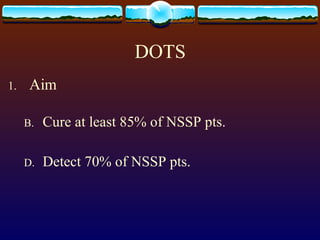
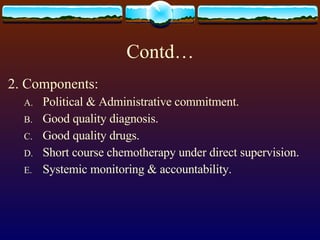
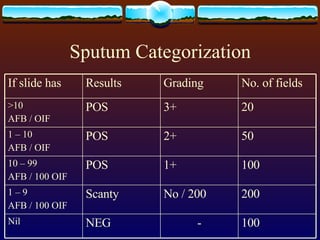
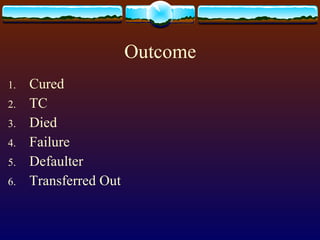
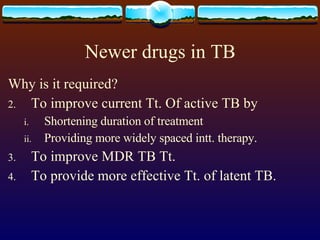
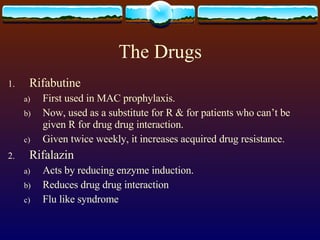
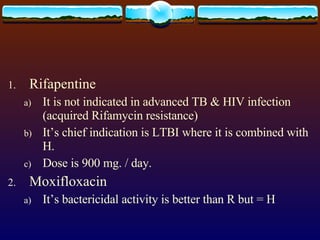
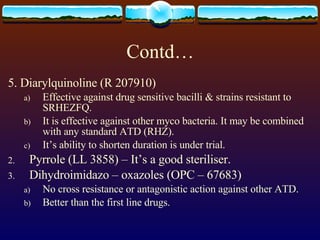
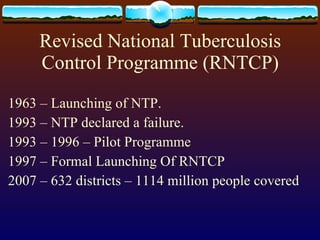
1. The document discusses the management of tuberculosis, including the history, statistics, principles of treatment, protocols, side effects of drugs, and the Revised National Tuberculosis Control Programme in India.
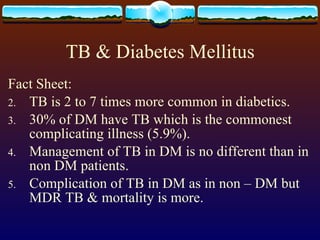
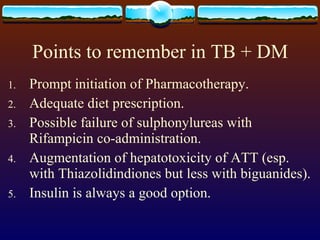
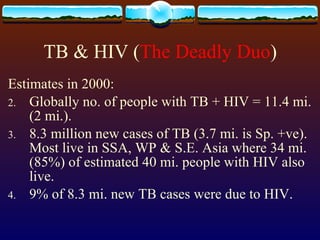
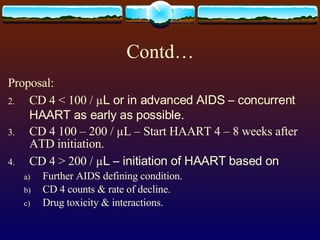
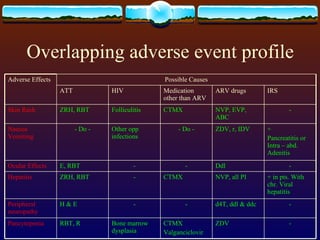
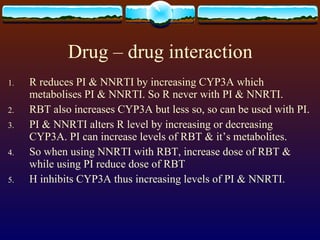
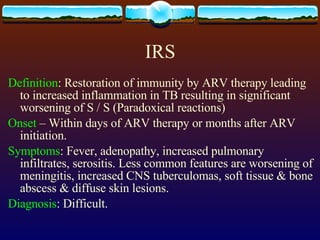
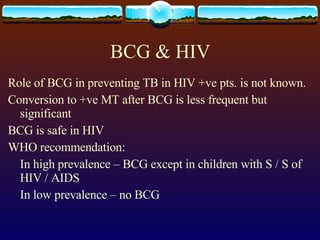
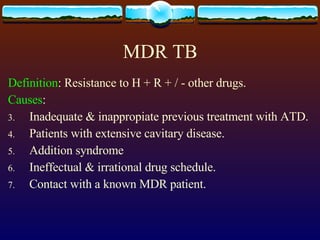
