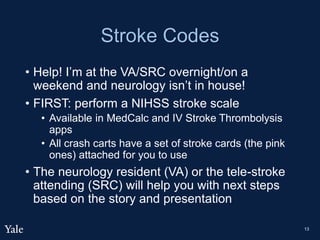
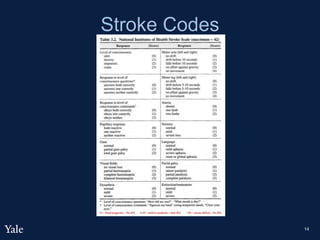
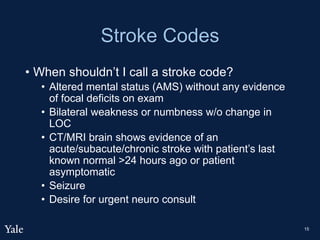
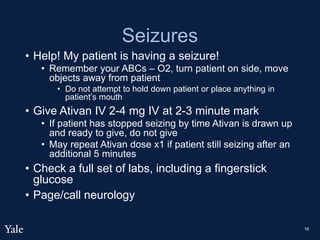
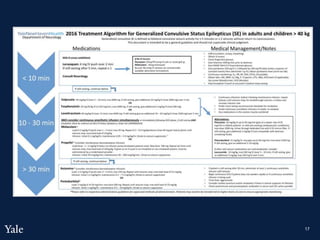
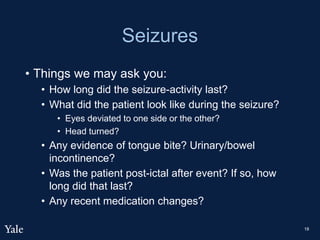
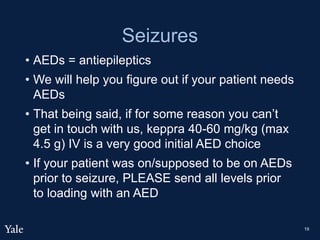
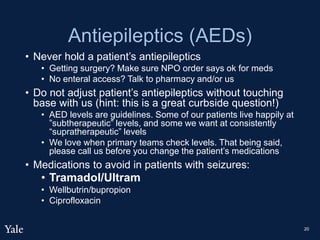
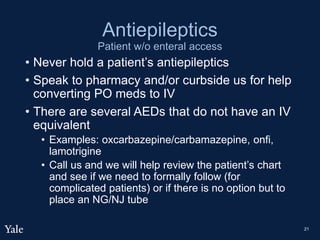
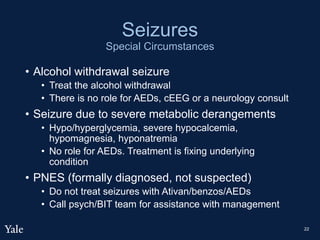
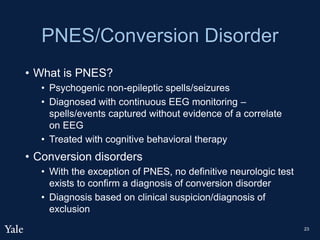
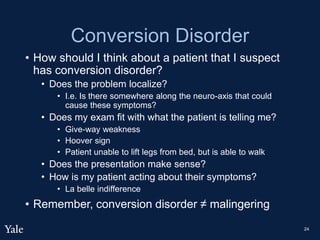
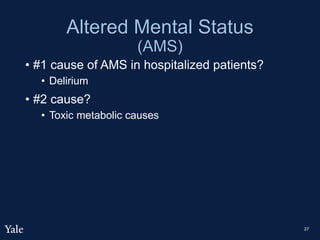
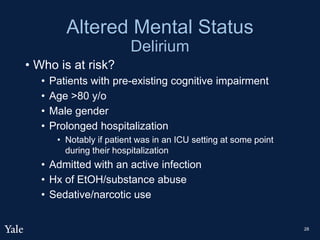
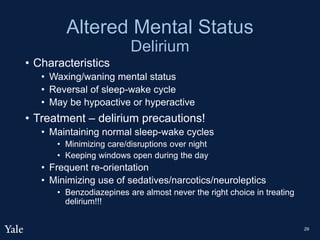
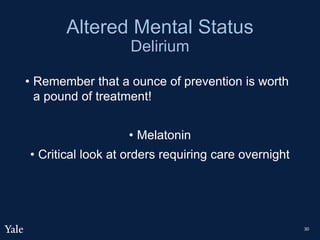
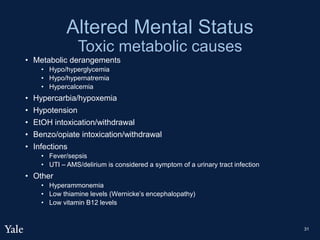
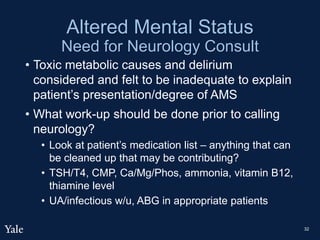
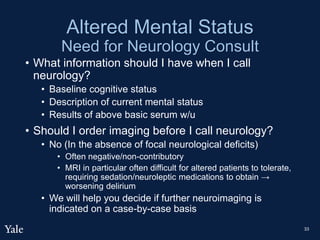
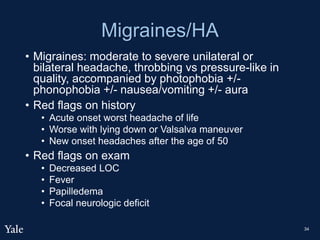
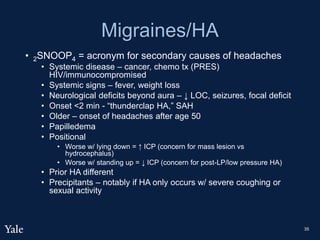
