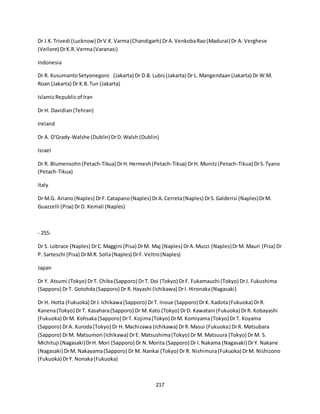
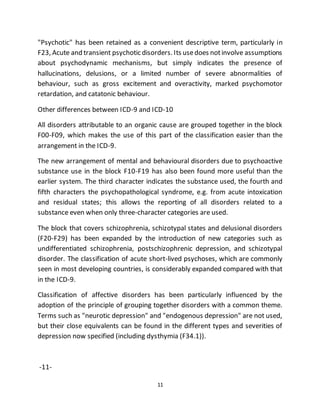
This document summarizes the development of the ICD-10 Classification of Mental and Behavioural Disorders by the World Health Organization over several decades through extensive international consultation and research. Major projects developed diagnostic assessment instruments and conducted field trials in over 40 countries to refine the diagnostic classifications and criteria. The final classification and this clinical guidelines publication reflect contributions from experts and institutions around the world and represent an international collaboration to improve psychiatric diagnosis worldwide.







![8
Chapter V, Mental and behavioural disorders, of ICD-10 is to be available in
severaldifferent versions for differentpurposes. This version, Clinical descriptions
and diagnostic guidelines, is intended for general clinical, educational and service
use. Diagnostic criteria for research has been produced for research purposes and
is designed to be used in conjunction with this book. The much shorter glossary
provided by Chapter V(F) for ICD-10 itself is suitable for use by coders or clerical
workers, and also serves as a reference point for compatibility with other
classifications; it is not recommended for use by mental health professionals.
Shorter and simpler versions of the classifications for use by primary health care
workers are now in preparation, as is a multiaxial scheme. Clinical descriptions
and diagnostic guidelines has been the starting point for the development of the
different versions, and the utmost care has been taken to avoid problems of
incompatibility between them.
Layout
It is important that users study this general introduction, and also read carefully
the additional introductory and explanatory texts at the beginning of several of
the individual categories. This is particularly important for F23.-(Acute and
transient psychotic disorders), and for the block F30-F39 (Mood [affective]
disorders). Because of the long-standing and notoriously difficult problems
associated with the description and classification of these disorders, special care
has been taken to explain how the classification has been approached.
For each disorder, a description is provided of the main clinical features, and also
of any important but less specific associated features. "Diagnostic guidelines" are
then provided in most cases, indicating the number and balance of symptoms
usually required before a confident diagnosis can be made. The guidelines are
worded so that a degree of flexibility is retained for diagnostic decisions in clinical
work, particularly in the situation where provisional diagnosis may have to be
made before the clinical picture is entirely clear or information is complete. To
avoid repetition, clinical descriptions and some general diagnostic guidelines are
provided for certain groups of disorders, in addition to those that relate only to
individual disorders.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-8-320.jpg)

![10
The chapter that dealt with mental disorders in ICD-9 had only 30 three-character
categories (290-319); Chapter V(F) of ICD-10 has 100 such categories. A
proportion of these categories has been left unused for the time being, so as to
allow the introduction of changes into the classification without the need to
redesign the entire system.
ICD-10 as a whole is designed to be a central ("core") classification for a family of
disease- and health-related classifications. Some members of the family of
classifications are derived by using a fifth or even sixth character to specify more
detail. In others, the categories are condensed to give broad groups suitable for
use, for instance, in primary health care or general medical practice. There is a
multiaxial presentation of Chapter V(F) of ICD-10 and a version for child
psychiatric practice and research. The "family" also includes classifications that
cover information not contained in the ICD, but having important medical or
health implications, e.g. the classification of impairments, disabilities and
handicaps, the classification of procedures in medicine, and the classification of
reasons for encounter between patients and health workers.
Neurosis and psychosis
The traditional division between neurosis and psychosis that was evident in ICD-9
(although deliberately left without any attempt to define these concepts) has not
been used in ICD-10. However, the term "neurotic" is still retained for occasional
use and occurs, for instance, in the heading of a major group (or block) of
disorders F40-F48, "Neurotic, stress-related and somatoform disorders". Except
for depressiveneurosis, mostof the disorders regarded as neuroses by those who
use the concept are to be found in this block,and the remainder are in the
subsequent blocks. Instead of following the neurotic-psychotic dichotomy, the
disorders are now arranged in groups according to major common themes or
descriptive likenesses, which makes for increased convenience of use. For
instance, cyclothymia (F34.0) is in the block F30-F39, Mood [affective] disorders,
rather than in F60-F69, Disorders of adult personality and behaviour; similarly, all
disorders associated with the use of psychoactive substances are grouped
together in F10-F19, regardless of their severity.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-10-320.jpg)








![20
Simple schizophrenia (F20.6) This category has been retained because of its
continued use in some countries, and because of the uncertainty about its nature
and its relationships to schizoid personality disorder and schizotypal disorder,
which will require additional information for resolution. The criteria proposed for
its differentiation highlight the problems of defining the mutual boundaries of this
whole group of disorders in practical terms.
Schizoaffectivedisorders (F25.-) The evidence at present available as to whether
schizoaffectivedisorders (F25.-) as defined in the ICD-10 should be placed in block
F20-F29 (schizophrenia, schizotypaland delusional disorders) or in F30-F39 (mood
[affective] disorders) is fairly evenly balanced. The final decision to place it in F20-
F29 was influenced by feedback from the field trials of the 1987 draft, and by
comments resulting from the worldwide circulation of the same draft to member
societies of the World Psychiatric Association. It is clear that widespread and
strong clinical traditions exist that favour its retention among schizophrenia and
delusional disorders. It is relevant to this discussion that, given a set of affective
symptoms, the addition of only mood-incongruent delusions is not sufficient to
change the diagnosis to a schizoaffective category. At least one typically
schizophrenic
-17-
symptom must be present with the affective symptoms during the same episode
of the disorder.
Mood [affective] disorders (F30-F39) It seems likely that psychiatrists will
continue to disagree about the classification of disorders of mood until methods
of dividing the clinical syndromes are developed that rely at least in part upon
physiological or biochemical measurement, rather than being limited as at
present to clinical descriptions of emotions and behaviour. As long as this
limitation persists, one of the major choices lies between a comparatively simple
classification with only a few degrees of severity, and one with greater details and
more subdivisions. The 1987 draft of ICD-10 used in the field trials had the merit](https://image.slidesharecdn.com/icd-161127112927/85/Icd-20-320.jpg)

![22
-18-
should encourage the collection of information that will lead to a better
understanding of their frequency and long-term course.
Agoraphobia and panic disorder There has been considerable debate recently as
to which of agoraphobia and panic disorder should be regarded as primary. From
an international and cross-cultural perspective, the amount and type of evidence
available does not appear to justify rejection of the still widely accepted notion
that the phobic disorder is best regarded as the prime disorder, with attacks of
panic usually indicating its severity.
Mixed categories of anxiety and depression Psychiatrists and others, especially
in developing countries, who see patients in primary health care services should
find particular use for F41.2 (mixed anxiety and depressivedisorder), F41.3 (other
mixed disorders), the various subdivisions of F43.2 (adjustment disorder), and
F44.7 (mixed dissociative [conversion] disorder). The purpose of these categories
is to facilitate the description of disorders manifest by a mixture of symptoms for
which a simpler and more traditional psychiatric label is not appropriate but
which nevertheless represent significantly common, severe states of distress and
interference with functioning. They also result in frequent referral to primary
care, medical and psychiatric services. Difficulties in using these categories
reliably may be encountered, but it is important to test them and - if necessary -
improve their definition.
Dissociative and somatoform disorders, in relation to hysteria The term
"hysteria" has notbeen used in the title for any disorder in Chapter V(F) of ICD-10
because of its many and varied shades of meaning. Instead, "dissociative" has
been preferred, to bring together disorders previously termed hysteria, of both
dissociative and conversion types. This is largely because patients with the
dissociative and conversion varieties often share a number of other
characteristics, and in addition they frequently exhibit both varieties at the same
or different times. It also seems reasonable to presume that the same (or very
similar) psychological mechanisms are common to both types of symptoms.
There appears to be widespread international acceptance of the usefulness of](https://image.slidesharecdn.com/icd-161127112927/85/Icd-22-320.jpg)


![25
emotionally unstable personality disorder (F60.3), again in the hope of stimulating
investigations.
Other disorders of adult personality and behaviour (F68) Two categories that
have been included here but were not present in ICD-9 are F68.0, elaboration of
physicalsymptoms for psychologicalreasons, and F68.1, intentionalproduction or
feigning of symptoms or disabilities, either physical or psychological [factitious
disorder]. Since these are, strictly speaking, disorders of role or illness behaviour,
it should be convenient for psychiatrists to have them grouped with other
disorders of adult behaviour. Together with malingering (Z76.5), which has always
been outside Chapter V of the ICD, the disorders from a trio of diagnoses often
need to be considered together. The crucial difference between the first two and
malingering is that the motivation for malingering is obvious and usually confined
to situations where personal danger, criminal sentencing, or large sums of money
are involved.
Mental retardation (F70-F79) The policy for Chapter V(F) of ICD-10 has always
been to deal with mental retardation as briefly and as simply as possible,
acknowledging that justice can be done to this topic only by means of a
comprehensive, possibly multiaxial, system. Such a system needs to be developed
separately, and work to produce appropriate proposals for international use is
now in progress.
-21-
Disorders with onset specific to childhood F80-F89 Disorders of psychological
development Disorders of childhood such as infantile autism and disintegrative
psychosis, classified in ICD-9 as psychoses, are now more appropriately contained
in F84.-, pervasive developmental disorders. While some uncertainty remains
about their nosological status, it has been considered that sufficient information
is now available to justify the inclusion of the syndromes of Rett and Asperger in
this group as specified disorders. Overactive disorder associated with mental
retardation and stereotyped movements (F84.4) has been included in spite of its](https://image.slidesharecdn.com/icd-161127112927/85/Icd-25-320.jpg)