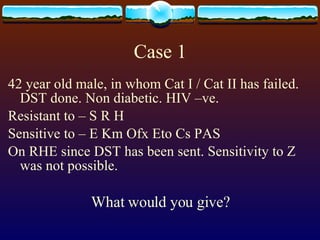
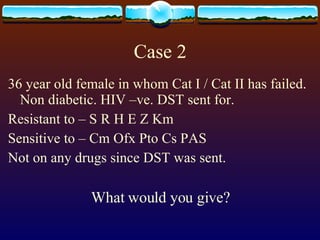
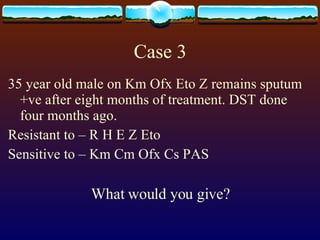
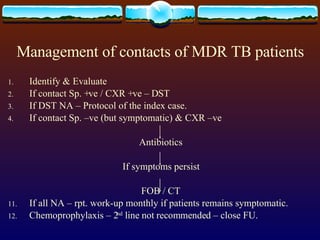
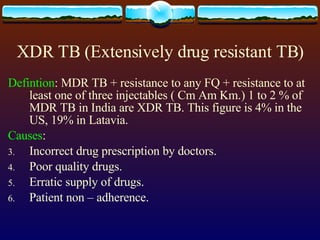
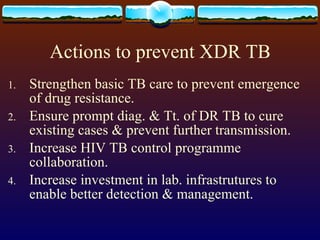
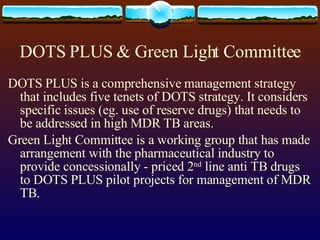
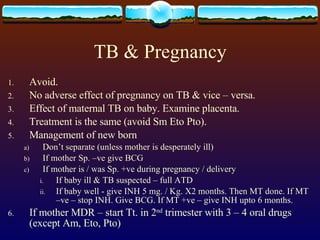
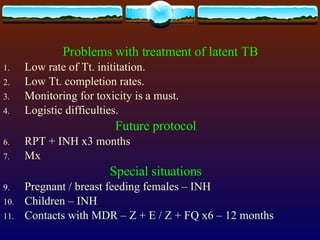
2. It covers topics like tuberculosis and diabetes, tuberculosis and HIV co-infection, multi-drug resistant tuberculosis, and paradoxical reactions seen with antituberculosis treatment and antiretroviral therapy.
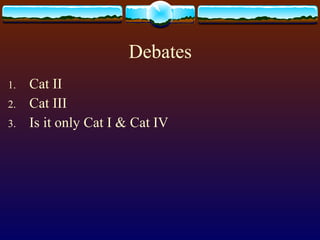
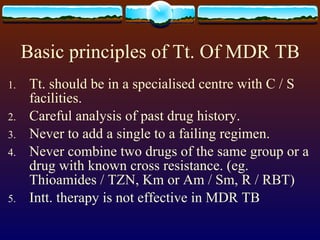
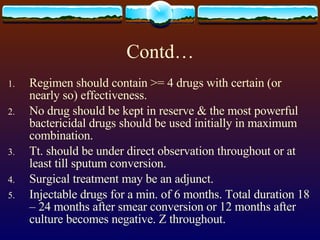
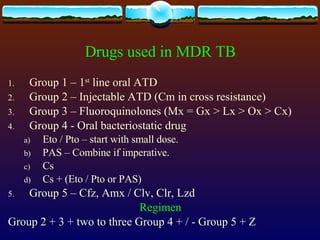
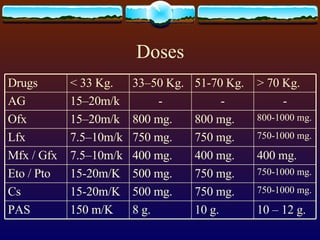
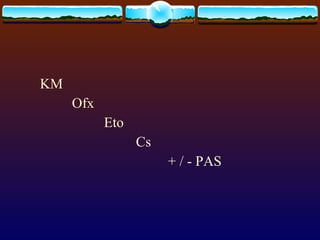
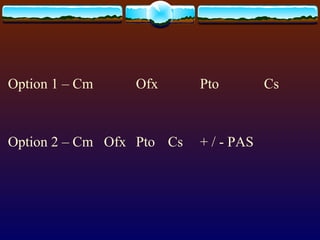
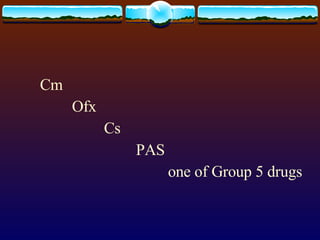
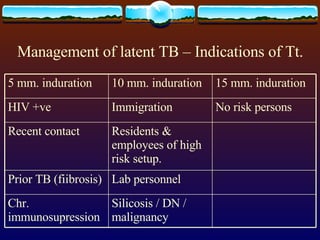
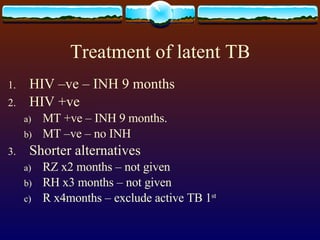
