1. The document provides an outline for a presentation on assessing the musculoskeletal system. It covers anatomy, examination techniques, specific joints and tests.
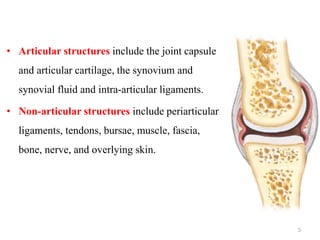
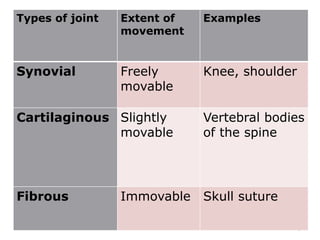
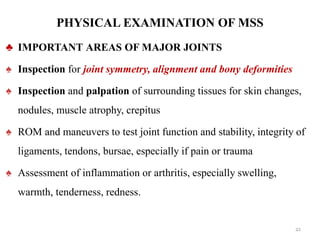
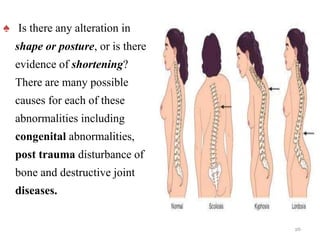
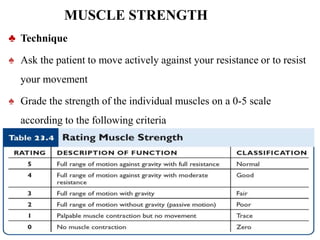
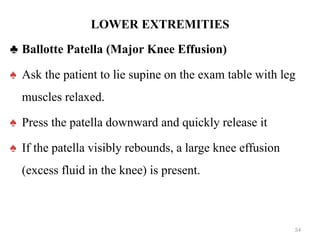
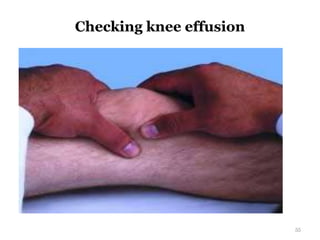
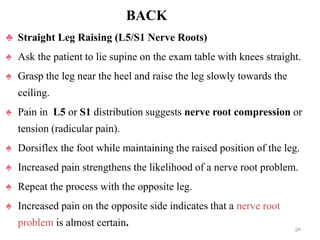
2. Key areas of assessment are inspection, palpation, range of motion testing, muscle strength and tone testing. Specific joints of the upper and lower body are examined.
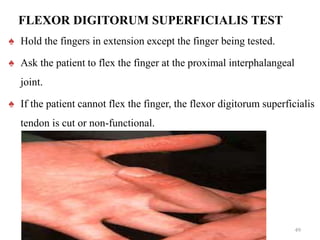
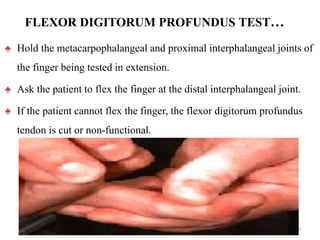
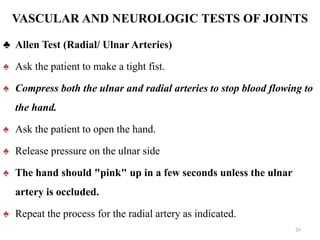
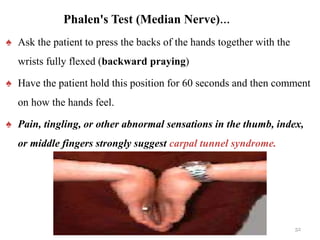
3. Special tests described include tests for the rotator cuff, nerves of the hand, and vascular supply of the hand. The goal is to evaluate for injuries, limitations, and other musculoskeletal abnormalities.