![28
-24-
List of categories
F00-F09 Organic,includingsymptomatic,mentaldisorders
F00 DementiainAlzheimer'sdisease F00.0DementiainAlzheimer'sdiseasewithearlyonset
F00.1DementiainAlzheimer'sdisease withlate onsetF00.2DementiainAlzheimer'sdisease,atypical or
mixedtype F00.9DementiainAlzheimer'sdisease,unspecified
F01VasculardementiaF01.0Vasculardementiaof acute onsetF01.1Multi-infarctdementia
F01.2Subcortical vasculardementiaF01.3Mixedcortical andsubcortical vasculardementiaF01.8Other
vasculardementiaF01.9Vasculardementia,unspecified
F02Dementiainotherdiseasesclassifiedelsewhere F02.0DementiainPick'sdisease F02.1Dementiain
Creutzfeldt-Jakobdisease F02.2DementiainHuntington'sdisease F02.3DementiainParkinson'sdisease
F02.4Dementiainhumanimmunodeficiencyvirus[HIV] diseaseF02.8Dementiainotherspecified
diseasesclassifiedelsewhere
F03Unspecifieddementia
A fifthcharactermay be addedto specifydementiainF00-F03,as follows:
.x0 Withoutadditional symptoms.x1Othersymptoms,predominantlydelusional .x2Othersymptoms,
predominantlyhallucinatory.x3Othersymptoms,predominantlydepressive .x4Othermixedsymptoms
F04Organic amnesicsyndrome,notinducedbyalcohol andothersubstances
F05Delirium,notinducedbyalcohol andotherpsychoactive substancesF05.0Delirium, not
superimposedondementia,sodescribedF05.1Delirium, superimposedondementiaF05.8Other
deliriumF05.9Delirium, unspecified
F06Other mental disordersdue tobraindamage anddysfunctionandtophysical disease F06.0Organic
hallucinosisF06.1Organiccatatonicdisorder
-25-
F06.2Organic delusional[schizophrenia-like]disorderF06.3Organicmood[affective] disorders .30
Organicmanic disorder .31 Organicbipolaraffective disorder .32 Organicdepressive disorder .33
OrganicmixedaffectivedisorderF06.4OrganicanxietydisorderF06.5Organicdissociative disorder
F06.6Organic emotionallylabile [asthenic] disorder F06.7Mildcognitive disorderF06.8Otherspecified
mental disordersdue tobraindamage anddysfunctionandtophysical disease F06.9Unspecifiedmental
disorderdue tobraindamage and dysfunctionandtophysical disease](https://image.slidesharecdn.com/icd-161127112927/85/Icd-28-320.jpg)
![29
F07Personalityandbehavioural disorderdue tobraindisease,damage anddysfunctionF07.0Organic
personalitydisorderF07.1PostencephaliticsyndromeF07.2Postconcussional syndrome F07.8Other
organicpersonalityandbehavioural disorder due tobraindisease,damage anddysfunction
F09Unspecifiedorganicorsymptomaticmental disorder
-26-
F10--F19 Mental andbehavioural disordersdue to psychoactive substance use
F10.-Mental and behavioural disordersdue touse of alcohol
F11.-Mental and behavioural disordersdue touse of opioids
F12.-Mental and behavioural disordersdue touse of cannabinoids
F13.-Mental and behavioural disordersdue touse of sedativesorhypnotics
F14.-Mental and behavioural disordersdue touse of cocaine
F15.-Mental and behavioural disordersdue touse of otherstimulants,includingcaffeine
F16.-Mental and behavioural disordersdue touse of hallucinoeens
F17.-Mental and behavioural disordersdue touse of tobacco
F18.-Mental and behavioural disordersdue touse of volatile solvents
F19.-Mental and behavioural disordersdue tomultipledruguse anduse of otherpsychoactive
substances
Four- and five-charactercategoriesmaybe usedtospecifythe clinical conditions,asfollows:
F1x.0 Acute intoxication .00 Uncomplicated .01 Withtrauma or otherbodilyinjury .02 Withother
medical complications .03With delirium .04 Withperceptual distortions .05 Withcoma .06 With
convulsions .07Pathological intoxication
F1x.1 Harmful use
F1x.2 Dependence syndrome .20 Currentlyabstinent .21 Currentlyabstinent,butina protected
environment .22 Currentlyona clinicallysupervised maintenance orreplacementregime [controlled
dependence] .23 Currentlyabstinent,butreceivingtreatment withaversive orblockingdrugs .24
Currentlyusingthe substance [active
-27-](https://image.slidesharecdn.com/icd-161127112927/85/Icd-29-320.jpg)
![30
dependence] .25 Continuoususe .26Episodicuse [dipsomania]
F1x.3 Withdrawal state .30 Uncomplicated .31With convulsions
F1x.4 Withdrawal state withdelirium .40Withoutconvulsions .41With convulsions
F1x.5 Psychoticdisorder .50 Schizophrenia-like .51 Predominantlydelusional .52 Predominantly
hallucinatory .53Predominantlypolymorphic .54 Predominantlydepressive symptoms .55
Predominantlymanicsymptoms .56Mixed
F1x.6 Amnesicsyndrome
F1x.7 Residual andlate-onsetpsychoticdisorder .70 Flashbacks .71 Personalityorbehaviourdisorder
.72 Residual affectivedisorder .73 Dementia .74 Otherpersistingcognitiveimpairment .75 Late-onset
psychoticdisorder
F1x.8 Othermental andbehavioural disorders
F1x.9 Unspecifiedmental andbehavioural disorder
-28-
F20-F29 Schizophrenia, schizotypal anddelusional disorders
F20 Schizophrenia F20.0 Paranoidschizophrenia F20.1 Hebephrenicschizophrenia F20.2 Catatonic
schizophrenia F20.3 Undifferentiatedschizophrenia F20.4 Post-schizophrenicdepression F20.5
Residual schizophrenia F20.6 Simple schizophrenia F20.8Other schizophrenia F20.9 Schizophrenia,
unspecified
A fifthcharactermay be usedto classifycourse:.x0Continuous.x1Episodicwithprogressive deficit.x2
Episodicwithstable deficit.x3Episodicremittent.x4Incomplete remission.x5Complete remission.x6
Other.x9 Course uncertain,periodof observationtooshort
F21 Schizotypal disorder
F22 Persistentdelusionaldisorders F22.0 Delusional disorder F22.8 Otherpersistentdelusional
disorders F22.9 Persistentdelusional disorder,unspecified
F23 Acute and transientpsychoticdisorders F23.0 Acute polymorphicpsychoticdisorderwithout
symptomsof schizophrenia F23.1Acute polymorphicpsychoticdisorderwithsymptomsof
schizophrenia F23.2 Acute schizophrenia-likepsychoticdisorder F23.3 Otheracute predominantly
delusionalpsychoticdisorders F23.8 Otheracute andtransientpsychoticdisorders F23.9Acute and
transientpsychoticdisordersunspecified](https://image.slidesharecdn.com/icd-161127112927/85/Icd-30-320.jpg)
![31
A fifthcharactermay be usedto identifythe presence orabsence of associatedacute stress:.x0Without
associatedacute stress.x1With associatedacute stress
-29-
F24 Induceddelusional disorder
F25 Schizoaffective disorders F25.0 Schizoaffectivedisorder,manictype F25.1 Schizoaffectivedisorder,
depressivetype F25.2 Schizoaffective disorder,mixedtype F25.8 Otherschizoaffective disorders F25.9
Schizoaffective disorder,unspecified
F28 Othernonorganicpsychoticdisorders
F29 Unspecifiednonorganicpsychosis
-30-
F30-F39 Mood [affective] disorders
Overviewof thisblock F30 Manic episode F30.0Hypomania F30.1 Mania withoutpsychoticsymptoms
F30.2 Mania withpsychoticsymptoms F30.8 Othermanicepisodes F30.9 Manic episode,unspecified
F31 Bipolaraffective disorder F31.0 Bipolaraffective disorder,currentepisode hypomanic F31.1 Bipolar
affective disorder,currentepisodemanicwithoutpsychoticsymptoms F31.2 Bipolaraffective disorder,
currentepisode manicwithpsychoticsymptoms F31.3Bipolaraffectivedisorder,currentepisode mild
or moderate depression .30 Withoutsomaticsyndrome .31 Withsomaticsyndrome F31.4 Bipolar
affective disorder,currentepisodesevere depressionwithoutpsychoticsymptoms F31.5 Bipolar
affective disorder,currentepisodesevere depressionwithpsychoticsymptoms F31.6 Bipolaraffective
disorder,currentepisodemixed F31.7 Bipolaraffectivedisorder,currentlyinremission F31.8Other
bipolaraffectivedisorders F31.9 Bipolaraffectivedisorder,unspecified
F32 Depressiveepisode F32.0 Milddepressive episode .00 Withoutsomaticsyndrome .01 With
somaticsyndrome F32.1 Moderate depressive episode .10 Without somaticsyndrome .11 With
somaticsyndrome F32.2 Severe depressive episode withoutpsychoticsymptoms F32.3 Severe
depressiveepisodewithpsychoticsymptoms F32.8Otherdepressive episodes F32.9 Depressive
episode,unspecified
-31-
F33 Recurrentdepressive disorder F33.0Recurrentdepressivedisorder,currentepisode mild .00
Withoutsomaticsyndrome .01 Withsomaticsyndrome F33.1 Recurrentdepressive disorder,current](https://image.slidesharecdn.com/icd-161127112927/85/Icd-31-320.jpg)
![32
episode moderate .10 Withoutsomaticsyndrome .11 With somaticsyndrome F33.2 Recurrent
depressivedisorder,currentepisode severewithoutpsychoticsymptoms F33.3 Recurrentdepressive
disorder,currentepisodesevere withpsychoticsymptoms F33.4 Recurrentdepressive disorder,
currentlyinremission F33.8Otherrecurrentdepressivedisorders F33.9 Recurrentdepressive disorder,
unspecified
F34 Persistentmood[affective] disorders F34.0Cyclothymia F34.1 Dysthymia F34.8 Otherpersistent
mood[affective] disorders F34.9Persistent mood[affective] disorder,unspecified F38 Othermood
[affective] disorders F38.0Othersingle mood[affective] disorders .00 Mixedaffectiveepisode F38.1
Otherrecurrentmood[affective] disorders .10 Recurrentbrief depressive disorder F38.8 Other
specifiedmood[affective] disorders
F39 Unspecifiedmood[affective] disorder
-32-
F40-F48 Neurotic,stress-relatedandsomatoformdisorders F40 Phobicanxietydisorders F40.0
Agoraphobia .00 Withoutpanicdisorder .01 Withpanic disorder F40.1 Social phobias F40.2 Specific
(isolated)phobias F40.8 Otherphobicanxietydisorders F40.9 Phobicanxietydisorder,unspecified
F41 Otheranxietydisorders F41.0 Panicdisorder[episodicparoxysmal anxiety] F41.1Generalized
anxietydisorder F41.2 Mixedanxietyanddepressivedisorder F41.3 Othermixedanxietydisorders
F41.8 Otherspecifiedanxietydisorders F41.9 Anxietydisorder,unspecified
F42 Obsessive- compulsive disorder F42.0 Predominantlyobsessionalthoughtsorruminations F42.1
Predominantlycompulsive acts[obsessionalrituals] F42.2 Mixedobsessional thoughtsandacts F42.8
Otherobsessive - compulsivedisorders F42.9 Obsessive - compulsive disorder,unspecified
F43 Reactiontosevere stress,andadjustmentdisorders F43.0Acute stressreaction F43.1 Post-
traumaticstressdisorder F43.2 Adjustmentdisorders .20 Brief depressive reaction .21 Prolonged
depressivereaction .22 Mixedanxietyanddepressive reaction .23 Withpredominantdisturbanceof
otheremotions .24 With predominantdisturbance of conduct .25 With mixeddisturbance of
emotionsandconduct .28 With otherspecifiedpredominantsymptoms F43.8Otherreactionsto
severe stress F43.9 Reactiontosevere stress,unspecified
F44 Dissociative [conversion] disorders F44.0Dissociative amnesia F44.1 Dissociative fugue F44.2
Dissociative stupor F44.3Trance and possessiondisorders F44.4 Dissociative motordisorders
-33-
F44.5 Dissociative convulsions](https://image.slidesharecdn.com/icd-161127112927/85/Icd-32-320.jpg)
![33
F44.6 Dissociative anaesthesiaandsensoryloss F44.7 Mixeddissociative [conversion] disorders F44.8
Otherdissociative[conversion] disorders .80 Ganser's syndrome .81 Multiple personalitydisorder .82
Transientdissociative [conversion]disordersoccurringinchildhood and adolescence .88 Other
specifieddissociative [conversion]disorders F44.9 Dissociative[conversion] disorder,unspecified
F45 Somatoformdisorders F45.0Somatizationdisorder F45.1Undifferentiatedsomatoformdisorder
F45.2 Hypochondriacal disorder F45.3 Somatoformautonomicdysfunction .30 Heart and
cardiovascularsystem .31 Upper gastrointestinal tract .32 Lowergastrointestinaltract .33
Respiratorysystem .34 Genitourinarysystem .38 Otherorgan or system F45.4 Persistentsomatoform
paindisorder F45.8 Othersomatoformdisorders F45.9Somatoformdisorder,unspecified
F48 Otherneuroticdisorders F48.0 Neurasthenia F48.1 Depersonalization - derealizationsyndrome
F48.8 Otherspecifiedneuroticdisorders F48.9Neuroticdisorder,unspecified
-34-
F50-F59 Behavioural syndromesassociatedwithphysiological disturbancesandphysical factors F50
Eatingdisorders F50.0 Anorexianervosa F50.1 Atypical anorexianervosa F50.2 Bulimianervosa F50.3
Atypical bulimianervosa F50.4 Overeatingassociated withotherpsychological disturbances F50.5
Vomitingassociatedwithotherpsychological disturbances F50.8Othereatingdisorders F50.9 Eating
disorder,unspecified
F51 Nonorganicsleepdisorders F51.0Nonorganicinsomnia F51.1 Nonorganichypersomnia F51.2
Nonorganicdisorderof the sleep-wake schedule F51.3 Sleepwalking[somnambulism] F51.4 Sleep
terrors[nightterrors] F51.5 Nightmares F51.8 Othernonorganicsleepdisorders F51.9 Nonorganic
sleepdisorder,unspecified
F52 Sexual dysfunction,notcausedbyorganicdisorderordisease F52.0 Lack or lossof sexual desire
F52.1 Sexual aversionandlackof sexual enjoyment .10 Sexual aversion .11 Lack of sexual enjoyment
F52.2 Failure of genital response F52.3 Orgasmicdysfunction F52.4Premature ejaculation F52.5
Nonorganicvaginismus F52.6 Nonorganicdyspareunia F52.7 Excessive sexual drive F52.8 Othersexual
dysfunction,notcausedbyorganicdisordersordisease F52.9 Unspecifiedsexual dysfunction,not
causedby organicdisorderordisease F53Mental and behavioural disordersassociatedwiththe
puerperium, notelsewhereclassified F53.0Mild mental andbehavioural disordersassociatedwiththe
puerperium, notelsewhereclassified
-35-
F53.1 Severe mental andbehavioural disordersassociatedwiththe puerperium, notelsewhere
classified F53.8 Othermental andbehavioural disordersassociatedwiththe puerperium, notelsewhere
classified F53.9 Puerperal mental disorder,unspecified](https://image.slidesharecdn.com/icd-161127112927/85/Icd-33-320.jpg)
![34
F54Psychological andbehavioural factorsassociatedwithdisordersordiseasesclassifiedelsewhere
F55 Abuse of non-dependence-producingsubstances F55.0 Antidepressants F55.1 Laxatives F55.2
Analgesics F55.3 Antacids F55.4 Vitamins F55.5 Steroidsorhormones F55.6 Specificherbal orfolk
remedies F55.8Othersubstancesthatdo not produce dependence F55.9Unspecified
F59Unspecifiedbehavioural syndromesassociatedwithphysiological disturbancesandphysical factors
-36-
F60-F69 Disordersof adultpersonalityandbehaviour
F60 Specificpersonalitydisorders F60.0 Paranoidpersonalitydisorder F60.1 Schizoidpersonality
disorder F60.2 Dissocial personalitydisorder F60.3 Emotionallyunstable personalitydisorder .30
Impulsive type .31 Borderline type F60.4Histrionicpersonalitydisorder F60.5 Anankasticpersonality
disorder F60.6 Anxious[avoidant]personalitydisorder F60.7 Dependentpersonalitydisorder F60.8
Otherspecificpersonalitydisorders F60.9 Personalitydisorder,unspecified
F61 Mixedandotherpersonalitydisorders F61.0 Mixedpersonalitydisorders F61.1Troublesome
personalitychanges
F62 Enduringpersonalitychanges,notattributabletobraindamage anddisease F62.0 Enduring
personalitychange aftercatastrophicexperience F62.1 Enduringpersonalitychange afterpsychiatric
illness F62.8Otherenduringpersonalitychanges F62.9Enduringpersonalitychange,unspecified
F63 Habitand impulse disorders F63.0 Pathological gambling F63.1Pathological fire-setting
[pyromania] F63.2 Pathological stealing[kleptomania] F63.3 Trichotillomania F63.8 Otherhabitand
impulse disorders F63.9Habit and impulse disorder,unspecified
F64 Genderidentitydisorders F64.0 Transsexualism F64.1 Dual-role transvestism F64.2 Gender
identitydisorderof childhood F64.8 Othergenderidentitydisorders F64.9 Genderidentitydisorder,
unspecified
F65 Disordersof sexual preference F65.0 Fetishism F65.1 Fetishistictransvestism F65.2Exhibitionism
F65.3 Voyeurism F65.4Paedophilia
-37-
F65.5 Sadomasochism F65.6 Multiple disordersof sexual preference F65.8Otherdisordersof sexual
preference F65.9Disorderof sexual preference,unspecified
F66 Psychological andbehavioural disordersassociatedwithsexual developmentandorientation F66.0
Sexual maturationdisorder F66.1 Egodystonicsexual orientation F66.2Sexual relationshipdisorder](https://image.slidesharecdn.com/icd-161127112927/85/Icd-34-320.jpg)
![35
F66.8 Otherpsychosexual developmentdisorders F66.9 Psychosexual developmentdisorder,
unspecified
A fifthcharactermay be usedto indicate associationwith:.x0Heterosexuality.x1Homosexuality.x2
Bisexuality.x8Other,includingprepubertal
F68 Otherdisordersof adultpersonalityandbehaviour F68.0 Elaborationof physical symptomsfor
psychological reasons F68.1 Intentional productionorfeigningof symptomsordisabilities,either
physical orpsychological [factitiousdisorder] F68.8 Otherspecifieddisordersof adultpersonalityand
behaviour
F69 Unspecifieddisorderof adultpersonalityandbehaviour
-38-
F70-F79 Mental retardation
F70 Mildmental retardation
F71 Moderate mental retardation
F72 Severe mental retardation
F73 Profoundmental retardation
F78 Othermental retardation
F79 Unspecifiedmental retardation
A fourthcharacter maybe usedto specifythe extentof associatedbehavioural impairment:
F7x.0 No,or minimal,impairmentof behaviour F7x.1Significantimpairmentof behaviourrequiring
attentionortreatment F7x.8 Otherimpairmentsof behaviour F7x.9Withoutmentionof impairmentof
behaviour
-39-
F80-F89 Disordersof psychological development
F80 Specificdevelopmental disordersof speechandlanguage F80.0 Specificspeecharticulation
disorder F80.1 Expressivelanguage disorder F80.2 Receptive languagedisorder F80.3 Acquiredaphasia
withepilepsy[Landau-Kleffnersyndrome] F80.8 Otherdevelopmentaldisordersof speechandlanguage
F80.9 Developmental disorderof speechandlanguage,unspecified F81 Specificdevelopmental
disordersof scholasticskills F81.0 Specificreadingdisorder F81.1Specificspellingdisorder F81.2](https://image.slidesharecdn.com/icd-161127112927/85/Icd-35-320.jpg)
![36
Specificdisorderof arithmetical skills F81.3 Mixeddisorderof scholasticskills F81.8 Other
developmental disordersof scholasticskills F81.9 Developmentaldisorderof scholasticskills,
unspecified F82Specificdevelopmental disorderof motorfunction F83 Mixedspecificdevelopmental
disorders
F84 Pervasive developmental disorders F84.0Childhoodautism F84.1 Atypical autism F84.2 Rett's
syndrome F84.3 Otherchildhooddisintegrative disorder F84.4Overactive disorderassociatedwith
mental retardationand stereotypedmovements F84.5 Asperger'ssyndrome F84.8Otherpervasive
developmental disorders F84.9Pervasive developmentaldisorder,unspecified F88Otherdisordersof
psychological development
F89 Unspecifieddisorderof psychological development
-40-
F90-F98 Behavioural andemotionaldisorderswithonsetusuallyoccurringinchildhoodandadolescence
F90 Hyperkineticdisorders F90.0 Disturbance of activityandattention F90.1 Hyperkineticconduct
disorder F90.8 Otherhyperkineticdisorders F90.9 Hyperkineticdisorder,unspecified F91 Conduct
disorders F91.0 Conductdisorderconfinedtothe familycontext F91.1 Unsocializedconductdisorder
F91.2 Socializedconductdisorder F91.3 Oppositionaldefiantdisorder F91.8 Otherconductdisorders
F91.9 Conductdisorder,unspecified F92Mixeddisordersof conductandemotions F92.0 Depressive
conduct disorder F92.8 Othermixeddisordersof conductandemotions F92.9Mixeddisorderof
conduct andemotions,unspecified F93 Emotional disorderswithonsetspecifictochildhood F93.0
Separationanxietydisorderof childhood F93.1Phobicanxietydisorderof childhood F93.2 Social
anxietydisorderof childhood F93.3Siblingrivalrydisorder F93.8 Otherchildhoodemotional disorders
F93.9 Childhoodemotionaldisorder,unspecified F94Disordersof social functioningwithonsetspecific
to childhoodandadolescence F94.0 Elective mutism F94.1 Reactive attachmentdisorderof childhood
F94.2 Disinhibitedattachmentdisorderof childhood F94.8 Otherchildhooddisordersof social
functioning F94.9 Childhooddisorderof social functioning,unspecified F95Tic disorders F95.0
Transientticdisorder F95.1 Chronicmotoror vocal ticdisorder F95.2 Combinedvocal andmultiple
motor ticdisorder[de laTourette's syndrome] F95.8 Othertic disorders F95.9 Tic disorder,
unspecified
-41-
F98 Otherbehavioural andemotional disorderswithonsetusually occurringinchildhoodand
adolescence F98.0Nonorganicenuresis F98.1Nonorganicencopresis F98.2Feedingdisorderof infancy
and childhood F98.3 Picaof infancyandchildhood F98.4 Stereotypedmovementdisorders F98.5
Stuttering[stammering] F98.6 Cluttering F98.8Otherspecifiedbehavioural andemotionaldisorders](https://image.slidesharecdn.com/icd-161127112927/85/Icd-36-320.jpg)
![37
withonset usuallyoccurringinchildhoodandadolescence F98.9Unspecifiedbehaviouralandemotional
disorderswithonsetusuallyoccurringinchildhoodandadolescence
F99 Unspecifiedmental disorder
F99 Mental disorder,nototherwise specified
-42-
Clinical descriptions
and
diagnosticguidelines
-43-
F00-F09 Organic,includingsymptomatic,mentaldisorders
Overviewof thisblock
F00 DementiainAlzheimer'sdisease F00.0DementiainAlzheimer'sdiseasewithearlyonset
F00.1DementiainAlzheimer'sdisease withlate onsetF00.2DementiainAlzheimer'sdisease,atypical or
mixed type F00.9DementiainAlzheimer'sdisease,unspecified
F01VasculardementiaF01.0Vasculardementiaof acute onsetF01.1Multi-infarctdementia
F01.2Subcortical vasculardementiaF01.3Mixedcortical andsubcortical vasculardementiaF01.8Other
vasculardementiaF01.9Vasculardementia, unspecified
F02Dementiainotherdiseasesclassifiedelsewhere F02.0DementiainPick'sdisease F02.1Dementiain
Creutzfeldt-Jakobdisease F02.2DementiainHuntington'sdisease F02.3DementiainParkinson'sdisease
F02.4Dementiainhumanimmunodeficiency virus[HIV] disease F02.8Dementiainotherspecified
diseasesclassified elsewhere
F03Unspecifieddementia
A fifthcharactermay be addedto specifydementiainF00-F03,as`follows: .x0Withoutadditional
symptoms .x1Othersymptoms,predominantlydelusional .x2Othersymptoms,predominantly
hallucinatory .x3Othersymptoms,predominantlydepressive .x4Othermixedsymptoms
F04Organic amnesicsyndrome,notinducedbyalcohol andother psychoactive substances](https://image.slidesharecdn.com/icd-161127112927/85/Icd-37-320.jpg)
![38
F05Delirium,notinducedbyalcohol andotherpsychoactive substancesF05.0Delirium, not
superimposedondementia,sodescribedF05.1Delirium, superimposedondementiaF05.8Other
deliriumF05.9Delirium, unspecified
F06Other mental disordersdue tobraindamage anddysfunction andtophysical disease F06.0Organic
hallucinosisF06.1OrganiccatatonicdisorderF06.2Organicdelusional [schizophrenia-like] disorder
-44-
F06.3Organic mood[affective]disorders.30Organicmanic disorder.31 Organicbipolardisorder.32
Organicdepressive disorder.33 Organicmixedaffective disorderF06.4Organicanxietydisorder
F06.5Organic dissociative disorderF06.6Organicemotionallylabile[asthenic] disorder F06.7Mild
cognitive disorderF06.8Otherspecifiedmentaldisordersdue tobraindamage anddysfunctionandto
physical disease F06.9Unspecifiedmentaldisorderdue tobraindamage and dysfunctionandto
physical disease
F07Personalityandbehavioural disordersdue tobraindisease,damage anddysfunctionF07.0Organic
personalitydisorderF07.1PostencephaliticsyndromeF07.2Postconcussional syndrome F07.8Other
organicpersonalityandbehavioural disorder due tobraindisease,damage anddysfunctionF07.9
Unspecifiedorganicpersonalityandbehavioural disordersdue tobraindisease, damage anddysfunction
F09Unspecifiedorganicorsymptomaticmental disorder
-45-
Introduction
Thisblockcomprises`arange of mental disordersgroupedtogetheronthe basisof theircommon,
demonstrable etiologyincerebral disease,braininjury,orotherinsultleadingtocerebral dysfunction.
The dysfunctionmaybe primary,as indiseases,injuries,andinsultsthataffectthe braindirectlyorwith
predilection;orsecondary,asinsystemicdiseasesanddisordersthatattackthe brainonlyas one of the
multiple organsorsystemsof the bodyinvolved.Alcohol-anddrug-causedbraindisorders,though
logicallybelongingtothisgroup,are classifiedunderF10-F19 because of practical advantagesinkeeping
all disordersdue topsychoactive substance use inasingle block.
Althoughthe spectrumof psychopathological manifestationsof the conditionsincludedhere isbroad,
the essential featuresof the disordersformtwomainclusters.Onthe one hand,there are syndromesin
whichthe invariable andmostprominentfeaturesare eitherdisturbancesof cognitive functions,suchas
memory,intellect,andlearning,ordisturbancesof the sensorium, suchasdisordersof consciousness
and attention.Onthe otherhand,there are syndromesof whichthe mostconspicuousmanifestations
are inthe areas of perception(hallucinations),thoughtcontents(delusions),ormoodand emotion](https://image.slidesharecdn.com/icd-161127112927/85/Icd-38-320.jpg)




