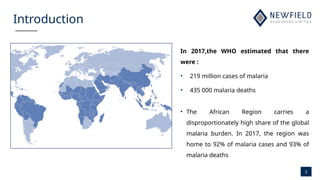
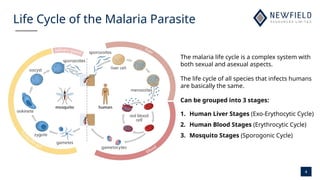
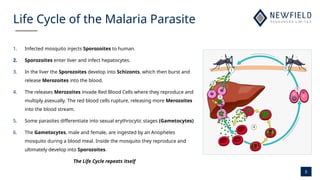
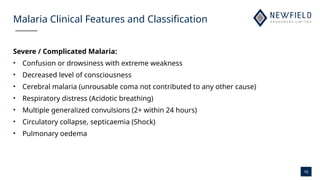
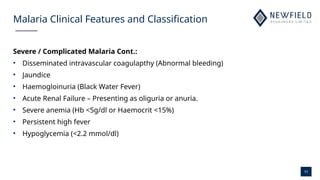
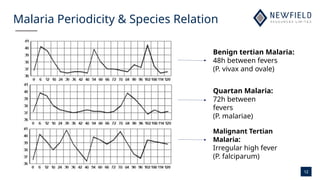
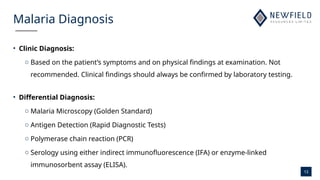
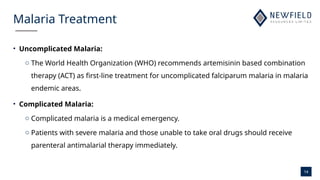
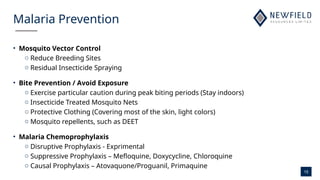
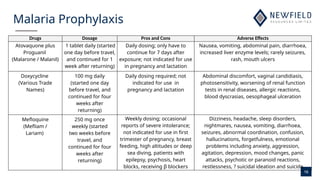
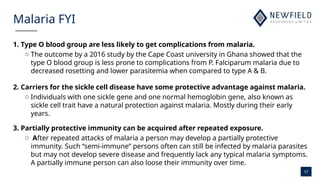
Malaria is a life-threatening disease caused by the Plasmodium genus, transmitted through infected Anopheles mosquitoes, with high prevalence and mortality primarily in Africa. The life cycle of the parasite involves stages in both human and mosquito hosts, and the disease presents varying symptoms from uncomplicated fevers to severe complications. Treatment includes artemisinin-based therapies for uncomplicated cases and immediate medical attention for severe cases, while prevention strategies focus on mosquito control and personal protective measures.