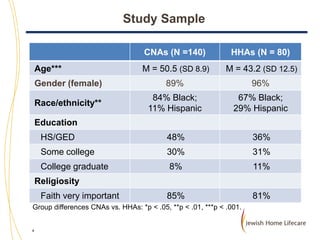
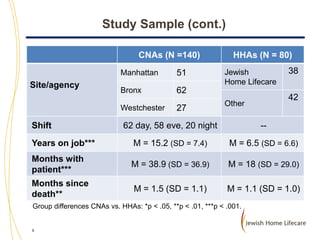
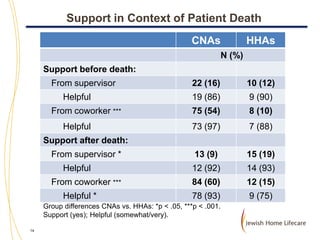
This study examined the experiences of direct care workers (CNAs and HHAs) with patient death, including their grief symptoms and needs for training and support. Key findings include:
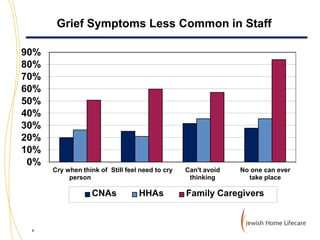
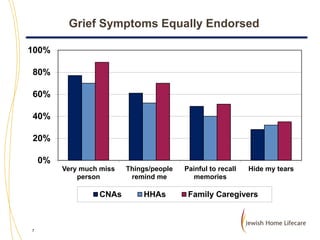
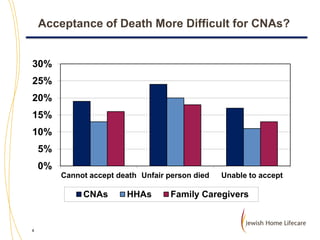
1) Both CNAs and HHAs reported grief symptoms similar to family caregivers after a patient's death, though some symptoms were less common in staff.
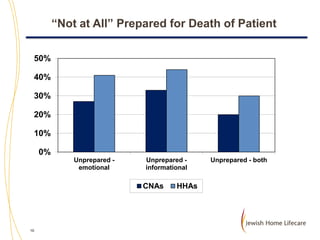
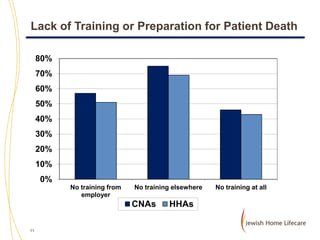
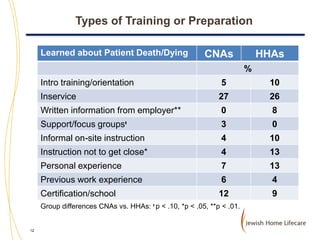
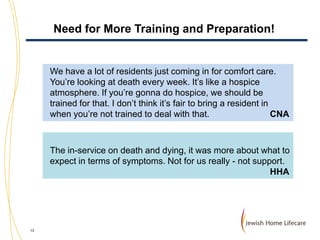
2) Most staff felt unprepared, both emotionally and informationally, for patient death due to little training.
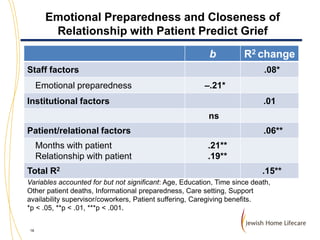
3) Greater emotional preparedness and closer relationships with patients predicted more intense grief.
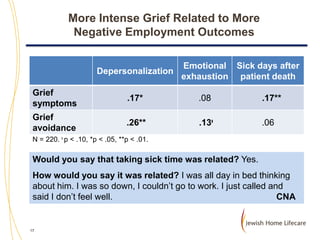
4) More intense grief was also related to more negative employment outcomes like increased emotional exhaustion.
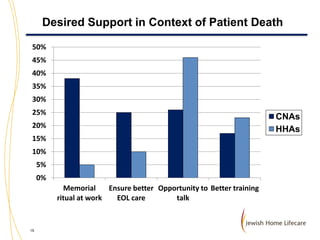
5) Staff desired more training, preparation, rituals to acknowledge
![Staff Appreciative of Opportunity to
Talk about Patient Death
This [study] is a good thing. Like now: it makes me feel like I’m kind of
getting real closure with [resident]. I got to say what I wanted to say.
Even if I’m not getting answers back, I’m letting out all I had here. If we
had this a long time ago, maybe new CNAs would act different with it.
CNA
For me, I’m grateful you did come. I wanted to tell someone [about
client]. You did inquire about her, and I was able to tell you. That’s the
part I’m gonna hold.
HHA
This interview makes me happy. It makes me happy that [JHL] wants to
know what is my emotional state, how the employee felt or how it
affected him/her. Truth is I did not do it for the money. This interview
has a value and I feel happy that [JHL] is concerned about me.
HHA
20](https://image.slidesharecdn.com/kathrinboerner-131113152058-phpapp02/85/Kathrin-Boerner-Direct-Care-Worker-s-Experiences-with-Patient-Death-Training-and-Support-20-320.jpg)