![43
F00.2 DementiainAlzheimer'sdisease,atypical ormixedtype Dementiasthatdonot fitthe
descriptionsandguidelinesforeitherF00.0or F00.1 shouldbe classifiedhere;mixedAlzheimer'sand
vasculardementiasare alsoincludedhere.
F00.9 DementiainAlzheimer'sdisease,unspecified
-50-
F01 Vasculardementia
Vascular(formerlyarteriosclerotic) dementia,whichincludesmulti-infarctdementia,isdistinguished
fromdementiainAlzheimer'sdisease byitshistoryof onset,clinical features,andsubsequentcourse.
Typically,there isahistoryof transientischaemicattackswithbrief impairmentof consciousness,
fleetingpareses,orvisual loss.The dementiamayalsofollow asuccessionof acute cerebrovascular
accidentsor,lesscommonly,asingle majorstroke.Some impairmentof memoryandthinkingthen
becomesapparent.Onset,whichisusuallyinlaterlife,canbe abrupt,followingone particularischaemic
episode,orthere maybe more gradual emergence.The dementiaisusuallythe resultof infarctionof
the braindue tovascular diseases,includinghypertensive cerebrovasculardisease.The infarctsare
usuallysmall butcumulativeintheireffect.
Diagnosticguidelines
The diagnosispresupposesthe presence of adementiaasdescribedabove.Impairmentof cognitive
functioniscommonlyuneven,sothatthere maybe memoryloss,intellectualimpairment,andfocal
neurological signs.Insightandjudgementmaybe relativelywell preserved.Anabruptonsetora
stepwise deterioration,aswell asthe presence of focal neurological signsandsymptoms,increasesthe
probabilityof the diagnosis;insome cases,confirmationcanbe providedonlybycomputerizedaxial
tomographyor,ultimately,neuropathological examination.
Associatedfeaturesare:hypertension,carotidbruit,emotionallabilitywithtransientdepressive mood,
weepingorexplosive laughter,andtransientepisodesof cloudedconsciousnessordelirium,often
provokedbyfurtherinfarction.Personalityisbelievedtobe relativelywell preserved,but personality
changesmay be evidentinaproportionof caseswithapathy,disinhibition,oraccentuationof previous
traitssuch as egocentricity,paranoidattitudes,orirritability.
Includes:arterioscleroticdementia
Differential diagnosis.Consider: delirium(F05.-);otherdementia,particularlyinAlzheimer'sdisease
(F00.-);mood[affective] disorders(F30-F39);mildormoderate mental retardation(F70-F71);subdural
haemorrhage (traumatic(S06.5),nontraumatic(162.0)).](https://image.slidesharecdn.com/icd-161127112927/85/Icd-43-320.jpg)


![46
F02.2 DementiainHuntington'sdisease A dementiaoccurringaspartof a widespreaddegenerationof
the brain.Huntington'sdisease istransmittedbyasingle autosomal dominantgene.Symptomstypically
emerge inthe thirdand fourthdecade,andthe sex incidence isprobablyequal.Inaproportionof cases,
the earliestsymptomsmaybe depression,anxiety,orfrankparanoidillness,accompaniedbya
personalitychange.Progressionisslow,leadingto deathusuallywithin10to 15 years.
-53-
Diagnosticguidelines
The associationof choreiformmovementdisorder,dementia,andfamilyhistoryof Huntington'sdisease
ishighlysuggestiveof the diagnosis,thoughsporadiccasesundoubtedlyoccur.
Involuntarychoreiformmovements,typicallyof the face,hands,andshoulders,orinthe gait,are early
manifestations.Theyusuallyprecede the dementiaandonlyrarelyremainabsentuntilthe dementiais
veryadvanced.Othermotorphenomenamaypredominate whenthe onsetisatan unusuallyyoungage
(e.g.striatal rigidity)orat a late age (e.g.intentiontremor).
The dementiaischaracterizedbythe predominantinvolvementof frontal lobe functionsinthe early
stage,withrelative preservationof memoryuntillater.
Includes:dementiainHuntington'schorea
Differential diagnosis.Consider:othercasesof choreicmovements;Alzheimer's,Pick'sorCreutzfeldt-
Jakobdisease (F00.-,F02.0, F02.1).
F02.3 DementiainParkinson'sdisease A dementiadevelopinginthe course of establishedParkinson's
disease (especiallyitssevereforms).Noparticulardistinguishingclinicalfeatureshave yetbeen
demonstrated.The dementiamaybe differentfromthatineitherAlzheimer'sdiseaseorvascular
dementia;however,there isalsoevidence thatitmaybe the manifestationof aco-occurrence of one of
these conditionswithParkinson'sdisease.Thisjustifiesthe identificationof casesof Parkinson'sdisease
withdementiaforresearchuntil the issueisresolved.
Diagnosticguidelines
Dementiadevelopinginanindividualwithadvanced,usuallysevere,Parkinson'sdisease.
Includes:dementiainparalysisagitans dementiainparkinsonism Differential diagnosis.Consider:
othersecondarydementias(F02.8);multi-infarctdementia(F01.1) associatedwithhypertensiveor
diabeticvasculardisease;braintumor(C70-C72);normal pressure hydrocephalus(G91.2).
F02.4 Dementiainhumanimmunodeficiencyvirus[HIV] disease A disordercharacterizedbycognitive
deficitsmeetingthe clinical diagnosticcriteriafordementia,inthe absenceof aconcurrentillnessor
condition otherthanHIV infectionthatcouldexplainthe findings.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-46-320.jpg)
![47
HIV dementiatypicallypresentswithcomplaintsof forgetfulness,slowness,poorconcentration,and
difficultieswithproblem-solvingandreading.Apathy,reducedspontaneity,andsocial withdrawal are
common,and ina significantminorityof
-54-
affectedindividualsthe illnessmaypresentatypicallyasanaffective disorder,psychosis,orseizures.
Physical examinationoftenrevealstremor,impairedrapidrepetitive movements,imbalance,ataxia,
hypertonia,generalizedhyperreflexia,positivefrontal releasesigns,andimpairedpursuitandsaccadic
eye movements.
ChildrenalsodevelopanHIV-associatedneurodevelopmental disordercharacterizedbydevelopmental
delay,hypertonia,microcephaly,andbasal gangliacalcification.The neurological involvementmost
oftenoccursin the absence of opportunisticinfectionsandneoplasms,whichisnotthe case foradults.
HIV dementiagenerally,butnotinvariably,progressesquickly(overweeksormonths) tosevere global
dementia,mutism,anddeath.
Includes:AIDS-dementiacomplex HIV encephalopathyorsubacute encephalitis
F02.8 Dementiainotherspecifieddiseasesclassifiedelsewhere Dementiacanoccur as a manifestation
or consequence of avarietyof cerebral andsomaticconditions.Tospecifythe etiology,the ICD-10code
for the underlyingconditionshouldbe added.
Parkinsonism-dementiacomplex of Guamshouldalsobe codedhere (identifiedbyafifthcharacter,if
necessary).Itisa rapidlyprogressingdementiafollowedbyextrapyramidal dysfunctionand,insome
cases,amyotrophiclateral sclerosis.The disease wasoriginallydescribedonthe islandof Guamwhere it
occurs withhighfrequencyinthe indigenouspopulation,affectingtwice asmanymalesasfemales;itis
nowknownto occur alsoin PapuaNewGuineaandJapan.
Includes:dementiain: carbon monoxide poisoning(T58) cerebral lipidosis(E75.-) epilepsy(G40.-)
general paralysisof the insane (A52.1) hepatolenticulardegeneration(Wilson'sdisease) (E83.0)
hypercalcaemia(E83.5) hypothyroidism, acquired(E00.-,E02) intoxications(T36-T65) multiple
sclerosis(G35) neurosyphilis(A52.1) niacindeficiency[pellagra] (E52) polyarteritisnodosa(M30.0)
systemiclupuserythematosus(M32.-) trypanosomiasis(AfricanB56.-,AmericanB57.-) vitaminB12
deficiency(E53.8)
F03 Unspecifieddementia
-55-](https://image.slidesharecdn.com/icd-161127112927/85/Icd-47-320.jpg)


![50
Includes:acute brainsyndrome acute confusional state (nonalcoholic) acute infective psychosis
acute organic reaction acute psycho-organicsyndrome
Differential diagnosis.Deliriumshouldbe distinguishedfromotherorganicsyndromes,especially
dementia(F00-F03),fromacute and transientpsychoticdisorders(F23.-),andfromacute statesin
schizophrenia(F20.-) ormood[affective] disorders(F30-F39) inwhichconfusionalfeaturesmaybe
present.Delirium, inducedbyalcohol andotherpsychoactivesubstances,shouldbe codedinthe
appropriate section(F1x.4).
F05.0 Delirium,notsuperimposedondementia,sodescribedThiscode shouldbe usedfordelirium
that isnot superimposeduponpre-existingdementia.
F05.1 Delirium,superimposedondementiaThiscode shouldbe usedforconditionsmeetingthe above
criteriabutdevelopinginthe course of a dementia(F00-F03).
F05.8 Otherdelirium
Includes:deliriumof mixedorigin subacute confusional state ordelirium
F05.9 Delirium,unspecified
-58-
F06 Othermental disordersdue tobraindamage anddysfunctionandtophysical disease
Thiscategoryincludesmiscellaneousconditionscausallyrelatedtobraindysfunctiondue toprimary
cerebral disease,tosystemicdisease affectingthe brainsecondarily,toendocrine disorderssuchas
Cushing'ssyndrome orothersomaticillnesses,andtosome exogenoustoxicsubstances(butexcluding
alcohol anddrugs classifiedunderF10-F19) or hormones.These conditionshave incommonclinical
featuresthatdo notby themselvesallow apresumptivediagnosisof anorganicmental disorder,suchas
dementiaordelirium.Rather,the clinicalmanifestationsresemble,orare identical with,thoseof
disordersnotregardedas"organic"in the specificsense restrictedtothisblockof the classification.
Theirinclusionhere isbasedonthe hypothesisthattheyare directlycausedbycerebral diseaseor
dysfunctionratherthanresultingfromeitherafortuitousassociationwithsuchdiseaseordysfunction,
or a psychological reactiontoitssymptoms,suchasschizophrenia-likedisordersassociatedwithlong-
standingepilepsy.
The decisiontoclassifyaclinical syndrome here issupportedbythe following:
(a)evidence of cerebral disease,damage ordysfunctionorof systemicphysical disease,knowntobe
associatedwithone of the listedsyndromes;(b)atemporal relationship(weeksorafew months)
betweenthe developmentof the underlyingdiseaseandthe onsetof the mental syndrome;(c)recovery
fromthe mental disorderfollowingremoval orimprovementof the underlyingpresumedcause;](https://image.slidesharecdn.com/icd-161127112927/85/Icd-50-320.jpg)

![52
The general criteriaforassumingorganicetiology,laiddowninthe introductiontoF06, mustbe met.In
addition,there shouldbe one of the following:
(a)stupor(diminutionorcomplete absence of spontaneousmovementwithpartial orcomplete mutism,
negativism, andrigidposturing); (b)excitement(grosshypermotilitywithorwithoutatendencyto
assaultiveness);(c)both(shiftingrapidlyandunpredictablyfromhypo- tohyperactivity).
Othercatatonic phenomenathat increase confidence inthe diagnosisare:stereotypies,waxyflexibility,
and impulsive acts.
Excludes:catatonicschizophrenia(20.2) dissociativestupor(F44.2) stuporNOS (R40.1)
F06.2 Organicdelusional [schizophrenia-like] disorderA disorderinwhichpersistentorrecurrent
delusionsdominate the clinical picture.The delusionsmaybe accompaniedbyhallucinationsbutare not
confinedtotheircontent.Featuressuggestive of schizophrenia,suchasbizarre delusions,hallucinations,
or thoughtdisorder,mayalsobe present.
Diagnosticguidelines
-60-
The general criteriaforassuminganorganic etiology,laiddowninthe introductiontoF06, mustbe met.
In addition,there shouldbe delusions(persecutory,of bodilychange,jealousy, disease,ordeathof the
subjector anotherperson).Hallucinations,thoughtdisorder,orisolatedcatatonicphenomenamaybe
present.Consciousnessandmemorymustnotbe affected.Thisdiagnosisshouldnotbe made if the
presumedevidenceof organiccausationisnonspecificorlimitedtofindingssuchasenlargedcerebral
ventricles(visualizedoncomputerizedaxial tomography) or"soft"neurological signs.
Includes:paranoidandparanoid-hallucinatoryorganicstates schizophrenia-likepsychosisinepilepsy
Excludes:acute andtransientpsychoticdisorders(F23.-) drug-inducedpsychoticdisorders(F1x.5)
persistentdelusionaldisorder(F22.-) schizophrenia(F20.-)
F06.3 Organicmood [affective] disordersDisorderscharacterizedbyachange inmood or affect,
usuallyaccompaniedbyachange in the overall level of activity.The onlycriterionforinclusionof these
disordersinthisblockistheirpresumeddirectcausationbyacerebral orother physical disorderwhose
presence musteitherbe demonstratedindependently(e.g.bymeansof appropriate physical and
laboratoryinvestigations) orassumedonthe basisof adequate historyinformation.The affective
disordermustfollowthe presumedorganicfactorandbe judgednotto representanemotional
response tothe patient'sknowledge of having,orhavingthe symptomsof,aconcurrentbrain disorder.
Postinfective depression(e.g.followinginfluenza)isacommonexample andshouldbe codedhere.
Persistentmildeuphorianotamountingtohypomania(whichissometimesseen,forinstance,in
associationwithsteroidtherapyorantidepressants) shouldnotbe codedhere butunderF06.8.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-52-320.jpg)
![53
Diagnosticguidelines
In additiontothe general criteriaforassumingorganicetiology,laiddowninthe introductiontoF06,the
conditionmustmeetthe requirementsforadiagnosisof one of the disorderslistedunderF30-F33.
Excludes:mood[affective] disorders,nonorganicor unspecified(F30- F39) righthemispheric
affective disorder(F07.8)
The followingfive-charactercodesmightbe usedtospecifythe clinical disorder:
F06.30 OrganicmanicdisorderF06.31 Organicbipolaraffective disorderF06.32 Organic depressive
disorderF06.33 Organicmixedaffective disorder
-61-
F06.4 OrganicanxietydisorderA disordercharacterizedbythe essential descriptive featuresof a
generalizedanxietydisorder(41.1),apanic disorder(F41.0),ora combinationof both,butarisingasa
consequence of anorganicdisordercapable of causingcerebral dysfunction(e.g.temporal lobe
epilepsy,thyrotoxicosis,orphaechromocytoma).
Excludes:anxietydisorders,nonorganicorunspecified(F41.-)
F06.5 Organicdissociative disorderA disorderthatmeetsthe requirementsforone of the disordersin
F44.- (dissociative [conversion] disorder) andforwhichthe general criteriafororganicetiologyare also
fulfilled(asdescribedinthe introductiontothisblock).
Excludes:dissociative[conversion] disorders,nonorganicor unspecified(F44.-)
F06.6 Organicemotionallylabile [asthenic] disorderA disordercharacterizedbymarkedandpersistent
emotional incontinence orlability,fatiguability,ora varietyof unpleasantphysicalsensations(e.g.
dizziness)andpainsregardedasbeingdue tothe presence of anorganic disorder.Thisdisorderis
thoughtto occur in associationwithcerebrovasculardiseaseorhypertensionmore oftenthanwith
othercauses.
Excludes:somatoformdisorders,nonorganicorunspecified (F45.-)
F06.7 Mildcognitive disorderThisdisordermayprecede,accompany,orfollow awide varietyof
infectionsandphysical disorders,bothcerebral andsystemic(includingHIV infection).Direct
neurological evidence of cerebral involvementisnotnecessarilypresent,butthere mayneverthelessbe
distressandinterference withusual activities.The boundariesof thiscategoryare still tobe firmly
established.Whenassociatedwithaphysical disorderfromwhichthe patientrecovers,mildcognitive
disorderdoesnotlastfor more thana few additional weeks.Thisdiagnosisshouldnotbe made if the
conditionisclearlyattributable toamental or behavioural disorderclassifiedinanyof the remaining
blocksinthisbook.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-53-320.jpg)



