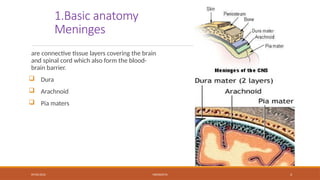
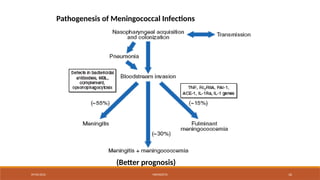
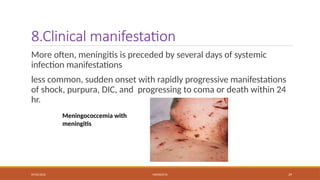
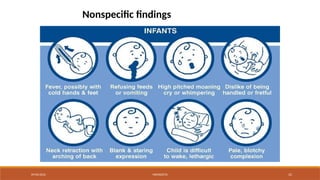
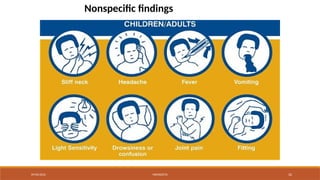
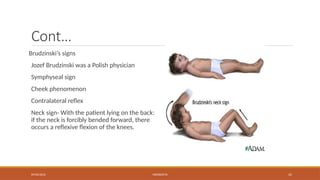
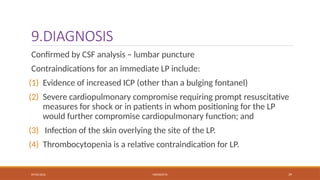
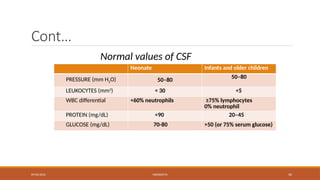
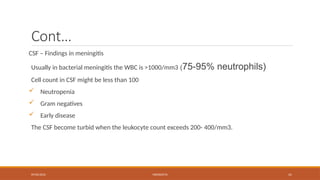
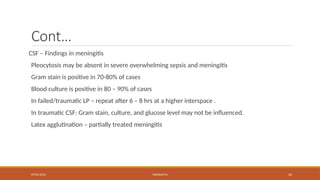
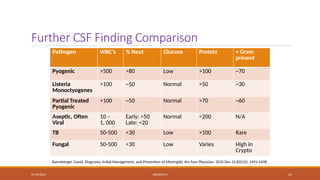
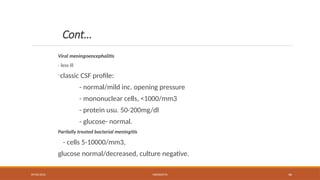
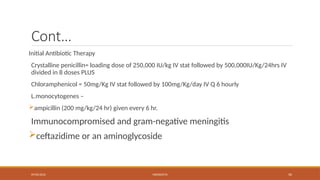
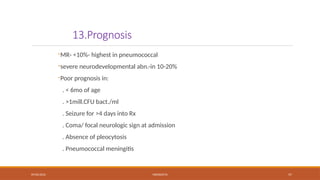
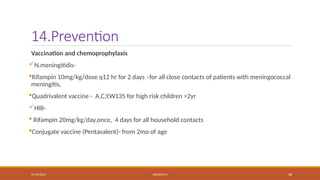
The document is a lecture on meningitis for medical students at Adigrat University, detailing causes, clinical manifestations, diagnosis, treatment, and complications of bacterial meningitis. It covers anatomy, epidemiology, pathogenesis, and various diagnostic criteria, emphasizing the importance of CSF analysis. Key points include the different causative organisms by age group, the significance of predisposing factors, and the necessity for immediate treatment to address organ failure and shock.