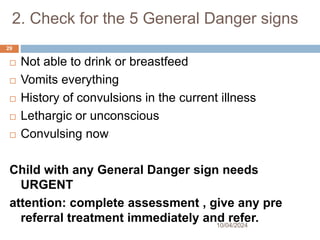
Check for general danger signs. Do you find any?
Health worker: No, I do not find any general danger signs in this case.
Case 2: Hassan
Hassan is 3 years old. He weighs 12 kg. His temperature is 39oC.
The health worker asked, 'What are the child's problems?' The mother said, 'Hassan
has been vomiting everything for 2 days.' This is Hassan's initial visit for this problem.