![57
-65-
F10-F19 Mental and behavioural disordersdue topsychoactivesubstance use
Overviewof thisblock
F10.-Mental and behavioural disordersdue touse of alcohol F11.-Mental andbehavioural disordersdue
to use of opioidsF12.-Mental andbehavioural disordersdue touse of cannabinoidsF13.-Mental and
behavioural disordersdue touse of sedativesorhypnoticsF14.-Mental andbehavioural disordersdue to
use of cocaine F15.-Mental andbehavioural disordersdue touse of otherstimulants,includingcaffeine
F16.-Mental and behavioural disordersdue touse of hallucinogensF17.-Mental and behavioural
disordersdue touse of tobacco F18.-Mental and behavioural disordersdue touse of volatile solvents
F19.-Mental and behavioural disordersdue tomultipledruguse anduse of otherpsychoactive
substances
Four- and five-charactercodesmaybe usedtospecifythe clinical conditions,asfollows:
F1x.0 Acute intoxication .00 Uncomplicated.01With trauma or otherbodilyinjury.02Withother
medical complications.03Withdelirium.04With perceptual distortions.05Withcoma .06 With
convulsions.07Pathological intoxication
F1x.1 Harmful use
F1x.2 Dependence syndrome .20 Currentlyabstinent.21Currentlyabstinent,butinaprotected
environment.22Currentlyona clinicallysupervisedmaintenanceor replacementregime [controlled
dependence] .23 Currentlyabstinent,butreceivingtreatmentwith aversive orblockingdrugs .24
Currentlyusingthe substance [active dependence].25Continuoususe .26 Episodicuse [dipsomania]
F1x.3 Withdrawal state .30 Uncomplicated.31 Withconvulsions
-66-
F1x.4 Withdrawal state withdelirium .40Withoutconvulsions.41Withconvulsions
F1x.5 Psychoticdisorder .50 Schizophrenia-like .51Predominantlydelusional.52Predominantly
hallucinatory.53Predominantlypolymorphic.54 Predominantlydepressive symptoms.55
Predominantlymanicsymptoms.56Mixed
F1x.6 Amnesicsyndrome
F1x.7 Residual andlate-onsetpsychoticdisorder.70 Flashbacks.71 Personalityorbehaviourdisorder.72
Residual affective disorder.73 Dementia.74Otherpersistingcognitive impairment.75Late-onset
psychoticdisorder](https://image.slidesharecdn.com/icd-161127112927/85/Icd-57-320.jpg)



![61
continue takingdrugs. The dependence syndrome maybe presentfora specificsubstance (e.g.
tobacco or diazepam),foraclass of substances(e.g.opioiddrugs),orfora wider
-71-
range of differentsubstances(asforthose individualswhofeel asense of compulsionregularlytouse
whateverdrugsare available andwhoshow distress,agitation,and/orphysical signsof awithdrawal
state uponabstinence).
Includes:chronicalcoholism dipsomania drugaddiction The diagnosisof the dependence syndrome
may be furtherspecifiedbythe followingfive-charactercodes:
F1x.20 Currentlyabstinent F1x.21 Currentlyabstinent,butinaprotectedenvironment(e.g.inhospital,
ina therapeuticcommunity,inprison,etc.) F1x.22 Currentlyona clinicallysupervisedmaintenance
or replacementregime[controlleddependence] (e.g.withmethadone;nicotinegumornicotine patch)
F1x.23 Currentlyabstinent,butreceivingtreatmentwithaversiveorblockingdrugs (e.g.naltrexone or
disulfiram) F1x.24 Currentlyusingthe substance [active dependence] F1x.25 Continuoususe
F1x.26 Episodicuse [dipsomania] F1.3 Withdrawal state A groupof symptomsof variable clustering
and severityoccurringonabsolute orrelative withdrawal of asubstance afterrepeated,andusually
prolongedand/orhigh-dose,use of thatsubstance.Onsetandcourse of the withdrawal state are time-
limitedandare relatedtothe type of substance andthe dose beingusedimmediatelybefore
abstinence.The withdrawal state maybe complicatedbyconvulsions. Diagnosticguidelines
Withdrawal state isone of the indicatorsof dependence syndrome (see F1x.2) andthislatterdiagnosis
shouldalsobe considered. Withdrawal state shouldbe codedasthe maindiagnosisif itisthe reason
for referral andsufficientlysevere to require medical attentioninitsownright. Physical symptoms
vary accordingto the substance beingused.Psychological disturbances(e.g.anxiety,depression,and
sleepdisorders) are also
-72-
commonfeaturesof withdrawal.Typically,the patientislikelytoreportthatwithdrawal symptomsare
relievedbyfurthersubstance use.
It shouldbe rememberedthatwithdrawalsymptomscanbe inducedbyconditioned/learnedstimuliin
the absence of immediatelyprecedingsubstance use.Insuchcasesa diagnosisof withdrawalstate
shouldbe made onlyif itis warrantedintermsof severity. Differential diagnosis.Manysymptoms
presentindrugwithdrawal state mayalsobe causedby otherpsychiatricconditions,e.g.anxietystates
and depressive disorders.Simple "hangover"ortremordue to otherconditionsshouldnotbe confused
withthe symptomsof a withdrawal state. The diagnosisof withdrawal state maybe furtherspecified
by usingthe followingfive-charactercodes: F1x.30 Uncomplicated](https://image.slidesharecdn.com/icd-161127112927/85/Icd-61-320.jpg)

![63
cocaine psychoses).Falsediagnosisinsuchcasesmayhave distressingandcostlyimplicationsforthe
patientandfor the healthservices. Includes:alcoholichallucinosis alcoholicjealousy alcoholic
paranoia alcoholicpsychosisNOS Differential diagnosis.Considerthe possibilityof anothermental
disorderbeingaggravatedorprecipitatedbypsychoactive substance use (e.g.schizophrenia(F20.-);
mood[affective] disorder(F30-F39);paranoidorschizoidpersonalitydisorder(F60.0,F60.1)).In such
cases,a diagnosisof psychoactive substance-inducedpsychoticstate maybe inappropriate.
-74-
The diagnosisof psychoticstate maybe furtherspecifiedbythe followingfive-charactercodes:
F1x.50 Schizophrenia-like F1x.51 Predominantlydelusional F1x.52 Predominantlyhallucinatory
(includesalcoholichallucinosis) F1x.53 Predominantlypolymorphic F1x.54 Predominantly
depressivesymptoms F1x.55 Predominantlymanicsymptoms F1x.56 Mixed F1x.6 Amnesic
syndrome A syndrome associatedwithchronicprominentimpairmentof recentmemory;remote
memoryissometimesimpaired,while immediaterecall ispreserved.Disturbancesof time sense and
orderingof eventsare usuallyevident,asare difficultiesinlearningnew material.Confabulationmaybe
markedbut isnot invariablypresent.Othercognitivefunctionsare usuallyrelativelywell preservedand
amnesicdefects are outof proportiontoother disturbances. Diagnosticguidelines Amnesic
syndrome inducedbyalcohol orotherpsychoactive substancescodedhere shouldmeetthe general
criteriafororganic amnesicsyndrome (seeF04).The primaryrequirementsfor thisdiagnosisare:
(a)memoryimpairmentasshowninimpairmentof recentmemory(learningof new material);
disturbancesof time sense (rearrangementsof chronological sequence,telescopingof repeatedevents
intoone,etc.); (b)absence of defectin immediate recall,of impairmentof consciousness,andof
generalizedcognitive impairment; (c)historyorobjectiveevidence of chronic(andparticularlyhigh-
dose) use of alcohol ordrugs. Personalitychanges,oftenwithapparentapathyandlossof initiative,
and a tendencytowardsself-neglectmayalsobe present,butshouldnotbe regardedasnecessary
conditionsfordiagnosis. Althoughconfabulationmaybe markeditshouldnotbe regardedas a
necessaryprerequisite fordiagnosis.
-75-
Includes:Korsakov'spsychosisorsyndrome,alcohol- or otherpsychoactive substance-induced
Differential diagnosis.Consider:organicamnesicsyndrome (nonalcoholic) (see F04);otherorganic
syndromesinvolvingmarkedimpairmentof memory(e.g.dementiaordelirium) (F00-F03;F05.-);a
depressivedisorder(F31-F33). F1x.7Residual andlate-onsetpsychoticdisorder A disorderinwhich
alcohol- orpsychoactive substance-inducedchangesof cognition,affect,personality,orbehaviour
persistbeyondthe periodduringwhichadirectpsychoactive substance-relatedeffectmightreasonably
be assumedto be operating. Diagnosticguidelines Onsetof the disordershouldbe directlyrelatedto
the use of alcohol ora psychoactive substance.Casesinwhichinitial onsetoccurslaterthanepisode(s)
of substance use shouldbe codedhere onlywhereclearandstrongevidence isavailabletoattribute the](https://image.slidesharecdn.com/icd-161127112927/85/Icd-63-320.jpg)
![64
state to the residual effectof the substance.The disordershouldrepresentachange fromor marked
exaggerationof priorandnormal state of functioning. The disordershouldpersistbeyondanyperiod
of time duringwhichdirecteffectsof the psychoactive substance mightbe assumedtobe operative(see
F1x.0, acute intoxication).Alcohol-orpsychoactive substance-induceddementiaisnotalways
irreversible;afteranextendedperiodof total abstinence,intellectualfunctionsandmemorymay
improve. The disordershouldbe carefullydistinguishedfromwithdrawal-relatedconditions(see F1x.3
and F1x.4).It shouldbe rememberedthat,undercertainconditionsandforcertainsubstances,
withdrawal state phenomenamaybe presentforaperiodof manydays or weeksafterdiscontinuation
of the substance. Conditionsinducedbyapsychoactive substance,persistingafteritsuse,andmeeting
the criteriafor diagnosisof psychoticdisordershouldnotbe diagnosedhere (use F1x.5,psychotic
disorder).Patientswhoshowthe chronicend-stateof Korsakov'ssyndrome shouldbe codedunder
F1x.6.
Differential diagnosis.Consider:pre-existingmental disordermaskedbysubstance use andre-emerging
as psychoactive substance-relatedeffectsfade (forexample,phobicanxiety,adepressivedisorder,
schizophrenia,orschizotypal disorder).Inthe case of flashbacks, consideracute andtransientpsychotic
disorders(F23.-).Consideralsoorganicinjuryandmildormoderate mental retardation(F70-F71),which
may coexistwithpsychoactive substancemisuse. Thisdiagnosticrubricmaybe furthersubdividedby
usingthe followingfive-charactercodes:
-76-
F1x.70 Flashbacks May be distinguishedfrompsychoticdisorderspartlybytheirepisodicnature,
frequentlyof veryshortduration(secondsorminutes) andbytheirduplication(sometimesexact) of
previous drug-relatedexperiences. F1x.71 Personalityorbehaviourdisorder Meetingthe criteriafor
organicpersonalitydisorder(F07.0). F1x.72 Residual affectivedisorder Meetingthe criteriafor
organicmood [affective] disorders(F06.3). F1x.73 Dementia Meetingthe general criteriafor
dementiaasoutlinedinthe introductiontoF00-F09. F1x.74 Otherpersistingcognitive impairment A
residual categoryfordisorderswithpersistingcognitive impairment,whichdonotmeetthe criteriafor
psychoactive substance-inducedamnesicsyndrome(F1x.6) ordementia(F1x.73).
F1x.75 Late-onsetpsychoticdisorder F1x.8Othermental andbehavioural disorders Code here any
otherdisorderinwhichthe use of a substance canbe identifiedascontributingdirectlytothe condition,
but whichdoesnotmeetthe criteriaforinclusioninanyof the above disorders. F1x.9Unspecified
mental andbehavioural disorder F20-F29 Schizophrenia,schizotypalanddelusionaldisorders
Overviewof thisblock F20 Schizophrenia F20.0 Paranoidschizophrenia F20.1 Hebephrenic
schizophrenia F20.2 Catatonicschizophrenia F20.3 Undifferentiatedschizophrenia F20.4 Post-
schizophrenicdepression F20.5 Residual schizophrenia F20.6 Simple schizophrenia F20.8 Other
schizophrenia F20.9 Schizophrenia,unspecified A fifthcharactermay be usedto classifycourse:
F20.x0 Continuous F20.x1 Episodicwithprogressive deficit F20.x2 Episodicwithstable deficit](https://image.slidesharecdn.com/icd-161127112927/85/Icd-64-320.jpg)










![75
F32.-). Includes:bouffée délirante withoutsymptomsof schizophreniaorunspecified cycloid
psychosiswithoutsymptomsof schizophreniaorunspecified
-88-
F23.1 Acute polymorphicpsychoticdisorderwithsymptomsof schizophrenia Anacute psychotic
disorderwhichmeetsthe descriptivecriteriaforacute polymorphicpsychoticdisorder(F23.0) butin
whichtypicallyschizophrenicsymptomsare alsoconsistentlypresent. Diagnosticguidelines
For a definite diagnosis,criteria(a),(b),and(c) specifiedforacute polymorphicpsychoticdisorder
(F23.0) mustbe fulfilled;inaddition,symptomsthatfulfilthe criteriaforschizophrenia(F20.-) musthave
beenpresentforthe majorityof the time since the establishmentof anobviouslypsychoticclinical
picture. If the schizophrenicsymptomspersistformore than1 month,the diagnosisshouldbe
changedto schizophrenia(F20.-). Includes:bouffée délirante withsymptomsof schizophrenia
cycloidpsychosiswithsymptomsof schizophrenia F23.2 Acute schizophrenia-like psychoticdisorder
An acute psychoticdisorderinwhichthe psychoticsymptomsare comparativelystable andfulfil the
criteriaforschizophrenia(F20.-) buthave lastedforlessthan1 month. Some degree of emotional
variabilityorinstabilitymaybe present,butnotto the extentdescribedinacute polymorphicpsychotic
disorder(F23.0). Diagnosticguidelines
For a definite diagnosis: (a)the onsetof psychoticsymptomsmustbe acute (2 weeksorlessfroma
nonpsychotictoa clearlypsychoticstate); (b)symptomsthatfulfil the criteriaforschizophrenia(F20.-)
musthave beenpresentforthe majorityof the time since the establishmentof anobviouslypsychotic
clinical picture; (c)the criteriaforacute polymorphicpsychoticdisorderare notfulfilled. If the
schizophrenicsymptomslastformore than1 month,the diagnosisshouldbe changedtoschizophrenia
(F20.-). Includes: acute (undifferentiated)schizophrenia brief schizophreniformdisorder brief
schizophreniformpsychosis oneirophrenia schizophrenicreaction Excludes:organicdelusional
[schizophrenia-like] disorder(F06.2) schizophreniformdisorderNOS(F20.8) F23.3 Otheracute
predominantlydelusional psychoticdisorders Acute psychoticdisordersinwhichcomparativelystable
delusionsorhallucinationsare the mainclinical features,butdonotfulfil the criteriaforschizophrenia
(F20.-). Delusionsof persecutionorreference are common,andhallucinationsare usuallyauditory
(voicestalkingdirectlytothe patient). Diagnosticguidelines
For a definite diagnosis:
-89-
(a)the onsetof psychoticsymptomsmustbe acute (2weeksorlessfroma nonpsychotictoa clearly
psychoticstate); (b)delusionsorhallucinationsmusthave beenpresentforthe majorityof the time
since the establishmentof anobviouslypsychoticstate;and (c)the criteriaforneitherschizophrenia
(F20.-) nor acute polymorphicpsychoticdisorder(F23.0) are fulfilled. If delusionspersistformore than](https://image.slidesharecdn.com/icd-161127112927/85/Icd-75-320.jpg)
![76
3 months,the diagnosisshouldbe changedtopersistentdelusional disorder(F22.-). If only
hallucinationspersistformore than3 months,the diagnosisshouldbe changedtoothernonorganic
psychoticdisorder(F28). Includes:paranoidreaction psychogenicparanoidpsychosis F23.8 Other
acute and transientpsychoticdisorders Anyotheracute psychoticdisordersthatare unclassifiable
underany othercategoryin F23 (suchas acute psychoticstatesinwhichdefinite delusionsor
hallucinationsoccurbutpersistforonlysmall proportionsof the time) shouldbe codedhere. Statesof
undifferentiatedexcitementshouldalsobe codedhere if more detailedinformation aboutthe patient's
mental state isnot available,providedthatthere isnoevidence of anorganiccause. F23.9 Acute and
transientpsychoticdisorder,unspecified
Includes:(brief) reactivepsychosisNOS
F24 Induceddelusionaldisorder
A delusional disordersharedbytwoormore people withclose emotional links. Onlyone of the people
suffersfroma genuine psychoticdisorder;the delusionsare inducedinthe other(s) andusually
disappearwhenthe peopleare separated.
Includes:folie àdeux inducedparanoidorpsychoticdisorder
F25 Schizoaffective disorders
These are episodicdisordersinwhichbothaffectiveandschizophrenicsymptomsare prominentwithin
the same episode of illness,preferablysimultaneously,butatleast withinafew daysof each other.
Theirrelationshiptotypical mood[affective] disorders(F30-F39) andto schizophrenicdisorders(F20-
F24) is uncertain. Theyare givena separate categorybecause theyare toocommonto be ignored.
Otherconditionsin whichaffective symptomsare superimposeduponorformpart of a pre-existing
schizophrenicillness,orinwhichtheycoexistoralternate withothertypesof persistentdelusional
disorders,are classifiedunderthe appropriate categoryinF20-F29. Mood-incongruentdelusionsor
hallucinationsinaffective disorders(F30.2,F31.2, F31.5, F32.3, or F33.3) donot by themselvesjustifya
diagnosisof schizoaffective disorder. Patientswhosufferfromrecurrentschizoaffective episodes,
particularlythose whose symptomsare of the manicrather thanthe depressive type,usuallymake afull
recoveryandonlyrarelydevelopadefectstate. Diagnosticguidelines
-90-
A diagnosisof schizoaffective disordershouldbe made onlywhenbothdefinite schizophrenicand
definiteaffectivesymptomsare prominentsimultaneously,or withinafew daysof each other,within
the same episode of illness,andwhen,asaconsequence of this,the episode of illnessdoesnotmeet
criteriaforeitherschizophreniaor a depressive ormanicepisode. The termshouldnotbe appliedto
patientswhoexhibitschizophrenicsymptomsandaffectivesymptomsonlyindifferentepisodesof
illness. Itiscommon,for example,foraschizophrenicpatienttopresentwithdepressive symptomsin
the aftermathof a psychoticepisode(seepost-schizophrenicdepression(F20.4)). Some patientshave](https://image.slidesharecdn.com/icd-161127112927/85/Icd-76-320.jpg)

