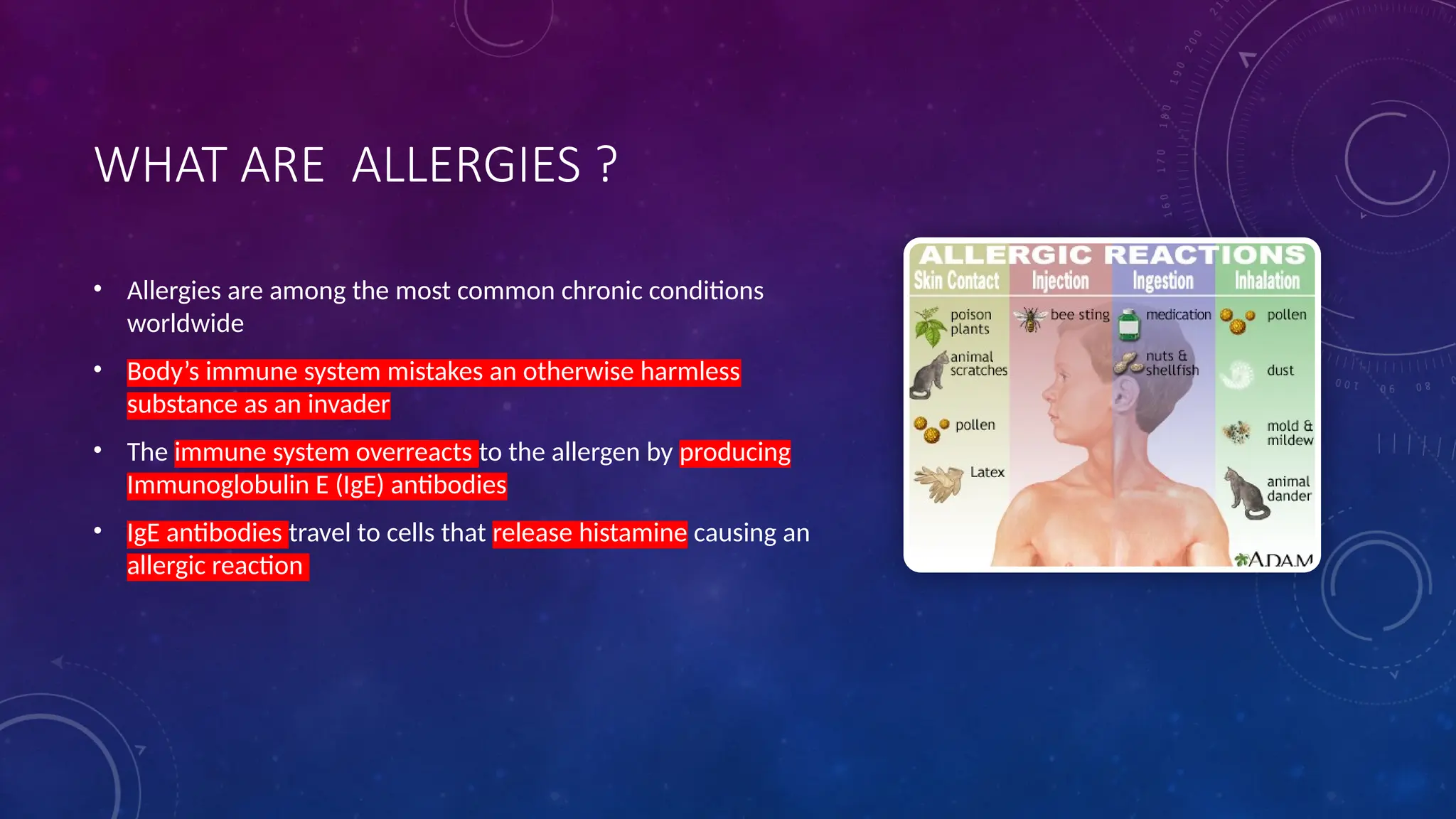
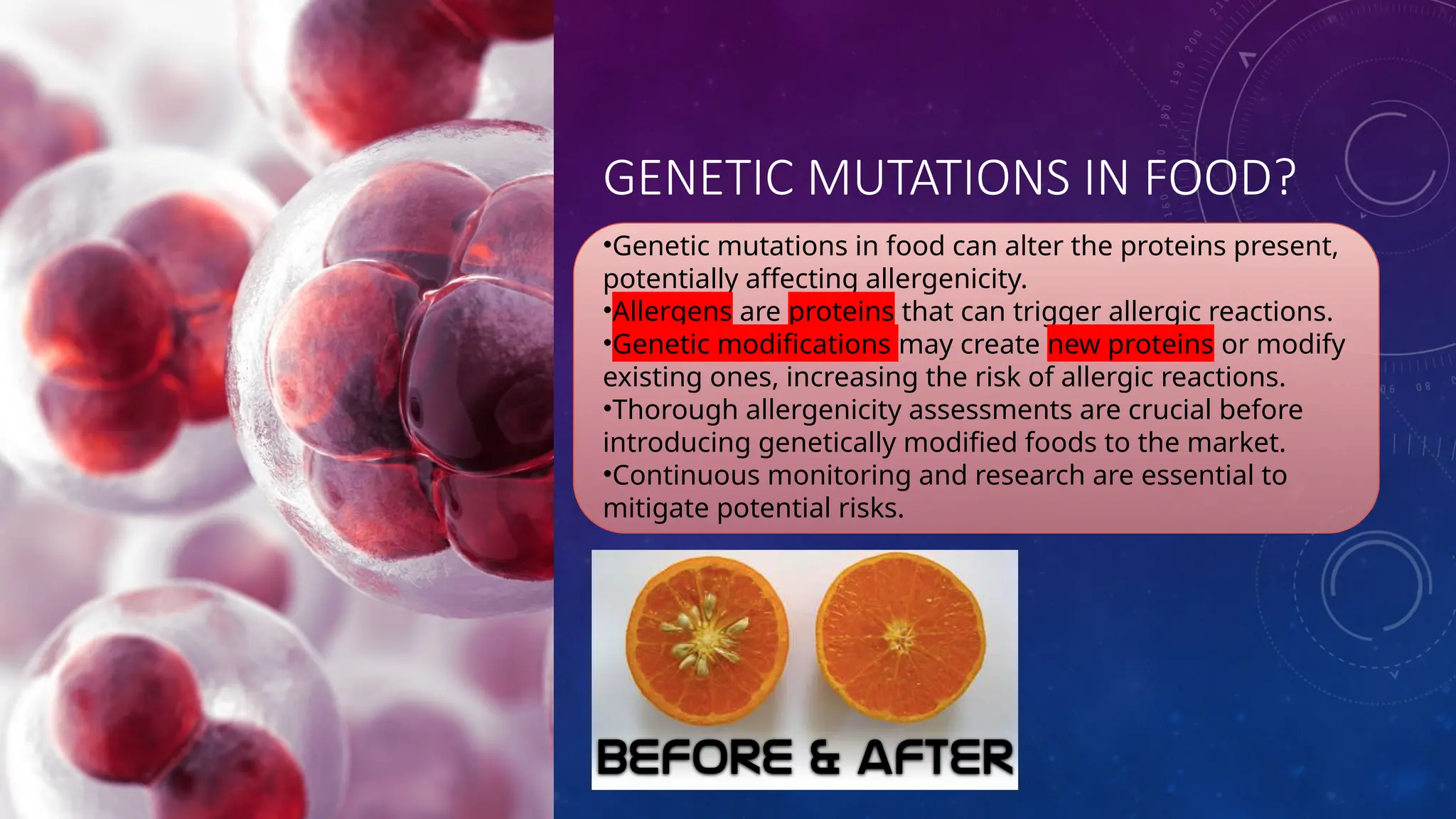
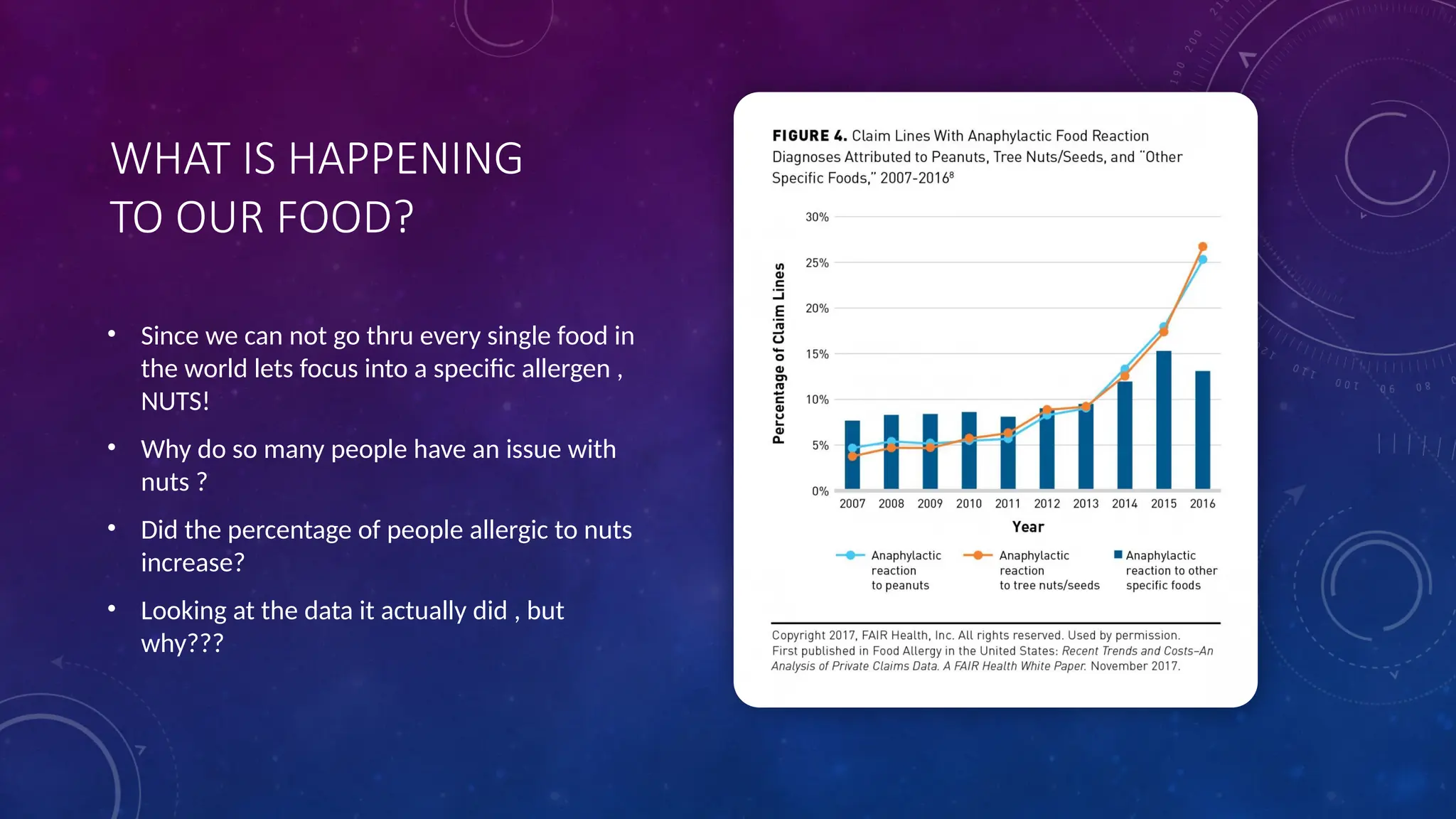