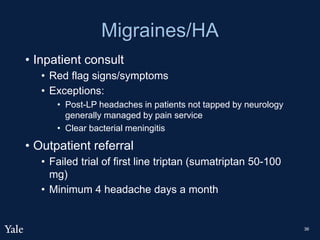
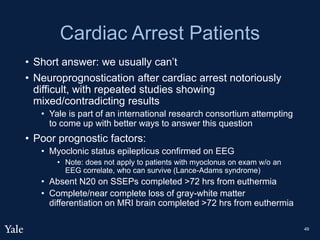
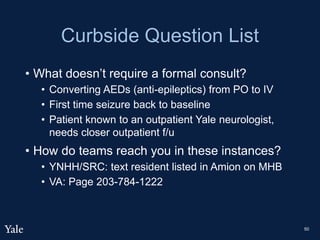
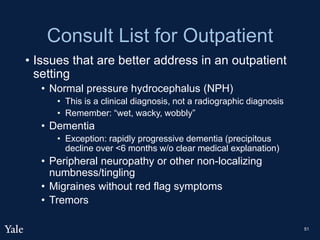
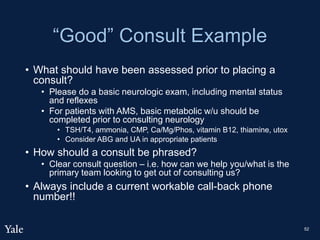
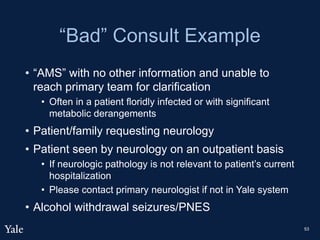
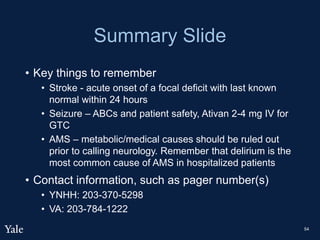
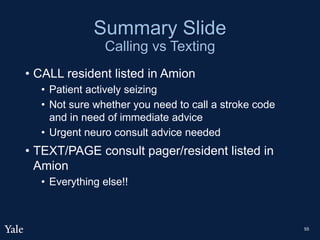
This document provides information about the neurology consultation service structure at various hospitals. It introduces the chief residents, Dr. Chris Traner and Dr. John Picard. It describes coverage details for inpatient neurology, the emergency department, subspecialties, and locations including the VA, SRC, and YNHH. It provides guidance on procedures, placing consults, expected response times, handling stroke codes and seizures, and special circumstances involving altered mental status, delirium, and conversion disorder.