![78
the prognosisislessfavourable. Althoughthe majorityof patientsrecovercompletely,someeventually
developaschizophrenicdefect. Diagnosticguidelines
There mustbe prominentdepression,accompaniedbyatleasttwocharacteristicdepressive symptoms
or associatedbehavioural abnormalitiesaslistedfordepressiveepisode (F32.-);withinthe same
episode,atleastone andpreferablytwotypicallyschizophrenicsymptoms(asspecifiedfor
schizophrenia(F20.-),diagnosticguidelines(a)-(d)) shouldbe clearlypresent. Thiscategory shouldbe
usedbothfor a single schizoaffectiveepisode,depressive type,andfora recurrentdisorderinwhichthe
majorityof episodesare schizoaffective,depressive type. Includes: schizoaffective psychosis,
depressivetype schizophreniformpsychosis,depressivetype F25.2 Schizoaffective disorder,mixed
type Disordersinwhichsymptomsof schizophrenia(F20.-) coexistwiththose of amixedbipolar
affective disorder(F31.6) shouldbe codedhere. Includes: cyclicschizophrenia mixed
schizophrenicandaffective psychosis F25.8 Otherschizoaffectivedisorders F25.9 Schizoaffective
disorder,unspecified
Includes: schizoaffective psychosisNOS
F28 Othernonorganicpsychoticdisorders
Psychoticdisordersthatdonot meetthe criteriaforschizophrenia(F20.-) orforpsychotictypesof mood
[affective] disorders(F30-F39),andpsychoticdisordersthatdonot meetthe symptomaticcriteriafor
persistentdelusionaldisorder(F22.-) shouldbe codedhere. Includes: chronic hallucinatorypsychosis
NOS
F29 Unspecifiednonorganicpsychosis
Thiscategoryshouldalsobe usedfor psychosisof unknownetiology.
Includes: psychosisNOS Excludes: mental disorderNOS (F99) organicor symptomaticpsychosis
NOS(F09) F30-F39 Mood [affective]disorders
Overviewof thisblock
F30 Manic Episode F30.0 Hypomania
-92-
F30.1 Mania withoutpsychoticsymptomsF30.2Mania withpsychoticsymptomsF30.8 Othermanic
episodesF30.9Manic episode,unspecified F31Bipolaraffective disorderF31.0Bipolaraffective
disorder,currentepisodehypomanicF31.1Bipolaraffective disorder,currentepisodemanicwithout
psychoticsymptomsF31.2Bipolaraffectivedisorder,currentepisode manicwithpsychoticsymptoms
F31.3Bipolaraffctive disorder,currentepisodemildormoderate depression .30Withoutsomatic
syndrome .31 Withsomaticsyndrome F31.4Bipolaraffective disorder,currentepisode severe
depressionwithoutpsychoticsymptomsF31.5Bipolaraffective disorder,currentepisodesevere](https://image.slidesharecdn.com/icd-161127112927/85/Icd-78-320.jpg)
![79
depressionwithpsychoticsymptomsF31.6Bipolaraffective disorder,currentepisode mixed
F31.7Bipolaraffective disorder,currentlyinremissionF31.8Otherbipolaraffectivedisorders
F31.9Bipolaraffective disorder,unspecified F32Depressive episode F32.0Milddepressiveepisode .00
Withoutsomaticsyndrome .01 With somaticsyndrome F32.1 Moderate depressiveepisode .10
Withoutsomaticsyndrome .11 With somaticsyndrome F32.2 Severe depressive episodewithout
psychoticsymptomsF32.3 Severe depressive episode withpsychoticsymptomsF32.8Otherdepressive
episodesF32.9Depressive episode,unspecified
-93-
F33 Recurrentdepressive disorderF33.0Recurrentdepressive disorder,currentepisodemild .00
Withoutsomaticsyndrome .01 With somaticsyndrome F33.1 Recurrentdepressive disorder,current
episode moderate .10 Withoutsomaticsyndrome .11 Withsomaticsyndrome F33.2Recurrent
depressivedisorder,currentepisode severewithoutpsychoticsymptomsF33.3Recurrentdepressive
disorder,currentepisodesevere withpsychoticsymptomsF33.4Recurrentdepressivedisorder,
currentlyinremissionF33.8Otherrecurrentdepressive disordersF33.9Recurrentdepressivedisorder,
unspecified F34Persistentmood[affective]disordersF34.0CyclothymiaF34.1 DysthymiaF34.8 Other
persistentmood[affective]disordersF34.9Persistentmood[affective] disorder,unspecified F38Other
mood[affective] disordersF38.0Othersingle mood[affective] disorders .00Mixedaffective episode
F38.1 Otherrecurrentmood[affective] disorders .10Recurrentbrief depressivedisorderF38.8 Other
specifiedmood[affective] disorders F39 Unspecifiedmood[affective] disorder
-94-
Introduction
The relationshipbetweenetiology,symptoms,underlyingbiochemical processes,response to
treatment,andoutcome of mood[affective] disordersisnotyetsufficientlywell understoodtoallow
theirclassificationinaway thatis likelytomeetwithuniversalapproval. Nevertheless,aclassification
mustbe attempted,andthatpresentedhere isputforwardinthe hope thatit will atleastbe
acceptable,since itisthe resultof widespreadconsultation.
In these disorders,the fundamental disturbance isachange inmoodor affect,usuallytodepression
(withorwithoutassociatedanxiety) ortoelation. Thismoodchange isnormallyaccompaniedbya
change in the overall level of activity,andmostothersymptomsare eithersecondaryto,oreasily
understoodinthe contextof,suchchanges. Most of these disorderstendtobe recurrent,andthe onset
of individual episodesisoftenrelatedtostressful eventsorsituations. Thisblockdealswithmood
disordersinall age groups;those arisinginchildhoodandadolescence shouldtherefore be codedhere.
The main criteriabywhichthe affective disordershave beenclassifiedhave beenchosenforpractical
reasons,inthat theyallowcommonclinical disorderstobe easilyidentified. Single episodeshave been](https://image.slidesharecdn.com/icd-161127112927/85/Icd-79-320.jpg)






![86
gradesof severity,adurationof atleast2 weeksisusuallyrequiredfordiagnosis,butshorterperiods
may be reasonable if symptomsare unusuallysevere andof rapidonset.
Some of the above symptomsmaybe markedanddevelopcharacteristicfeaturesthatare widely
regardedas havingspecial clinical significance. The mosttypical examplesof these "somatic"symptoms
(see introductiontothisblock,page 112 [of Blue Book]) are:lossof interestorpleasure inactivitiesthat
are normallyenjoyable;lackof emotional reactivitytonormallypleasurablesurroundingsandevents;
wakinginthe morning2 hours or more before the usual time;depressionworseinthe morning;
objective evidence of definite psychomotorretardationoragitation(remarkedonorreportedbyother
people);markedlossof appetite;weightloss(oftendefinedas5% or more of bodyweightinthe past
month);markedlossof libido. Usually,thissomaticsyndrome isnotregardedaspresentunlessabout
fourof these symptomsare definitelypresent.
The categoriesof mild(F32.0),moderate (F32.1) and severe (F32.2and F32.3) depressive episodes
describedinmore detail belowshouldbe usedonlyforasingle (first) depressive episode. Further
depressiveepisodesshouldbe classifiedunder one of the subdivisionsof recurrentdepressive disorder
(F33.-).
These gradesof severityare specifiedtocoverawide range of clinical statesthatare encounteredin
differenttypesof psychiatricpractice. Individualswithmilddepressiveepisodesare commoninprimary
care and general medical settings,whereaspsychiatricinpatientunitsdeal largelywithpatientssuffering
fromthe severe grades.
-101-
Acts of self-harmassociatedwithmood[affective] disorders,mostcommonlyself-poisoningby
prescribedmedication,shouldbe recordedbymeansof anadditional code fromChapterXXof ICD-10
(X60-X84). These codesdonot involve differentiationbetweenattemptedsuicideand"parasuicide",
since bothare includedinthe general category of self-harm.
Differentiationbetweenmild,moderate,andsevere depressive episodesrestsuponacomplicated
clinical judgementthatinvolvesthe number,type,andseverityof symptomspresent. The extentof
ordinarysocial andwork activitiesisoftenauseful general guide tothe likelydegreeof severityof the
episode,butindividual,social,andcultural influencesthatdisruptasmoothrelationshipbetween
severityof symptomsandsocial performanceare sufficientlycommonandpowerful tomake itunwise
to include social performance amongstthe essentialcriteriaof severity.
The presence of dementia(F00-F03) ormental retardation(F70-F79) doesnotrule out the diagnosisof a
treatable depressiveepisode,butcommunicationdifficultiesare likelytomake itnecessarytorelymore
than usual forthe diagnosisuponobjectivelyobservedsomaticsymptoms,suchaspsychomotor
retardation,lossof appetite andweight,andsleepdisturbance.
Includes:](https://image.slidesharecdn.com/icd-161127112927/85/Icd-86-320.jpg)



![90
Recurrentdepressive episode maybe subdivided,asbelow,byspecifyingfirstthe type of the current
episode andthen(if sufficientinformationisavailable)the type thatpredominatesin all the episodes.
Includes:recurrentepisodesof depressivereaction,psychogenicdepression, reactive depression,
seasonal affective disorder(F33.0or F33.2) recurrentepisodesof endogenousdepression,major
depression,manic depressive psychosis(depressedtype),psychogenicorreactive depressive
psychosis,psychoticdepression,vital depression(F33.2 or F33.3)
Excludes:recurrentbrief depressiveepisodes(F38.1)
F33.0 Recurrentdepressive disorder,currentepisodemild
D i a g n o s ti c g u i d e li n e s
For a definite diagnosis:
(a)the criteriaforrecurrentdepressive disorder(F33.-) shouldbe fulfilled,andthe currentepisode
shouldfulfilthe criteriafordepressiveepisode,mildseverity(F32.0);and(b)atleasttwoepisodes
shouldhave lastedaminimumof 2 weeksandshouldhave beenseparatedbyseveral monthswithout
significantmooddisturbance. Otherwise,the diagnosisshouldbe otherrecurrentmood[affective]
disorder(F38.1).
A fifthcharactermay be usedto specifythe presence of the somaticsyndromeinthe currentepisode:
F33.00 Withoutsomaticsyndrome (See F32.00)
-105-
F33.01 With somaticsyndrome (See F32.01)
If required,the predominanttype of previousepisodes(mildormoderate,severe,uncertain)maybe
specified.
F33.2Recurrentdepressive disorder,currentepisode moderate
D i a g n o s ti c g u i d e li n e s
For a definite diagnosis:
(a)the criteriaforrecurrentdepressive disorder(F33.-) shouldbe fulfilled,andthe currentepisode
shouldfulfilthe criteriafordepressiveepisode,moderateseverity(F32.1);and(b)atleasttwoepisodes
shouldhave lastedaminimumof 2 weeksandshouldhave beenseparatedbyseveral monthswithout
significantmooddisturbance.
Otherwise the diagnosisshouldbe otherrecurrentmood[affective] disorder(F38.1).](https://image.slidesharecdn.com/icd-161127112927/85/Icd-90-320.jpg)
![91
A fifthcharactermay be usedto specifythe presence of the somaticsyndromeinthe currentepisode:
F33.10 Withoutsomaticsyndrome (see F32.10)
F33.11 Withsomaticsyndrome (see F32.11)
If required,the predominanttype of previousepisodes(mild,moderate,severe,uncertain) maybe
specified.
F33.3Recurrentdepressive disorder,currentepisode severe withpsychoticsymptoms
D i a g n o s ti c g u i d e li n e s
For a definite diagnosis:
(a)the criteriaforrecurrentdepressive disorder(F33.-) shouldbe fulfilled,andthe currentepisode
shouldfulfilthe criteriaforsevere depressive episode withpsychoticsymptoms(F32.3);and(b)atleast
twoepisodesshouldhave lastedaminimumof 2weeksandshouldhave beenseparatedbyseveral
monthswithoutsignificantmooddisturbance.
Otherwise the diagnosisshouldbe otherrecurrentmood[affective] disorder(F38.1).
If required,delusionsorhallucinationsmaybe specifiedasmood-congruentormood- incongruent(see
F30.2).
-106-
If required,the predominanttype of previousepisodes(mild,moderate,severe,uncertain) maybe
specified.
F33.4 Recurrentdepressive disorder,currentlyinremission
D i a g n o s ti c g u i d e li n e s
For a definite diagnosis:
(a)the criteriaforrecurrentdepressive disorder(F33.-) shouldhave beenfulfilledinthe past,butthe
currentstate shouldnotfulfil the criteriafordepressive episode of anydegree of severityorforany
otherdisorderinF30 - F39; and (b)atleasttwoepisodesshouldhave lastedaminimumof 2 weeksand
shouldhave beenseparatedbyseveral monthswithoutsignificantmooddisturbance. Otherwise the
diagnosisshouldbe otherrecurrentmood[affective]disorder(F38.1).
Thiscategorycan still be usedif the patientisreceivingtreatmenttoreduce the riskof furtherepisodes.
F33.8 Otherrecurrentdepressivedisorders](https://image.slidesharecdn.com/icd-161127112927/85/Icd-91-320.jpg)
![92
F33.9 Recurrentdepressive disorder,unspecified
Includes: monopolardepressionNOS
F34 Persistentmood[affective] disorders
These are persistentandusuallyfluctuatingdisordersof moodinwhichindividual episodesare rarelyif
eversufficientlysevere towarrant beingdescribedashypomanicorevenmilddepressive episodes.
Because theylastforyears at a time,andsometimesforthe greaterpartof the individual'sadultlife,
theyinvolve considerable subjectivedistressanddisability.Insome instances,however,recurrentor
single episodesof manicdisorder,ormildorsevere depressive disorder,maybecome superimposedon
a persistentaffectivedisorder.The persistentaffective disordersare classifiedhere ratherthanwiththe
personalitydisordersbecause of evidencefromfamilystudiesthattheyare geneticallyrelatedtothe
mooddisorders,andbecause theyare sometimesamenable tothe same treatmentsasmooddisorders.
Both early- andlate- onsetvarietiesof cyclothymiaanddysthymiaare described,and shouldbe
specifiedassuchif required.
F34.0 CyclothymiaA persistentinstabilityof mood,involvingnumerousperiodsof milddepressionand
mildelation.Thisinstabilityusuallydevelopsearlyinadultlifeandpursuesachroniccourse,althoughat
timesthe moodmay be normal and stable formonthsat a time.The moodswingsare usuallyperceived
by the individual asbeingunrelatedtolife events.The diagnosisisdifficulttoestablishwithouta
prolongedperiodof
-107-
observationoran unusuallygoodaccountof the individual'spastbehaviour.Because the moodswings
are relativelymildandthe periodsof moodelevationmaybe enjoyable,cyclothymiafrequentlyfailsto
come to medical attention.Insome casesthismaybe because the moodchange,althoughpresent,is
lessprominentthancyclical changesinactivity,self-confidence,sociability,orappetitive behaviour.If
required,age of onsetmaybe specifiedasearly(inlate teenage orthe twenties) orlate.
Diagnosticguidelines
The essential featureisapersistentinstabilityof mood,involvingnumerousperiodsof milddepression
and mildelation,noneof whichhasbeensufficientlysevere orprolongedtofulfil the criteriaforbipolar
affective disorder(F31.-) orrecurrentdepressivedisorder(F33.-).Thisimpliesthatindividual episodesof
moodswingsdonot fulfil the criteriaforanyof the categoriesdescribedundermanicepisode (F30.-) or
depressiveepisode(F32.-).
Includes:affective personalitydisordercycloidpersonalitycyclothymicpersonality
Differential diagnosis.Thisdisorderiscommoninthe relativesof patientswithbipolaraffective disorder
(F31.-) and some individualswithcyclothymiaeventuallydevelopbipolaraffective disorderthemselves.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-92-320.jpg)
![93
It may persistthroughoutadultlife,cease temporarilyorpermanently,ordevelopintomore severe
moodswingsmeetingthe criteriaforbipolaraffective disorder(F31.-) orrecurrentdepressivedisorder
(F33.-)
F34.1 DysthymiaA chronicdepressionof moodwhichdoesnotcurrentlyfulfil the criteriaforrecurrent
depressivedisorder,mildormoderate severity(F33.0of F33.1), in termsof eitherseverityordurationof
individualepisodes,althoughthe criteriaformilddepressive episode mayhave beenfulfilledinthe past,
particularlyatthe onsetof the disorder.The balance betweenindividual phasesof milddepressionand
interveningperiodsof comparative normalityisveryvariable.Sufferersusuallyhave periodsof daysor
weekswhentheydescribe themselves aswell,butmostof the time (oftenformonthsata time) they
feel tiredanddepressed;everythingisaneffortandnothingisenjoyed.Theybroodandcomplain,sleep
badlyand feel inadequate,butare usuallyable tocope withthe basicdemandsof everydaylife.
Dysthymiathereforehasmuchincommonwiththe conceptsof depressive neurosisandneurotic
depression.If required,age of onsetmaybe specifiedasearly(inlate teenage orthe twenties) orlate.
Diagnosticguidelines
The essential featureisaverylong-standingdepressionof moodwhichisnever,oronlyveryrarely,
severe enoughtofulfil the criteriaforrecurrentdepressive disorder,mildormoderate severity(F33.0or
F33.1). It usuallybeginsearlyinadultlifeandlastsforat leastseveral years,sometimesindefinitely.
Whenthe onsetislater inlife,the
-108-
disorderisoftenthe aftermathof a discrete depressive episode (F32.-) andassociatedwith
bereavementorotherobviousstress.
Includes:depressive neurosis depressive personalitydisorder neuroticdepression(withmore than2
years'duration) persistentanxietydepression
Excludes:anxietydepression(mildornotpersistent) (F41.2) bereavementreaction,lastinglessthan2
years(F43.21, prolonged depressivereaction) residualschizophrenia(F20.5)
F34.8 Otherpersistentmood[affective] disordersA residual categoryforpersistentaffective disorders
that are notsufficientlysevere orlong- lastingtofulfil the criteriaforcyclothymia(F34.0) ordysthymia
(F34.1) but that are neverthelessclinicallysignificant.Some typesof depressionpreviouslycalled
"neurotic"are includedhere,providedthattheydonot meetthe criteriaforeithercyclothymia(F34.0)
or dysthymia(F34.1) or for depressive episodeof mild(F32.0) ormoderate (F32.1) severity.
F34.9 Persistentmood[affective]disorder,unspecified
F38 Othermood[affective] disorders](https://image.slidesharecdn.com/icd-161127112927/85/Icd-93-320.jpg)
![94
F38.0 Othersingle mood[affective] disordersF38.00Mixedaffective episodeAnaffective episode
lastingforat least2 weeks,characterizedbyeitheramixture ora rapidalternation(usuallywithinafew
hours) of hypomanic,manic,anddepressivesymptoms.
F38.1 Otherrecurrentmood[affective] disorders F38.10 Recurrentbrief depressive disorderRecurrent
brief depressive episodes,occurringaboutonce a monthoverthe past year.The individual depressive
episodesall lastlessthan2weeks(typically2-3days,withcomplete recovery) butfulfil the symptomatic
criteriaformild,moderate,orsevere depressiveepisode (F32.0,F32.1, F32.2).
Differential diagnosis.Incontrasttothose withdysthymia(F34.1),patientsare notdepressedforthe
majorityof the time.If the depressiveepisodesoccuronlyin relationtothe menstrual cycle,F38.8
shouldbe usedwitha secondcode forthe underlyingcause (N94.8,otherspecifiedconditions
associatedwithfemalegenitalorgansandmenstrual cycle).
F38.8 Otherspecifiedmood[affective] disordersThisisaresidual categoryforaffectivedisordersthat
do notmeetthe criteriafor anyothercategoriesF30 - F38.1 above.
-109-
F39 Unspecifiedmood[affective] disorder
To be usedonlyasa lastresort,whennootherterm can be used.
Includes:affective psychosisNOS
Excludes:mental disorderNOS(F99)
-110-
F40-F48 Neurotic,stress-relatedandsomatoformdisorders
Overviewof thisblock
F40 Phobicanxietydisorders F40.0Agoraphobia .00 Withoutpanicdisorder .01 Withpanic disorder
F40.1 Social phobias F40.2 Specific(isolated) phobias F40.8Otherphobicanxietydisorders F40.9
Phobicanxietydisorder,unspecified F41Otheranxietydisorders F41.0 Panicdisorder[episodic
paroxysmal anxiety] F41.1Generalizedanxiety disorder F41.2 Mixedanxietyanddepressivedisorder
F41.3 Othermixedanxietydisorders F41.8 Otherspecifiedanxietydisorders F41.9Anxietydisorder,
unspecified F42Obsessive-compulsive disorder F42.0 Predominantlyobsessional thoughtsor
ruminations F42.1 Predominantlycompulsive acts[obsessional rituals] F42.2 Mixedobsessional
thoughtsandacts F42.8 Otherobsessive-compulsive disorders F42.9 Obsessive-compulsivedisorder,
unspecified F43Reactionto severe stress,andadjustmentdisorders F43.0 Acute stressreaction F43.1
Post-traumaticstressdisorder F43.2 Adjustmentdisorders .20 Brief depressivereaction .21 Prolonged](https://image.slidesharecdn.com/icd-161127112927/85/Icd-94-320.jpg)
![95
depressivereaction .22 Mixedanxietyanddepressive reaction .23 Withpredominantdisturbanceof
otheremotions .24 With predominantdisturbance of conduct .25 With mixeddisturbance of
emotionsandconduct .28 With otherspecifiedpredominantsymptoms F43.8Otherreactionsto
severe stress F43.9 Reactiontosevere stress,unspecified
-111-
F44 Dissociative [conversion] disorders F44.0Dissociative amnesia F44.1 Dissociative fugue F44.2
Dissociative stupor F44.3Trance and possessiondisorders F44.4 Dissociative motordisorders F44.5
Dissociative convulsions F44.6 Dissociative anaesthesia andsensoryloss F44.7Mixeddissociative
[conversion] disorders F44.8 Otherdissociative[conversion] disorders .80 Ganser's syndrome .81
Multiple personalitydisorder.82 Transientdissociative[conversion] disordersoccurringinchildhood
and adolescence .88 Otherspecifieddissociative [conversion] disorders F44.9Dissociative
[conversion] disorder,unspecified F45 Somatoformdisorders F45.0 Somatizationdisorder F45.1
Undifferentiatedsomatoformdisorder F45.2 Hypochondriacal disorder F45.3 Somatoformautonomic
dysfunction .30 Heart andcardiovascularsystem .31 Uppergastrointestinaltract .32 Lower
gastrointestinal tract .33 Respiratorysystem .34 Genitourinarysystem .38 Otherorgan or system
F45.4 Persistentsomatoform paindisorder F45.8 Othersomatoformdisorders F45.9 Somatoform
disorder,unspecified F48 Otherneuroticdisorders F48.0 Neurasthenia F48.1 Depersonalization-
derealizationsyndrome F48.8Other specifiedneuroticdisorders F48.9 Neuroticdisorder,unspecified
-112-
Introduction
Neurotic,stress-related,andsomatoformdisordershave beenbroughttogetherinone large overall
groupbecause of theirhistorical associationwiththe conceptof neurosisandthe associationof a
substantial (thoughuncertain)proportionof these disorderswithpsychological causation. Asnotedin
the general introductiontothisclassification,the conceptof neurosishasnotbeenretainedasa major
organizingprinciple,butcare hasbeentakentoallow the easyidentificationof disordersthatsome
usersstill mightwishtoregardas neuroticintheirownusage of the term(see note onneurosisinthe
general introduction(page3).
Mixturesof symptomsare common(coexistentdepressionandanxietybeingbyfarthe mostfrequent),
particularlyinthe lesssevere varietiesof these disordersoftenseeninprimarycare. Althoughefforts
shouldbe made to decide whichisthe predominantsyndrome,acategoryisprovidedforthose casesof
mixeddepressionandanxietyinwhichitwouldbe artificial toforce adecision(F41.2).
F40 Phobicanxietydisorders](https://image.slidesharecdn.com/icd-161127112927/85/Icd-95-320.jpg)



