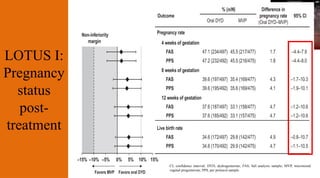
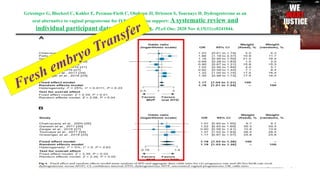
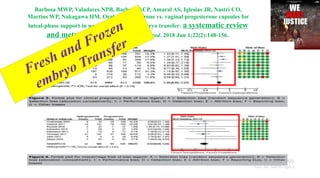
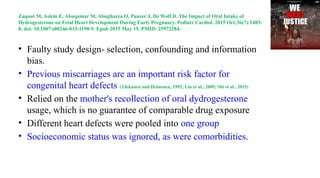
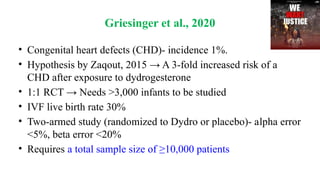
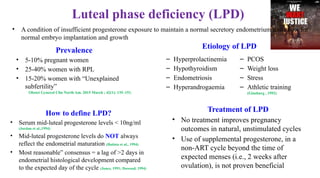
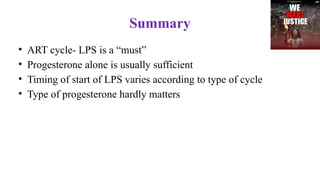
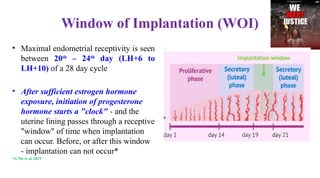
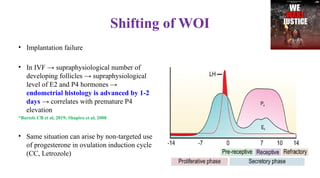
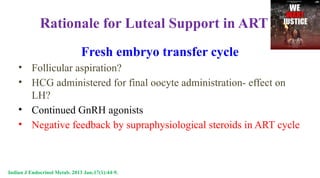
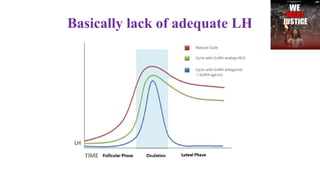
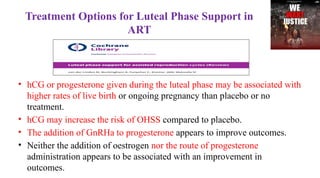
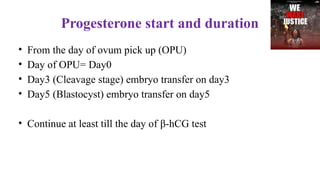
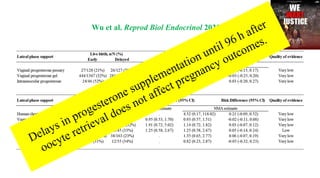
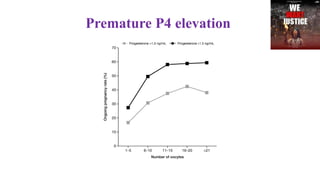
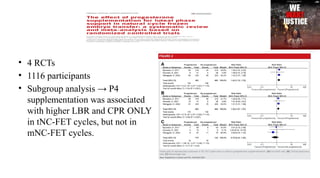
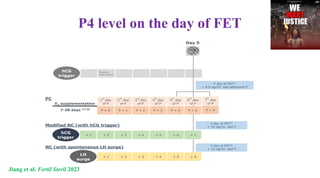
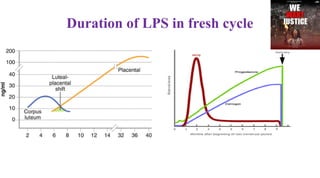
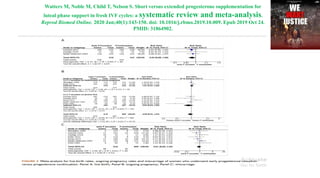
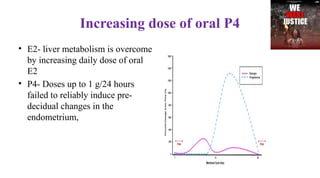
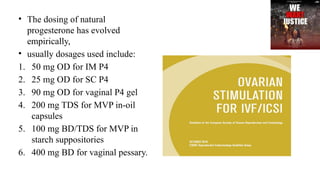
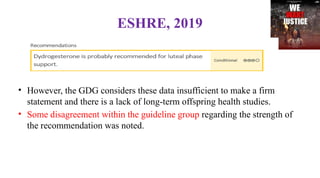
This document discusses the importance of luteal phase support (LPS) in assisted reproductive technology (ART) cycles, outlining the optimal timing and methods for progesterone administration to improve implantation success rates. It emphasizes the varying requirements for LPS based on the cycle type, efficacy of different progesterone formulations, and treatment protocols, while also addressing potential risks and outcomes associated with these treatments. Key findings suggest that timely and adequate LPS can significantly enhance live birth rates in ART, although the choice of progesterone may be less critical than previously thought.

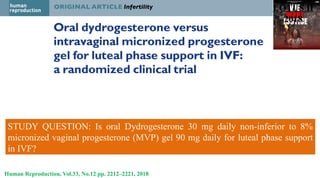
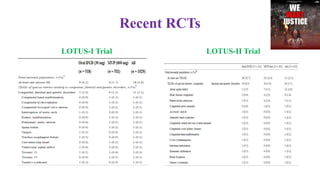
![STUDY QUESTION: Is oral Dydrogesterone 30 mg daily (10 mg three times daily [TID]) non-
inferior to micronized vaginal progesterone (MVP) 600 mg daily (200 mg TID) for luteal
support in in vitro fertilization (IVF), assessed by the presence of fetal heartbeats determined
by transvaginal ultrasound at 12 weeks of gestation?
LOTUS I
2017
Human Reproduction, Vol.32, No.5 pp. 1019–1027, 2017](https://image.slidesharecdn.com/lpspatnafinal-241027173630-1e7cddbb/85/Luteal-Phase-Support-29-320.jpg)