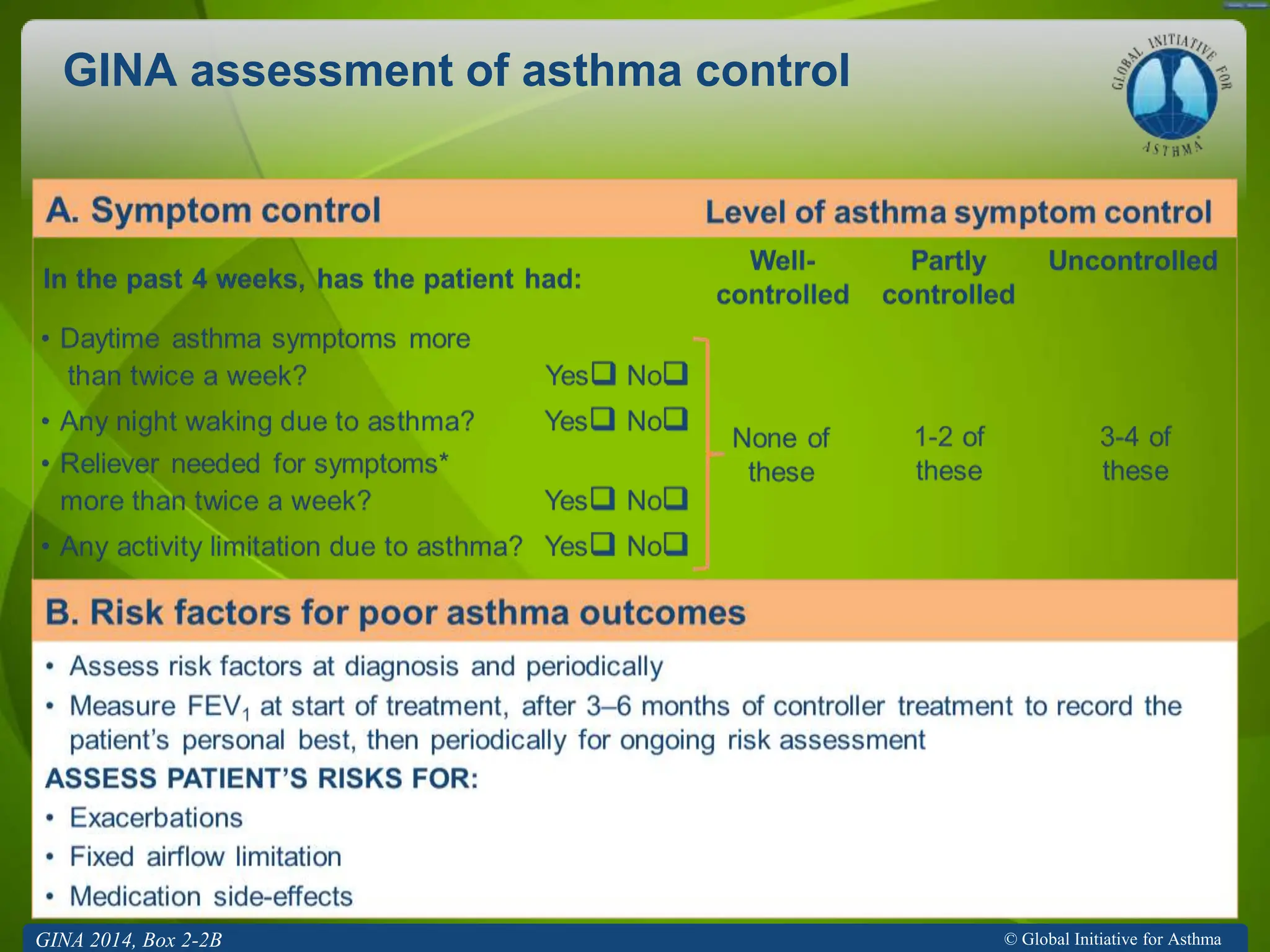
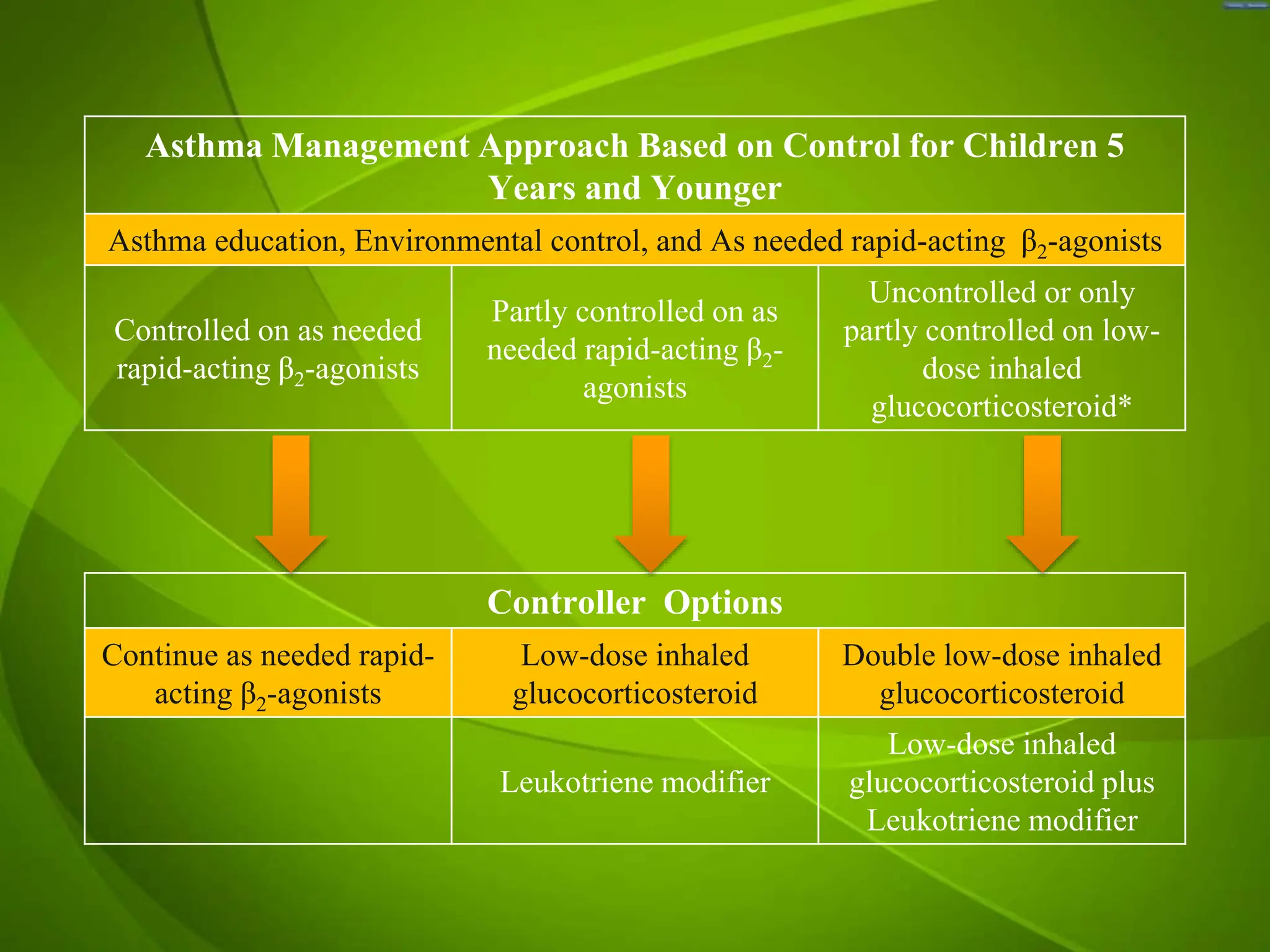
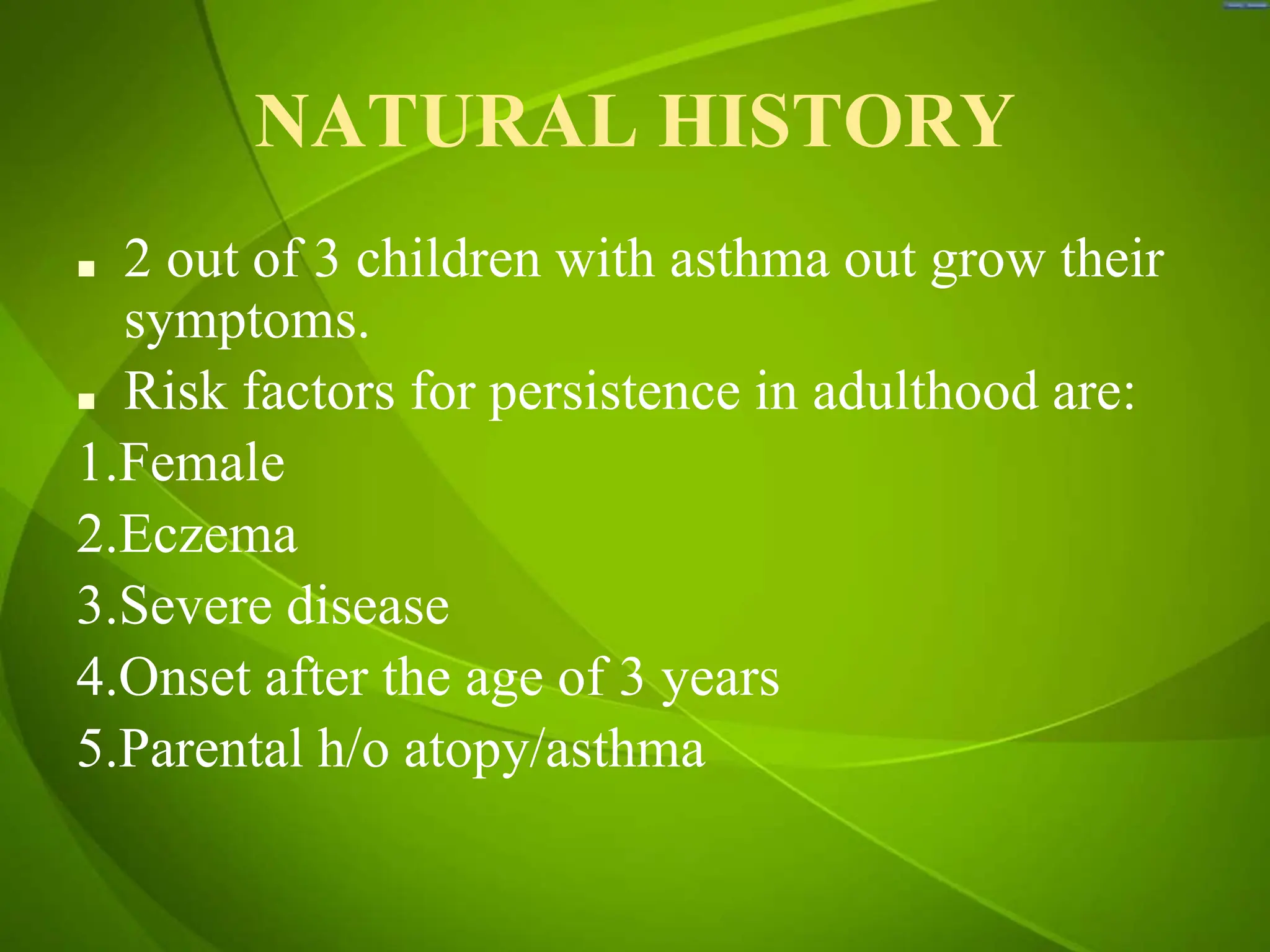
Childhood asthma is characterized by respiratory symptoms, including wheeze and cough, which vary in intensity and can result from different inflammatory patterns. Diagnosis is primarily clinical, based on symptom history and variable airflow limitation; comorbidities must be assessed to improve quality of life. Treatment focuses on patient education, pharmacotherapy, and symptom management through inhaled medications, with an emphasis on proper inhaler technique and monitoring of treatment efficacy.