![99
disorder(F45.2) or delusional disorder(F22.0),dependinguponthe strengthandpersistence of their
conviction.
F40.8 Otherphobicanxietydisorders F40.9 Phobicanxietydisorder,unspecified
Includes:phobiaNOS phobicstatesNOS
-115-
F41 Otheranxietydisorders
Manifestationsof anxietyare the majorsymptomsof these disordersandare not restrictedtoany
particularenvironmental situation. Depressiveandobsessionalsymptoms,andevensome elementsof
phobicanxiety,mayalsobe present,providedthattheyare clearlysecondaryorlesssevere.
F41.0 Panicdisorder[episodicparoxysmal anxiety] The essential featuresare recurrentattacksof severe
anxiety(panic) whichare notrestrictedtoany particularsituationorsetof circumstances,andwhichare
therefore unpredictable. Asinotheranxietydisorders,the dominantsymptomsvaryfrompersonto
person,butsuddenonsetof palpitations,chestpain,chokingsensations,dizziness,andfeelingsof
unreality(depersonalizationorderealization) are common. There isalso,almostinvariably,asecondary
fearof dying,losingcontrol,orgoingmad. Individual attacksusuallylastforminutesonly,though
sometimeslonger; theirfrequencyandthe course of the disorderare both rathervariable. Anindividual
ina panicattack oftenexperiencesacrescendoof fearand autonomicsymptomswhichresultsinan
exit,usuallyhurried,fromwhereverhe orshe may be. If thisoccurs ina specificsituation,suchasona
busor ina crowd, the patientmaysubsequentlyavoidthatsituation. Similarly,frequentand
unpredictablepanicattacksproduce fearof beingalone orgoingintopublicplaces. A panicattack is
oftenfollowedby apersistentfearof havinganotherattack.
Diagnosticguidelines
In thisclassification,apanicattack that occurs inan establishedphobicsituationisregardedasan
expressionof the severityof the phobia,whichshouldbe givendiagnosticprecedence. Panicdisorder
shouldbe the maindiagnosisonlyinthe absence of anyof the phobiasinF40.-.
For a definite diagnosis,several severe attacksof autonomicanxietyshouldhave occurredwithina
periodof about1 month:
(a)incircumstances where thereisnoobjective danger; (b)withoutbeingconfinedtoknownor
predictable situations;and(c)withcomparativefreedomfromanxietysymptomsbetweenattacks
(althoughanticipatoryanxietyiscommon). Includes:panicattack panicstate
Differential diagnosis. Panicdisordermustbe distinguishedfrompanicattacksoccurringas part of
establishedphobicdisordersasalreadynoted. Panicattacksmay be secondaryto depressive disorders,](https://image.slidesharecdn.com/icd-161127112927/85/Icd-99-320.jpg)



![103
Althoughobsessionalthoughtsandcompulsive actscommonlycoexist,itisusefultobe able tospecify
one setof symptomsaspredominantinsome individuals,since theymayrespondtodifferent
treatments.
F42.0 Predominantlyobsessional thoughtsorruminationsThese maytake the formof ideas,mental
images,orimpulsestoact. Theyare veryvariable incontentbutnearlyalwaysdistressingtothe
individual. A womanmaybe tormented,forexample,byafearthat she mighteventuallybe unable to
resistan impulse to kill the childshe loves,orbythe obscene orblasphemousandego-alienqualityof a
recurrentmental image. Sometimesthe ideasare merelyfutile,involvinganendlessandquasi-
philosophical considerationof imponderable alternatives. Thisindecisive considerationof alternativesis
an importantelementinmanyotherobsessional ruminationsandisoftenassociatedwithaninabilityto
make trivial butnecessarydecisionsinday-to-dayliving.
The relationshipbetweenobsessionalruminationsanddepressionisparticularlyclose:adiagnosisof
obsessive-compulsive disordershouldbe preferredonlyif ruminationsarise orpersistinthe absence of
a depressive disorder.
F42.1 Predominantlycompulsive acts[obsessionalrituals]The majorityof compulsive actsare
concernedwithcleaning(particularlyhand-washing),repeatedcheckingtoensure thata potentially
dangeroussituationhasnotbeenallowedtodevelop,ororderlinessandtidiness. Underlyingthe overt
behaviourisafear,usuallyof dangereithertoor causedby the patient,andthe ritual act is an
ineffectual orsymbolicattempttoavertthatdanger. Compulsive ritual actsmayoccupymanyhours
everydayand are sometimesassociatedwithmarkedindecisivenessandslowness. Overall,theyare
equallycommoninthe twosexesbuthand-washingritualsare more commoninwomenandslowness
withoutrepetitionismore commoninmen.
Compulsiveritual actsare lesscloselyassociatedwithdepressionthanobsessional thoughtsandare
more readilyamenable tobehavioural therapies.
F42.2 Mixedobsessional thoughtsandactsMost obsessive-compulsive individualshave elementsof
bothobsessional thinkingandcompulsivebehaviour. Thissubcategoryshouldbe usedif the twoare
equallyprominent,asisoftenthe case,butitis useful tospecifyonlyone if itisclearlypredominant,
since thoughtsandacts may respondtodifferenttreatments.
F42.8 Otherobsessive-compulsive disorders F42.9 Obsessive-compulsivedisorder,unspecified
F43 Reactiontosevere stress,andadjustmentdisorders
Thiscategorydiffersfromothersinthatit includesdisordersidentifiablenotonlyongroundsof
symptomatologyandcourse butalsoonthe basisof one or otherof twocausative influences - an
exceptionallystressful life eventproducinganacute stressreaction,ora significantlifechange leading
to continuedunpleasantcircumstancesthatresultinanadjustmentdisorder. Lesssevere psychosocial
stress("life events")mayprecipitatethe onsetorcontribute tothe](https://image.slidesharecdn.com/icd-161127112927/85/Icd-103-320.jpg)




![108
F43.22 Mixedanxietyanddepressive reactionBothanxietyanddepressive symptomsare prominent,
but at levelsnogreaterthanspecifiedinmixedanxietyanddepressive disorder(F41.2) or othermixed
anxietydisorder(F41.3).
F43.23 Withpredominantdisturbanceof otheremotionsThe symptomsare usuallyof several typesof
emotion,suchasanxiety,depression,worry,tensions,andanger. Symptomsof anxietyanddepression
may fulfil the criteriaformixedanxietyanddepressive disorder(F41.2) orothermixedanxietydisorder
(F41.3), buttheyare not sopredominantthatothermore specificdepressive oranxietydisorderscanbe
diagnosed. Thiscategoryshouldalsobe usedforreactionsinchildreninwhichregressive behaviour
such as bed-wettingorthumb-suckingare alsopresent.
F43.24 Withpredominantdisturbanceof conductThe maindisturbance isone involvingconduct,e.g.an
adolescentgrief reactionresultinginaggressive ordissocialbehaviour.
F43.25 Withmixeddisturbance of emotionsandconductBothemotional symptomsanddisturbance of
conduct are prominentfeatures.
F43.28 Withotherspecifiedpredominantsymptoms
F43.8 Otherreactionsto severe stress
F43.9 Reactionto severe stress,unspecified F44 Dissociative [conversion] disorders
The common theme sharedbydissociative (orconversion) disordersisapartial or complete lossof the
normal integrationbetweenmemoriesof the past,awarenessof identity,immediate sensations,and
control of bodilymovements. There isnormallyaconsiderable degree of consciouscontrol overthe
memoriesandsensationsthatcan be selectedforimmediateattention,andthe movementsthatare to
be carriedout. In the dissociative disordersitispresumedthatthisabilitytoexercise aconsciousand
selectivecontrol isimpaired,toa degree thatcan varyfrom dayto day or evenfromhour to hour. It is
usuallyverydifficulttoassessthe extenttowhichsome of the lossof functionsmightbe under
voluntarycontrol.
These disordershave previouslybeenclassifiedasvarioustypesof "conversionhysteria",butitnow
seemsbesttoavoidthe term"hysteria"asfar as possible,inview of itsmanyandvaried
-123-
meanings. Dissociative disordersasdescribedhere are presumedtobe "psychogenic"inorigin,being
associatedcloselyintime withtraumaticevents,insoluble andintolerable problems,ordisturbed
relationships. Itistherefore oftenpossible tomake interpretationsandpresumptionsaboutthe
individual'smeansof dealingwithinintolerablestress,butconceptsderivedfromanyone particular
theory,suchas "unconsciousmotivation"and"secondarygain",are notincludedamongthe guidelines
or criteriafor diagnosis.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-108-320.jpg)

F44.0 Dissociative amnesiaThe mainfeature islossof memory,usuallyof importantrecentevents,
whichisnot due to organicmental disorderandistoo extensive tobe explainedbyordinary
forgetfulnessorfatigue. The amnesiaisusuallycentredontraumaticevents,suchasaccidentsor
unexpectedbereavements,andisusuallypartial andselective. The extentandcompletenessof the](https://image.slidesharecdn.com/icd-161127112927/85/Icd-109-320.jpg)




