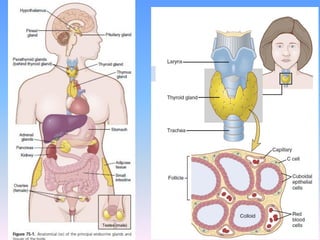
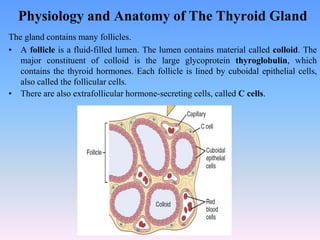
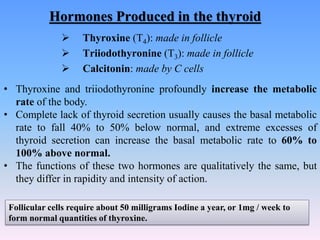
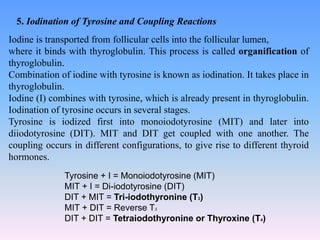
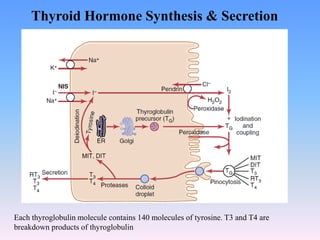
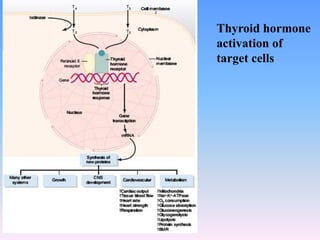
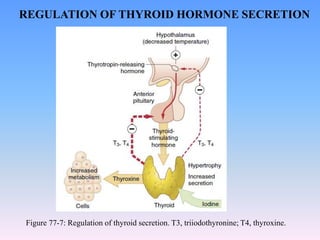
The document outlines the physiology and production of thyroid hormones, mainly thyroxine (T4) and triiodothyronine (T3), which are critical for regulating the body's metabolic rate. It explains the synthesis of these hormones from thyroglobulin within thyroid follicles, the process of iodide trapping, and the mechanisms by which these hormones are released and transported to tissues. Additionally, the regulation of thyroid hormone secretion through feedback mechanisms involving the hypothalamus and anterior pituitary gland is described.