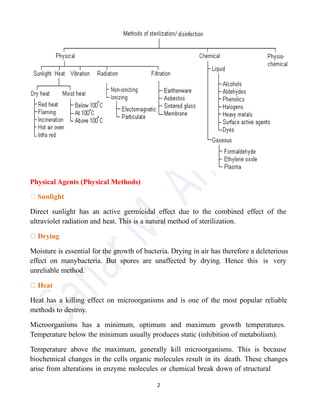
The document discusses sterilization and disinfection processes, defining sterilization as the complete elimination of all microorganisms, while disinfection refers to the reduction of pathogenic microbes on inanimate surfaces. It emphasizes various methods of sterilization, such as physical (heat, filtration, irradiation) and chemical means, as well as the distinctions between terms like antisepsis, decontamination, and sanitation. The text also outlines characteristics of ideal disinfectants and factors that influence their effectiveness.