![114
observation,anduponobtaininganunderstandingof the personalityof the patient,the circumstances
surroundingthe onsetof the disorder,andthe consequencesof recoveryversuscontinueddisability.
F44.4 Dissociative motordisordersThe commonestvarietiesof dissociative motordisorderare lossof
abilitytomove the whole ora part of a limbor limbs. Paralysismaybe partial,withmovementsbeing
weakor slow,orcomplete. Variousformsandvariable degreesof incoordination(ataxia) maybe
evident,particularly inthe legs,resultinginbizarre gaitorinabilitytostandunaided(astasia-abasia).
There may alsobe exaggeratedtremblingorshakingof one ormore extremitiesorthe whole body.
There may be close resemblancetoalmostanyvarietyof ataxia,apraxia,akinesia,aphonia,dysarthria,
dyskinesia,orparalysis.
Includes:psychogenicaphonia psychogenicdysphonia
F44.5 Dissociative convulsionsDissociative convulsions(pseudoseizures) maymimicepilepticseizures
verycloselyintermsof movements,buttongue-biting,seriousbruisingdue tofalling,andincontinence
of urine are rare indissociative convulsion,andlossof consciousnessisabsentorreplacedbya state of
stuporor trance.
F44.6 Dissociative anaesthesiaandsensorylossAnaestheticareasof skinoftenhave boundarieswhich
make it clearthat theyare associatedmore withthe patient'sideasaboutbodilyfunctionsthanwith
medical knowledge. There mayalsobe differential lossbetweenthe sensorymodalitieswhichcannot
be due to a neurological lesion. Sensorylossmaybe accompaniedbycomplaintsof paraesthesia.
Loss of visionisrarelytotal indissociative disorders,andvisual disturbancesare more oftenalossof
acuity,general blurringof vision,or"tunnel vision". Inspite of complaintsof visual loss,the patient's
general mobilityandmotorperformance are oftensurprisinglywell preserved.
Dissociative deafnessandanosmiaare farlesscommonthanlossof sensationorvision. Includes:
psychogenicdeafness
F44.7 Mixeddissociative [conversion] disordersMixturesof the disordersspecifiedabove (F44.0-F44.6)
shouldbe codedhere.
-128-
F44.8 Otherdissociative [conversion] disorders
F44.80 Ganser'ssyndrome The complex disorderdescribedbyGanser,whichischaracterizedby
"approximate answers",usuallyaccompaniedbyseveral otherdissociative symptoms,oftenin
circumstancesthatsuggesta psychogenicetiology,shouldbe codedhere.
F44.81 Multiple personalitydisorderThisdisorderisrare,and controversyexistsaboutthe extentto
whichitis iatrogenicorculture-specific. The essential feature isthe apparentexistence of twoormore
distinctpersonalitieswithinanindividual,withonlyone of thembeingevidentata time. Each](https://image.slidesharecdn.com/icd-161127112927/85/Icd-114-320.jpg)
![115
personalityiscomplete,withitsownmemories,behaviour,andpreferences;these maybe inmarked
contrast to the single premorbidpersonality.
In the commonformwithtwo personalities,one personalityisusuallydominantbutneitherhasaccess
to the memoriesof the otherandthe two are almostalwaysunaware of eachother'sexistence. Change
fromone personalitytoanotherinthe firstinstance isusuallysuddenandcloselyassociatedwith
traumaticevents. Subsequentchangesare oftenlimitedtodramaticor stressful events,oroccurduring
sessionswithatherapistthatinvolve relaxation,hypnosis,orabreaction.
F44.82 Transientdissociative [conversion] disordersoccurringinchildhoodandadolescence
F44.88 Otherspecifieddissociative [conversion] disorders
Includes:psychogenicconfusion twilightstate
F44.9 Dissociative [conversion]disorder,unspecified
- 129-
F45 Somatoformdisorders
The main feature of somatoformdisordersisrepeatedpresentationof physical symptoms,together
withpersistentrequestsformedicalinvestigations,inspite of repeatednegativefindingsand
reassurancesbydoctorsthat the symptomshave nophysical basis. If any physical disordersare present,
theydo notexplainthe nature andextentof the symptomsorthe distressandpreoccupationof the
patient. Evenwhenthe onsetandcontinuationof the symptomsbearaclose relationshipwith
unpleasantlifeeventsorwithdifficultiesorconflicts,the patientusuallyresistsattemptstodiscussthe
possibilityof psychological causation;thismayevenbe the case inthe presence of obviousdepressive
and anxietysymptoms. The degree of understanding,eitherphysical orpsychological,thatcanbe
achievedaboutthe cause of the symptomsisoftendisappointingandfrustratingforbothpatientand
doctor.
In these disordersthere isoftenadegree of attention-seeking(histrionic) behaviour,particularlyin
patientswhoare resentful of theirfailure topersuade doctorsof the essentiallyphysical nature of their
illnessandof the needforfurtherinvestigationsorexaminations.
Differential diagnosis. Differentiationfromhypochondriacal delusionsusuallydependsuponclose
acquaintance withthe patient. Althoughthe beliefsare long-standingandappearto be heldagainst
reason,the degree of convictionisusuallysusceptible,tosome degreeandinthe shortterm, to
argument,reassurance,andthe performance of yetanotherexaminationorinvestigation. Inaddition,
the presence of unpleasantandfrighteningphysical sensationscanbe regardedasa culturally
acceptable explanationforthe developmentandpersistence of aconvictionof physical illness.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-115-320.jpg)








![124
Includes:Briquet'sdisorder Dhat syndrome koro latah occupational neurosis,includingwriter's
cramp psychasthenia psychasthenicneurosis psychogenicsyncope
F48.9 Neuroticdisorder,unspecified
Includes:neurosisNOSF50-F59 Behavioural syndromesassociatedwithphysiological disturbancesand
physical factors
Overviewof thisblock
F50 EatingdisordersF50.0 Anorexianervosa F50.1 Atypical anorexianervosaF50.2Bulimianervosa
F50.3 Atypical bulimianervosaF50.4Overeatingassociatedwithotherpsychological disturbancesF50.5
Vomitingassociatedwithotherpsychological disturbancesF50.8OthereatingdisordersF50.9 Eating
disorder,unspecified F51 NonorganicsleepdisordersF51.0NonorganicinsomniaF51.1Nonorganic
hypersomniaF51.2Nonorganicdisorderof the sleep - wake schedule F51.3Sleepwalking
[somnambulism]
- 137-
F51.4 Sleepterrors[nightterrors] F51.5 NightmaresF51.8OthernonorganicsleepdisordersF51.9
Nonorganicsleepdisorder,unspecified F52 Sexual dysfunction,notcausedbyorganicdisorderor
disease F52.0 Lack or lossof sexual desireF52.1Sexual aversionandlackof sexual enjoyment .10 Sexual
aversion .11 Lack of sexual enjoymentF52.2Failure of genital response F52.3Orgasmicdysfunction
F52.4 Premature ejaculationF52.5NonorganicvaginismusF52.6NonorganicdyspareuniaF52.7
Excessive sexual driveF52.8Other sexual dysfunction,notcausedbyorganicdisorderordisease F52.9
Unspecifiedsexualdysfunction,notcausedbyorganicdisorderordisease F53 Mental and behavioural
disordersassociatedwiththe puerperium, notelsewhereclassifiedF53.0Mildmental andbehavioural
disordersassociatedwiththe puerperium, notelsewhereclassifiedF53.1Severemental andbehavioural
disorders associatedwiththe puerperium, notelsewhereclassifiedF53.8Othermental andbehavioural
disordersassociatedwiththe puerperium, notelsewhereclassifiedF53.9Puerperal mental disorder,
unspecified
F54Psychological andbehavioural factorsassociated withdisordersordiseasesclassifiedelsewhere
F55Abuse of non-dependence-producingsubstancesF55.0AntidepressantsF55.1LaxativesF55.2
AnalgesicsF55.3AntacidsF55.4 VitaminsF55.5SteroidsorhormonesF55.6 Specificherbal orfolk
remediesF55.8Othersubstancesthatdo notproduce dependence F55.9Unspecified
F59Unspecifiedbehavioural syndromesassociatedwithphysiological disturbancesandphysical factors
- 138-](https://image.slidesharecdn.com/icd-161127112927/85/Icd-124-320.jpg)

![126
Prepubertal patientsmayshowfailure tomake the expectedweightgainduringthe periodof growth.
(b)The weightlossisself-inducedbyavoidance of "fatteningfoods". One ormore of the followingmay
alsobe present:self-inducedvomiting;self-inducedpurging;excessive exercise;use of appetite
suppressantsand/ordiuretics. (c)There isbody-imagedistortioninthe formof a specific
psychopathologywherebyadreadof fatnesspersistsasan intrusive,overvaluedideaandthe patient
imposesalowweightthresholdonhimself orherself. (d)A widespreadendocrine disorderinvolving the
hypothalamic- pituitary - gonadal axisismanifestinwomenasamenorrhoeaandinmenas a lossof
sexual interestandpotency. (Anapparentexceptionisthe persistence of vaginal bleedsinanorexic
womenwhoare receivingreplacementhormonal therapy,mostcommonlytakenasacontraceptive
pill.) There mayalsobe elevatedlevelsof growthhormone,raisedlevelsof cortisol,changesinthe
peripheral metabolismof the thyroidhormone,andabnormalitiesof insulinsecretion. (e)If onsetis
prepubertal,the sequenceof pubertal eventsisdelayedorevenarrested(growthceases;ingirlsthe
breastsdo notdevelopandthere isa primaryamenorrhoea;inboysthe genitalsremainjuvenile). With
recovery,pubertyisoftencompletednormally,butthe menarche islate.
Differential diagnosis. There maybe associateddepressive orobsessionalsymptoms,aswell asfeatures
of a personalitydisorder,whichmaymake differentiationdifficultand/orrequire the use of more than
one diagnosticcode. Somaticcausesof weightlossinyoungpatientsthatmustbe distinguishedinclude
chronicdebilitatingdiseases,braintumors,andintestinal disorderssuchasCrohn'sdisease ora
malabsorptionsyndrome.
Excludes: lossof appetite (R63.0) psychogeniclossof appetite(F50.8)
F50.1 Atypical anorexianervosaThistermshouldbe usedforthose individualsinwhomone ormore of
the keyfeaturesof anorexianervosa(F50.0),suchas amenorrhoeaorsignificantweightloss,isabsent,
but whootherwise presentafairlytypical clinical picture. Suchpeople are usuallyencounteredin
psychiatricliaisonservicesingeneral hospitalsorinprimarycare. Patientswhohave all the key
symptomsbutto onlya milddegree mayalsobe bestdescribedbythisterm. Thistermshouldnotbe
usedforeatingdisordersthatresemble anorexianervosabutthatare due to knownphysical illness.
F50.2 BulimianervosaBulimianervosaisasyndrome characterizedbyrepeatedboutsof overeatingand
an excessivepreoccupationwiththe control of bodyweight,leadingthe patienttoadoptextreme
measuressoas to mitigate the "fattening"effectsof ingestedfood. The termshouldbe restrictedtothe
formof the disorderthatis relatedto
[height(m)]2
- 140-
anorexianervosabyvirtue of sharingthe same psychopathology. The age andsex distributionissimilar
to that of anorexianervosa,butthe age of presentationtendstobe slightlylater. The disordermaybe
viewedasa sequel topersistentanorexianervosa(althoughthe reverse sequence mayalsooccur). A
previouslyanorexicpatientmayfirstappeartoimprove asa resultof weightgainandpossiblyareturn](https://image.slidesharecdn.com/icd-161127112927/85/Icd-126-320.jpg)

![128
F50.4 Overeatingassociatedwithotherpsychological disturbancesOvereatingthathasledto obesityas
a reactionto distressingeventsshouldbe codedhere. Bereavements,accidents,surgical operations,
and emotionallydistressingeventsmaybe followedbya"reactive obesity",especiallyinindividuals
predisposedtoweight gain.
Obesityasa cause of psychological disturbance shouldnotbe codedhere. Obesitymaycause the
individualtofeel sensitiveabouthisorher appearance andgive rise toa lack of confidence inpersonal
relationships;the subjective appraisalof bodysize maybe exaggerated. Obesityasacause of
psychological disturbance shouldbe codedinacategorysuch as F38.- (othermood[affective]
disorders),F41.2(mixedanxietyanddepressive disorder),orF48.9 (neuroticdisorder,unspecified),plus
a code fromE66.- of ICD-10 to indicate the type of obesity.
Obesityasan undesirableeffectof long-termtreatmentwithneurolepticantidepressantsorothertype
of medicationshouldnotbe codedhere,butunderE66.1 (drug-inducedobesity) plusanadditionalcode
fromChapterXX (External causes) of ICD-10,toidentifythe drug.
Obesitymaybe the motivationfordieting,whichinturnresultsinminoraffective symptoms(anxiety,
restlessness,weakness,andirritability)or,more rarely,severe depressive symptoms("dieting
depression"). The appropriate code fromF30-F39 or F40-F49 shouldbe usedtocoverthe symptomsas
above,plusF50.8 (othereatingdisorder) toindicate the dieting,plusacode fromE66.- to indicate the
type of obesity.
Includes: psychogenicovereating
Excludes: obesity(E66.-) polyphagiaNOS(R63.2)
F50.5 VomitingassociatedwithotherpsychologicaldisturbancesApartfromthe self-inducedvomiting
of bulimianervosa,repeatedvomitingmayoccurindissociative disorders(F44.-),inhypochondriacal
disorder(F45.2) whenvomitingmaybe one of several bodilysymptoms,andinpregnancywhen
emotional factorsmaycontribute torecurrentnauseaandvomiting.
Includes: psychogenichyperemesisgravidarum psychogenicvomiting
Excludes: nauseaandvomitingNOS(R11)
F50.8 Othereatingdisorders
- 142-
Includes: picaof nonorganicorigininadults psychogeniclossof appetite
F50.9 Eatingdisorder,unspecified
F51 Nonorganicsleepdisorders](https://image.slidesharecdn.com/icd-161127112927/85/Icd-128-320.jpg)




![133
clock) or an abnormal processingof the time-cuesthatdrive the biological clock(the lattermayinfact
be relatedtoan emotional and/orcognitivedisturbance).
The presentcode isreservedfor those disordersof the sleep-wake schedule inwhichpsychological
factors playthe mostimportantrole,whereascasesof presumedorganicoriginshouldbe classified
underG47.2, i.e.as non-psychogenicdisordersof the sleep-wakeschedule. Whetherornot
psychological factorsare of primaryimportance and,therefore,whetherthe presentcode orG47.2
shouldbe usedisa matterfor clinical judgementineachcase.
Diagnosticguidelines
The followingclinical featuresare essentialforadefinite diagnosis:
(a)the individual'ssleep-wakepatternisoutof synchronywiththe sleep-wake schedulethatisnormal
for a particularsocietyandsharedbymost people inthe same cultural environment; (b)insomnia
duringthe major sleepperiodandhypersomnia duringthe wakingperiodare experiencednearlyevery
day forat least1 monthor recurrentlyforshorterperiodsof time; (c)the unsatisfactoryquantity,
quality,andtimingof sleepcause markeddistressorinterferewithordinaryactivitiesindailyliving.
Wheneverthere isnoidentifiablepsychiatricorphysical cause of the disorder,the presentcode should
be usedalone. None the less,the presenceof psychiatricsymptomssuchasanxiety,depression,or
hypomaniadoesnotinvalidatethe diagnosisof anonorganicdisorderof the sleep-wake schedule,
providedthatthisdisorderispredominantinthe patient'sclinical picture. Whenotherpsychiatric
symptomsare sufficientlymarkedandpersistent,the specificmental disorder(s) shouldbe diagnosed
separately.
Includes: psychogenicinversionof circadian,nyctohemeral,orsleeprhythm
F51.3 Sleepwalking[somnambulism] Sleepwalkingorsomnambulismisastate of alteredconsciousness
inwhichphenomenaof sleepandwakefulnessare combined. Duringasleepwalkingepisode the
individualarisesfrombed,usuallyduringthe firstthirdof nocturnal sleep,andwalksabout,exhibiting
lowlevelsof awareness,reactivity,andmotorskill. A sleepwalkerwill sometimesleave the bedroom
and at timesmayactually
- 147-
walkout of the house,andis thusexposedtoconsiderable risksof injuryduringthe episode. Most
often,however,he orshe will returnquietlytobed,eitherunaidedorwhengentlyledbyanother
person. Upon awakeningeitherfromthe sleepwalkingepisodeorthe nextmorning,there isusuallyno
recall of the event.
Sleepwalkingandsleepterrors(F51.4) are verycloselyrelated. Bothare consideredasdisordersof
arousal,particularlyarousal fromthe deepeststagesof sleep(stages3and 4). Many individualshave a](https://image.slidesharecdn.com/icd-161127112927/85/Icd-133-320.jpg)
![134
positive familyhistoryforeitherconditionaswell asapersonal historyof havingexperiencedboth.
Moreover,bothconditionsare muchmore commonin childhood,whichindicatesthe role of
developmental factorsintheiretiology. Inaddition,insome cases,the onsetof these conditions
coincideswithafebrile illness. Whentheycontinue beyondchildhoodorare firstobservedin
adulthood,bothconditionstendtobe associatedwithsignificantpsychological disturbance;the
conditionsmayalsooccur forthe firsttime inoldage or in the earlystagesof dementia. Baseduponthe
clinical andpathogeneticsimilaritiesbetweensleepwalkingandsleepterrors,andthe factthat the
differentialdiagnosisof these disordersisusuallyamatterof whichof the twois predominant,they
have bothbeenconsideredrecentlytobe partof the same nosologiccontinuum. Forconsistencywith
tradition,however,aswell astoemphasize the differencesinthe intensityof clinicalmanifestations,
separate codesare providedinthisclassification.
Diagnosticguidelines
The followingclinical featuresare essentialforadefinite diagnosis:
(a)the predominantsymptomisone ormore episodesof risingfrombed,usuallyduringthe firstthirdof
nocturnal sleep,andwalkingabout; (b)duringanepisode,the individualhasa blank,staringface,is
relativelyunresponsivetothe effortsof otherstoinfluence the eventortocommunicate withhimor
her,and can be awakenedonlywithconsiderabledifficulty; (c)uponawakening(eitherfromanepisode
or the nextmorning),the individualhasnorecollectionof the episode; (d)withinseveral minutesof
awakeningfromthe episode,there isnoimpairmentof mental activityorbehaviour,althoughthere
may initiallybe ashortperiodof some confusionanddisorientation; (e)there isnoevidence of an
organicmental disordersuchas dementia,oraphysical disordersuchasepilepsy.
Differential diagnosis. Sleepwalkingshouldbe differentiatedfrompsychomotorepilepticseizures.
Psychomotorepilepsyveryseldomoccursonlyat night. Duringthe epilepticattackthe individual is
completelyunresponsive toenvironmental stimuli,andperseverativemovementssuchasswallowing
and rubbingthe handsare common. The presence of epilepticdischargesinthe EEG confirms the
diagnosis,althoughaseizure disorderdoesnotpreclude coexistingsleepwalking.
- 148-
Dissociative fugue(seeF44.1) mustalsobe differentiatedfromsleepwalking. Indissociative disorders
the episodesare muchlongerindurationandpatientsare more alertand capable of complex and
purposeful behaviours. Further,thesedisordersare rare inchildrenandtypicallybeginduringthe hours
of wakefulness.
F51.4 Sleepterrors[nightterrors] Sleepterrorsornightterrorsare nocturnal episodesof extremeterror
and panicassociatedwithintensevocalization,motility,andhighlevelsof autonomicdischarge. The
individualsitsuporgetsup witha panickyscream, usuallyduringthe firstthirdof nocturnal sleep,often
rushingto the dooras if tryingto escape,althoughhe orshe veryseldomleavesthe room. Effortsof](https://image.slidesharecdn.com/icd-161127112927/85/Icd-134-320.jpg)






