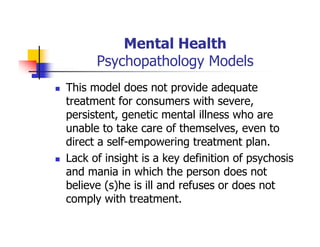
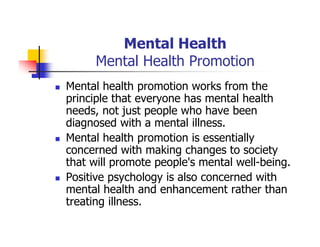
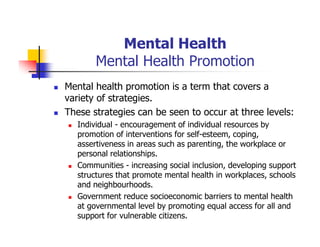
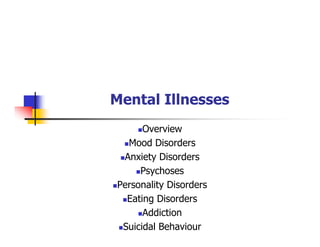
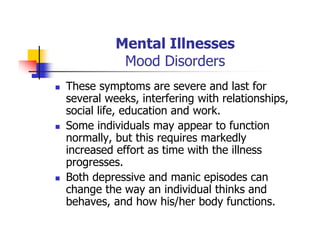
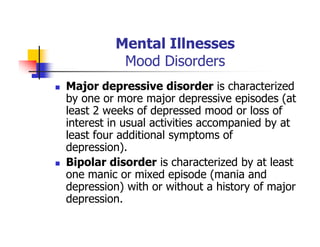
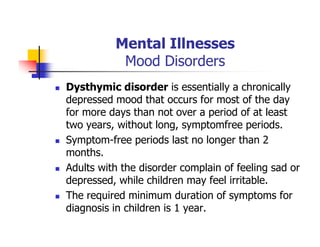
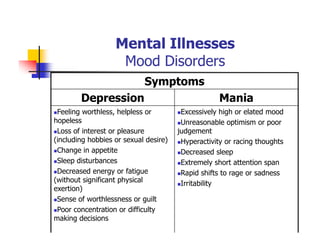
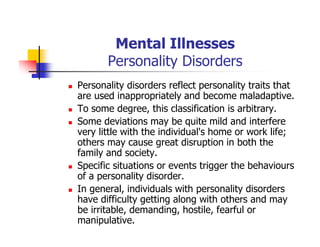
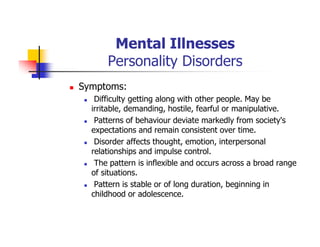
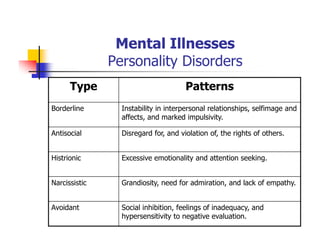
This document provides information about a Mental Health and Office Administration course taught by Dr. George Boghozian. It includes his education background and teaching experience. The document then summarizes key topics from the course, including definitions of mental health, models of psychopathology, and strategies for promoting positive mental health. Mental health is defined as emotional well-being and the ability to cope with life's stresses. The document discusses biological, environmental, and social factors that influence mental illnesses and notes that many such illnesses can be effectively treated.