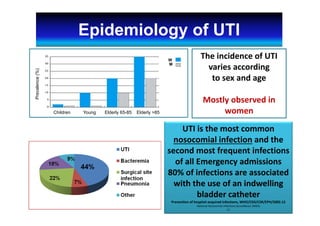
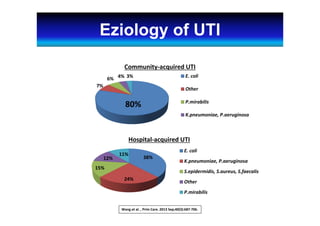
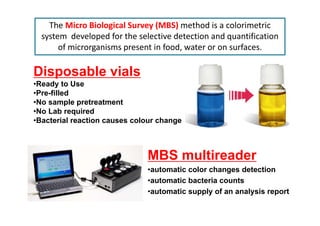
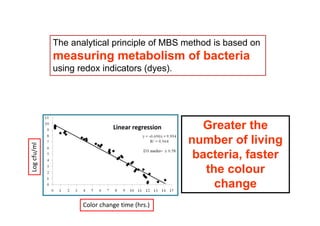
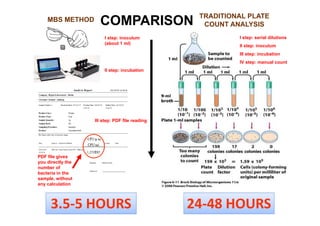
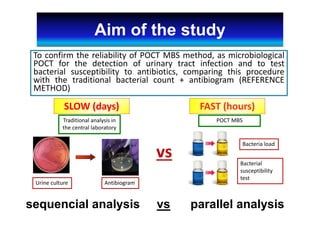
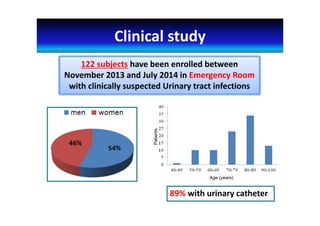
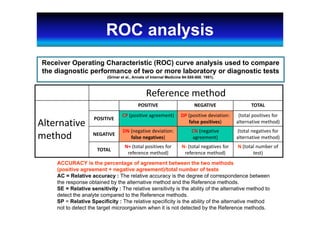
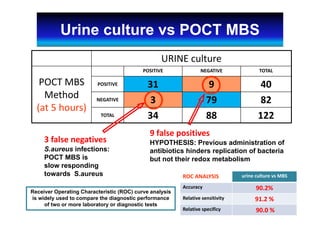
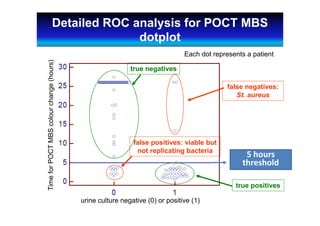
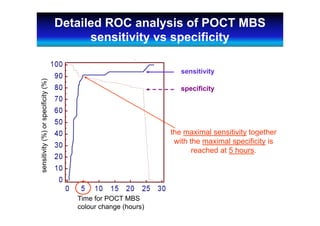
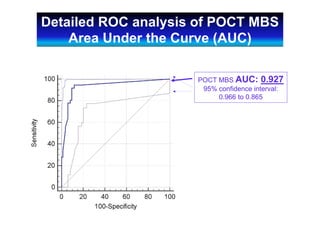
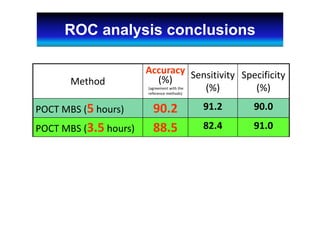
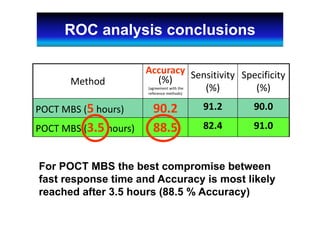
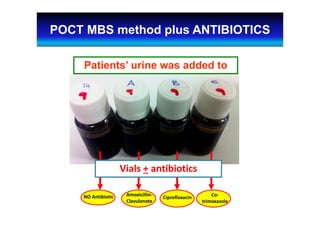
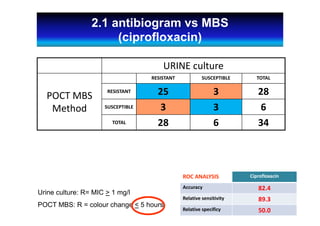
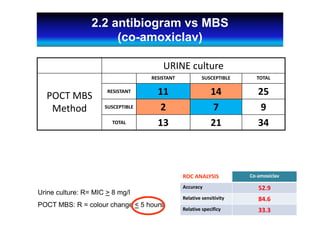
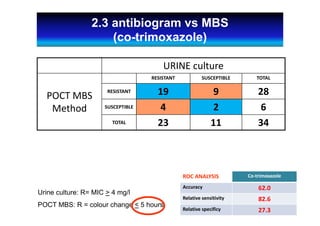
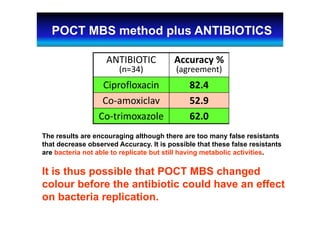
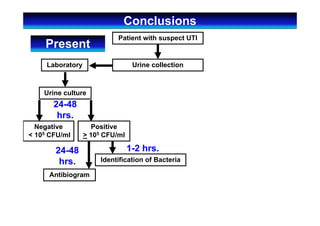
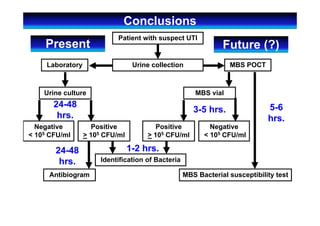
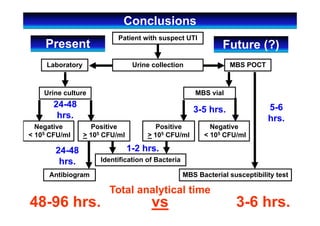
The document discusses using the Micro Biological Survey (MBS) method as a point-of-care test for rapidly diagnosing urinary tract infections. A clinical study found the MBS method identified urinary tract infections in 3-5 hours with 90.2% accuracy compared to traditional culture methods requiring 24-48 hours. While the MBS method showed high sensitivity at 91.2%, it had some false positive results, possibly due to antibiotics inhibiting bacterial growth but not metabolism. The MBS method also evaluated bacterial antibiotic susceptibility in 3-5 hours compared to 1-2 days for standard methods, though it had lower accuracy levels due to false resistant results where bacteria were non-replicating but metabolically active. Overall, the

![Acknowledgements
Partially supported by FILAS spa
(Regional Agency for the promotion of
development and innovation)
[grant number FILAS- RS-2009-1026]](https://image.slidesharecdn.com/mbsutipresentation-200111060207/85/Mbs-uti-presentation-32-320.jpg)