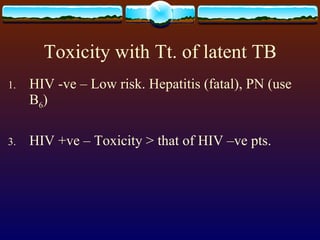
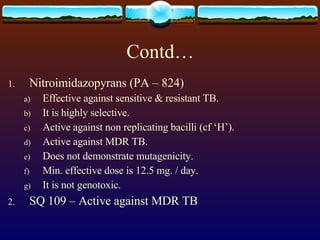
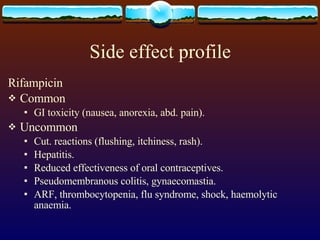
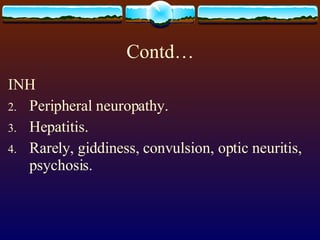
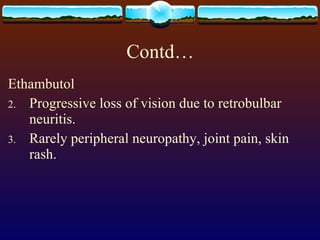
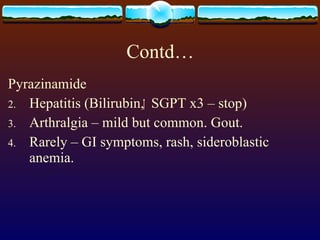
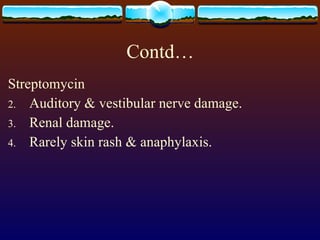
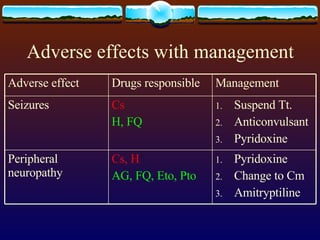
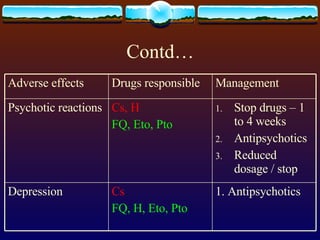
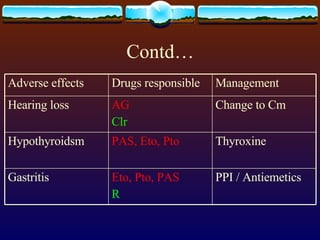
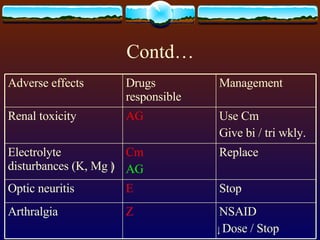
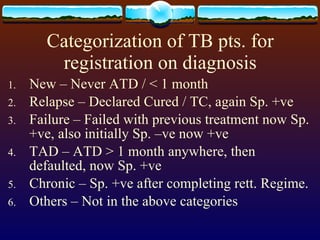
3. Guidelines are provided for treatment of different categories of tuberculosis patients, management of drug interactions and adverse effects, and regimens for multi-drug resistant cases.
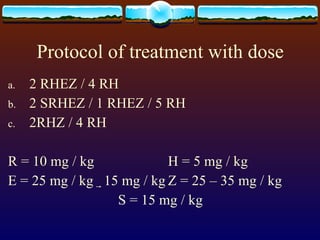

![Standardized treatment protocol Cat I – [2 (RHEZ) 3 / 4 (RH) 3 ] Cat II – [2 (SRHEZ) 3 / 1 (RHEZ) 3 / 5 (RHE) 3 ] Cat III – [2 (RHZ) 3 / 4 (RH) 3 ] Cat IV - Individualised](https://image.slidesharecdn.com/mot-358620-28093/85/MOT-19-320.jpg)