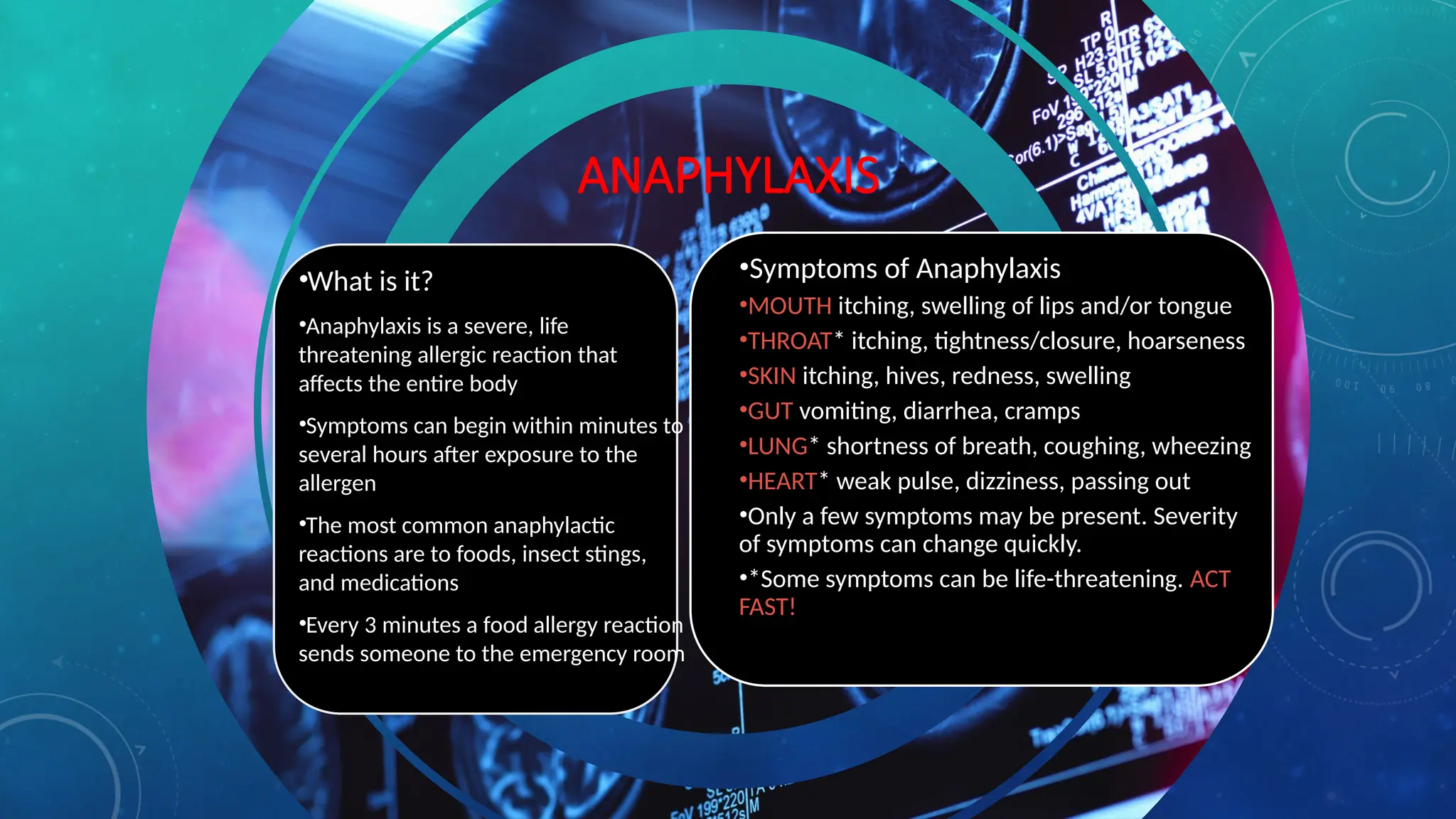
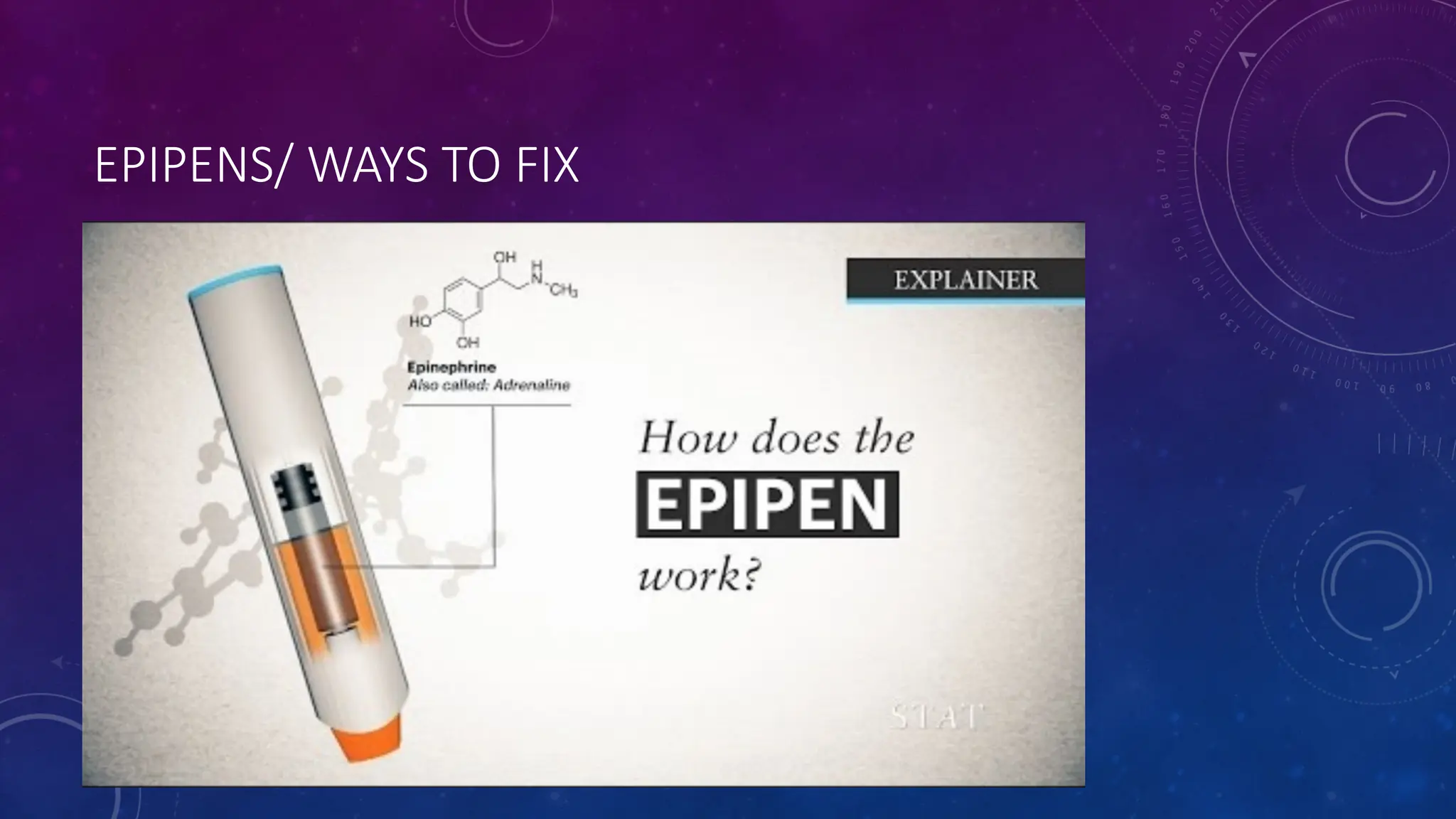
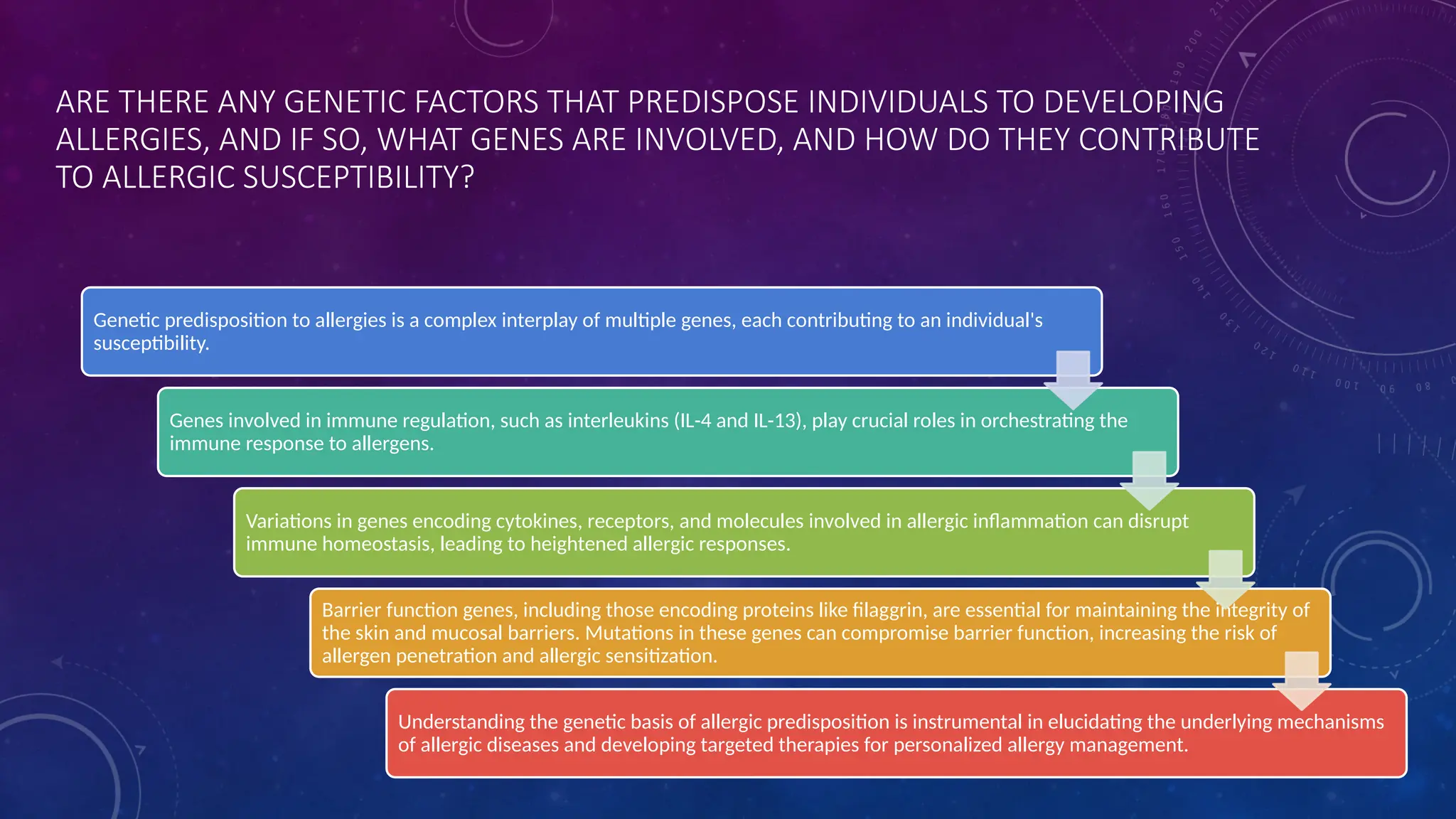
This document explores the complexities of allergies, detailing their physiological mechanisms, common allergens, and genetic and environmental factors that contribute to their development. It discusses the impact of allergies on quality of life and the importance of new diagnostic tools and management strategies, including immunotherapy and allergen avoidance techniques. The document emphasizes ongoing research into the microbiome's role in allergy susceptibility and the need for comprehensive strategies to mitigate allergic reactions.