![141
Impulsive type .31 Borderline type F60.4HistrionicpersonalitydisorderF60.5 Anankasticpersonality
disorderF60.6 Anxious[avoidant] personalitydisorderF60.7DependentpersonalitydisorderF60.8
OtherspecificpersonalitydisordersF60.9 Personalitydisorder,unspecified F61Mixedand other
personalitydisordersF61.01 MixedpersonalitydisordersF61.11 Troublesomepersonalitychanges
F62 Enduringpersonalitychanges,notattributabletobraindamage anddisease F62.0 Enduring
personalitychange aftercatastrophicexperience
- 155-
F62.1 Enduringpersonalitychange afterpsychiatricillnessF62.8Otherenduringpersonalitychanges
F62.9 Enduringpersonalitychange,unspecified F63 Habitand impulse disordersF63.0Pathological
gamblingF63.1 Pathological fire-setting[pyromania] F63.2Pathological stealing[kleptomania] F63.3
TrichotillomaniaF63.8Otherhabitand impulse disordersF63.9Habit and impulse disorder,unspecified
F64 GenderidentitydisordersF64.0TranssexualismF64.1Dual-role transvestismF64.2Genderidentity
disorderof childhoodF64.8OthergenderidentitydisordersF64.9Genderidentitydisorder,unspecified
F65 Disordersof sexual preference F65.0FetishismF65.1FetishistictransvestismF65.2Exhibitionism
F65.3 VoyeurismF65.4PaedophiliaF65.5SadomasochismF65.6Multiple disordersof sexual preference
F65.8 Otherdisordersof sexual preference F65.9Disorderof sexual preference,unspecified F66
Psychological andbehavioural disordersassociatedwithsexualdevelopmentandorientationF66.0
Sexual maturationdisorderF66.1 Egodystonicsexual orientationF66.2Sexual relationshipdisorder
F66.8 Otherpsychosexual developmentdisordersF66.9Psychosexual developmentdisorder,
unspecified
A fifthcharactermay be usedto indicate associationwith: . x0 Heterosexuality .x1 Homosexuality .x2
Bisexuality .x8 Other,includingprepubertal F68Otherdisordersof adultpersonalityandbehaviour
F68.0 Elaborationof physical symptomsforpsychological reasonsF68.1Intentional productionor
feigningof symptomsordisabilitieseitherphysicalorpsychological [factitiousdisorder] F68.8Other
specifieddisordersof adultpersonalityandbehaviour F69 Unspecifieddisorderof adultpersonalityand
behaviour
- 156-
Introduction
Thisblockincludesavarietyof clinicallysignificantconditionsandbehaviourpatternswhichtendtobe
persistentandare the expressionof anindividual'scharacteristiclifestyleandmode of relatingtoself
and others. Some of these conditionsandpatternsof behaviouremergeearlyinthe course of individual
development,asa resultof bothconstitutional factorsandsocial experience,whileothersare acquired
laterinlife.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-141-320.jpg)




![146
F60.5 AnankasticpersonalitydisorderPersonalitydisordercharacterizedby:
(a)feelingsof excessivedoubtandcaution; (b)preoccupationwithdetails,rules,lists,order,organization
or schedule; (c)perfectionismthatinterfereswithtaskcompletion; (d)excessive conscientiousness,
scrupulousness,andundue preoccupationwithproductivitytothe exclusionof pleasureand
interpersonalrelationships; (e)excessivepedantryandadherence tosocial conventions; (f)rigidityand
stubbornness;
- 161-
(g)unreasonable insistence bythe patientthatotherssubmittoexactlyhisorherway of doingthings,or
unreasonable reluctance toallowotherstodothings; (h)intrusionof insistentandunwelcomethoughts
or impulses.
Includes: compulsive andobsessionalpersonality(disorder) obsessive-compulsive personalitydisorder
Excludes: obsessive-compulsive disorder(F42.-)
F60.6 Anxious[avoidant] personalitydisorder
Personalitydisordercharacterizedby:
(a)persistentandpervasive feelingsof tensionandapprehension; (b)belief thatone issociallyinept,
personallyunappealing,orinferiortoothers; (c)excessive preoccupationwithbeingcriticizedor
rejectedinsocial situations;(d)unwillingnesstobecome involvedwithpeople unlesscertainof being
liked;(e)restrictionsinlifestyle because of needtohave physical security; (f)avoidance of social or
occupational activitiesthatinvolvesignificantinterpersonal contactbecause of fearof criticism,
disapproval,orrejection. Associatedfeaturesmayinclude hypersensitivitytorejectionandcriticism.
F60.7 DependentpersonalitydisorderPersonalitydisordercharacterizedby:
(a)encouragingorallowingotherstomake mostof one'simportantlife decisions; (b)subordinationof
one'sownneedstothose of othersonwhomone is dependent,andundue compliance withtheir
wishes; (c)unwillingnesstomake evenreasonabledemandsonthe peopleone dependson; (d)feeling
uncomfortable orhelplesswhenalone,because of exaggeratedfearsof inabilitytocare foroneself;
(e)preoccupationwithfearsof beingabandonedbyapersonwithwhomone hasa close relationship,
and of beinglefttocare for oneself; (f)limitedcapacitytomake everydaydecisionswithoutanexcessive
amountof advice andreassurance fromothers.
Associatedfeaturesmayinclude perceivingoneself ashelpless, incompetent,andlackingstamina.
Includes:asthenic,inadequate,passive,andself-defeatingpersonality (disorder)](https://image.slidesharecdn.com/icd-161127112927/85/Icd-146-320.jpg)




![151
F63.1 Pathological fire-setting[pyromania] The disorderischaracterizedbymultipleactsof,or attempts
at, settingfire topropertyorotherobjects,withoutapparentmotive,andbya persistentpreoccupation
withsubjectsrelatedtofire andburning. There mayalsobe an abnormal interestinfire-enginesand
otherfire-fightingequipment,inotherassociationsof fires,andincallingoutthe fire service.
Diagnosticguidelines
The essential featuresare:
(a)repeatedfire-settingwithoutanyobviousmotivesuchasmonetarygain,revenge,orpolitical
extremism; (b)anintenseinterestinwatchingfiresburn;and(c)reportedfeelingsof increasingtension
before the act,and intense excitementimmediatelyafterithasbeencarriedout.
Differential diagnosis. Pathological fire-settingshouldbe distinguishedfrom:
(a)deliberatefire-settingwithoutamanifestpsychiatricdisorder(inthese casesthere isanobvious
motive) (Z03.2,observationforsuspectedmental disorder); (b)fire-settingbyayoungpersonwith
conduct disorder(F91.1),where there isevidenceof otherdisorderedbehavioursuchas stealing,
aggression,ortruancy; (c)fire-settingbyanadultwithsociopathicpersonalitydisorder(F60.2),where
there isevidence of otherpersistentdisturbance of social
- 167-
behavioursuchasaggression,orotherindicationsof lackof concernwiththe interestsandfeelingsof
otherpeople; (d)fire-settinginschizophrenia(F20.-),whenfires are typicallystartedinresponseto
delusionalideasorcommandsfromhallucinatedvoices; (e)fire-settinginorganicpsychiatricdisorders
(F00-F09), whenfiresare startedaccidentallyasa resultof confusion,poormemory,orlackof
awarenessof the consequencesof the act,or a combinationof these factors.
Dementiaoracute organic statesmayalso leadtoinadvertentfire-setting;acute drunkenness,chronic
alcoholismorotherdrugintoxication(F10-F19) are othercauses.
F63.2 Pathological stealing[kleptomania] The disorderischaracterizedbyrepeatedfailure toresist
impulsestosteal objectsthatare notacquiredforpersonal use or monetarygain. The objectsmay
insteadbe discarded,givenaway,orhoarded.
Diagnosticguidelines
There isan increasingsense of tensionbefore,andasense of gratificationduringandimmediatelyafter,
the act. Althoughsome effortatconcealmentisusuallymade,notall the opportunitiesforthisare
taken. The theftis a solitaryact,not carriedout withan accomplice. The individual mayexpress
anxiety,despondency,andguiltbetweenepisodesof stealingfromshops(orotherpremises) butthis
doesnotpreventrepetition. Casesmeetingthisdescriptionalone,andnotsecondarytoone of the
disorderslistedbelow,are uncommon.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-151-320.jpg)






![158
F68.0 Elaborationof physical symptomsforpsychological reasonsPhysicalsymptomscompatible with
and originallydue toaconfirmedphysical disorder,disease,ordisabilitybecome exaggeratedor
prolongeddue tothe psychological state of the patient.Anattention-seeking(histrionic) behavioural
syndrome develops,whichmayalsocontainadditional (andusuallynonspecific) complaintsthatare not
of physical origin.The patientiscommonlydistressedbythispainordisabilityandisoftenpreoccupied
withworries,whichmaybe justified,of the possibilityof prolongedorprogressive disabilityorpain.
Dissatisfactionwiththe resultof treatmentorinvestigations,ordisappointmentwiththe amountof
personal attentionreceivedinwardsandclinicsmayalsobe a motivatingfactor.Some casesappearto
be clearlymotivatedbythe possibilityof financialcompensationfollowingaccidentsorinjuries,butthe
syndrome doesnotnecessarilyresolve rapidlyevenaftersuccessful litigation.
- 174-
Includes:compensationneurosis
F68.1 Intentional productionorfeigningof symptomsordisabilities,eitherphysical orpsychological
[factitiousdisorder] Inthe absence of aconfirmedphysical ormental disorder,disease,ordisability,the
individualfeignssymptomsrepeatedlyandconsistently.Forphysical symptomsthismayevenextendto
self-inflictionof cutsor abrasionstoproduce bleeding,ortoself-injectionof toxicsubstances.The
imitationof painandthe insistence uponthe presence of bleedingmaybe soconvincingandpersistent
that repeatedinvestigationsandoperationsare performedatseveral differenthospitalsorclinics,in
spite of repeatedlynegative findings.
The motivationforthisbehaviourisalmostalwaysobscure andpresumablyinternal,andthe condition
isbestinterpretedasa disorderof illnessbehaviourandthe sickrole.Individualswiththispatternof
behaviourusuallyshowsignsof anumberof othermarkedabnormalitiesof personalityand
relationships.
Malingering,definedasthe intentional productionorfeigningof eitherphysical orpsychological
symptomsordisabilities,motivatedbyexternal stressesorincentives,shouldbe codedasZ76.5 of ICD-
10, and notby one of the codesinthisbook.The commonestexternal motivesformalingeringinclude
evadingcriminal prosecution.obtainingillicitdrugs,avoidingmilitary conscriptionordangerousmilitary
duty,and attemptstoobtainsicknessbenefitsorimprovementsinlivingconditionssuchashousing.
Malingeringiscomparativelycommoninlegal andmilitarycircles,andcomparativelyuncommonin
ordinarycivilianlife.
Includes:hospital hoppersyndrome Munchhausen'ssyndrome peregrinatingpatient
Excludes:batteredbabyorchildsyndrome NOS(T74.1) factitial dermatitis(unintentionallyproduced)
(L98.1) malingering(personfeigningillness)(Z76.5) Munchhausenbyproxy(childabuse) (T74.8)](https://image.slidesharecdn.com/icd-161127112927/85/Icd-158-320.jpg)




![163
individualsare immobileorseverelyrestrictedinmobility,incontinent,andcapable atmostof onlyvery
rudimentaryformsof nonverbal communication. Theypossesslittle ornoabilitytocare fortheirown
basicneeds,andrequire constanthelpandsupervision.
Diagnosticguidelines
The IQ is under20. Comprehensionanduse of language islimitedto,atbest,understandingbasic
commandsand makingsimple requests. The mostbasicand simple visuo-spatialskillsof sortingand
matchingmay be acquired,andthe affectedpersonmaybe able withappropriate supervisionand
guidance totake a small partin domesticandpractical tasks. An organicetiologycanbe identifiedin
mostcases. Severe neurological orotherphysical disabilitiesaffectingmobilityare common,asare
epilepsyandvisual andhearingimpairments. Pervasive developmental disordersin
- 180-
theirmostsevere form,especiallyatypical autism,are particularlyfrequent,especiallyinthose whoare
mobile.
Includes: idiocy profoundmental subnormality profoundoligophrenia
F78 Othermental retardation
Thiscategoryshouldbe usedonlywhenassessmentof the degree of intellectual retardationbymeans
of the usual proceduresisrenderedparticularlydifficultorimpossible byassociatedsensoryorphysical
impairments,asinblind,deaf-mute,andseverelybehaviourallydisturbedorphysicallydisabledpeople.
F79 Unspecifiedmental retardation
There isevidence of mental retardation,butinsufficientinformationisavailable toassignthe patientto
one of the above categories.
Includes: mental deficiencyNOS mental subnormalityNOS oligophreniaNOSF80-F89 Disordersof
psychological development
Overviewof thisblock
F80 Specificdevelopmental disordersof speechandlanguage F80.0 Specificspeecharticulation
disorder F80.1 Expressivelanguage disorder F80.2 Receptive languagedisorder F80.3 Acquiredaphasia
withepilepsy[Landau-Kleffnersyndrome] F80.8 Otherdevelopmentaldisordersof speechandlanguage
F80.9 Developmental disorderof speechandlanguage,unspecified F81 Specificdevelopmental
disordersof scholasticskills F81.0 Specificreadingdisorder F81.1Specificspellingdisorder F81.2
Specificdisorderof arithmetical skills F81.3 Mixeddisorderof scholasticskills F81.8 Other
developmental disordersof scholasticskills F81.9 Developmentaldisorderof scholasticskills,](https://image.slidesharecdn.com/icd-161127112927/85/Icd-163-320.jpg)




![168
overgeneralizationsof rulesmayalsooccur,as maya lackof sentence fluencyanddifficultiesin
sequencingwhenrecountingpastevents.
- 186-
It isfrequentforimpairmentsinspokenlanguagetobe accompaniedbydelaysorabnormalitiesin
word-soundproduction.
The diagnosisshouldbe made onlywhenthe severityof the delayinthe developmentof expressive
language isoutside the limitsof normal variationforthe child'smental age,butreceptivelanguageskills
are withinnormal limits(althoughmayoftenbe somewhatbelow average). The use of nonverbal cues
(suchas smilesandgesture) and"internal"language asreflectedinimaginative ormake-believe play
shouldbe relativelyintact,andthe abilitytocommunicate sociallywithoutwordsshouldbe relatively
unimpaired. The childwill seektocommunicate inspite of the language impairmentandwill tendto
compensate forlackof speechbyuse of demonstration,gesture,mime,ornon-speechvocalizations.
However,associateddifficultiesinpeerrelationships,emotionaldisturbance,behavioural disruption,
and/oroveractivityandinattentionare notuncommon,particularlyinschool-age children. Ina minority
of casesthere maybe some associatedpartial (oftenselective) hearingloss,butthisshouldnotbe of a
severitysufficienttoaccountforthe language delay. Inadequate involvementinconversational
interchanges,ormore general environmentalprivation,mayplayamajoror contributoryrole inthe
impaireddevelopmentof expressive language. Where thisisthe case,the environmental causal factor
shouldbe notedbymeansof the appropriate Zcode fromChapterXXI of ICD-10.The impairmentin
spokenlanguage shouldhave beenevidentfrominfancywithoutanyclearprolongedphase of normal
language usage. However,ahistoryof apparentlynormal firstuse of afew single words,followedbya
setbackor failure toprogress,isnotuncommon. Includes: developmental dysphasiaoraphasia,
expressive type
Excludes: acquiredaphasiawithepilepsy[Landau-Kleffnersyndrome] (F80.3) developmentalaphasia
or dysphasia,receptive type (F80.2) dysphasiaandaphasiaNOS(R47.0) elective mutism(F94.0)
mental retardation(F70-F79) pervasive developmentaldisorders(F84.-)
F80.2 Receptive languagedisorderA specificdevelopmental disorderin whichthe child'sunderstanding
of language isbelowthe appropriatelevel forhisorhermental age. In almostall cases,expressive
language ismarkedlydisturbedandabnormalitiesinword-soundproductionare common.
Diagnosticguidelines
Failure torespondtofamiliarnames(inthe absence of nonverbalclues)bythe firstbirthday,inabilityto
identifyatleastafewcommonobjectsby18 months,or failure tofollow simple,routineinstructionsby
the age of 2 yearsshouldbe takenas significantsignsof delay. Laterdifficulties](https://image.slidesharecdn.com/icd-161127112927/85/Icd-168-320.jpg)
![169
- 187-
include inabilitytounderstandgrammatical structures(negatives,questions,comparatives,etc.),and
lack of understandingof more subtle aspectsof language (tone of voice,gesture,etc.).
The diagnosisshouldbe made onlywhenthe severityof the delayinreceptivelanguage isoutside the
normal limitsof variationforthe child'smental age,andwhenthe criteriafora pervasive developmental
disorderare not met. In almostall cases,the developmentof expressivelanguageisalsoseverely
delayedandabnormalitiesinword-soundproductionare common. Of all the varietiesof specific
developmental disordersof speechandlanguage,thishasthe highestrate of associatedsocio-
emotional-behaviouraldisturbance. Suchdisturbancesdonottake any specificform, buthyperactivity
and inattention,social ineptnessandisolationfrompeers,andanxiety,sensitivity,orundue shynessare
all relativelyfrequent. Childrenwiththe mostsevere formsof receptivelanguage impairmentmaybe
somewhatdelayedintheirsocial development,mayecholanguage thattheydonotunderstand,and
may showsomewhatrestrictedinterestpatterns. However,theydifferfromautisticchildreninusually
showingnormal social reciprocity,normal make-believe play,normal use of parentsforcomfort,near-
normal use of gesture,andonlymildimpairmentsinnonverbal communication. Some degree of high-
frequencyhearinglossisnotinfrequent,butthe degree of deafnessisnot sufficienttoaccountfor the
language impairment.
Includes: congenital auditoryimperception developmentalaphasiaordysphasia,receptivetype
developmental Wernicke'saphasia worddeafness
Excludes: acquiredaphasiawithepilepsy[Landau-Kleffnersyndrome] (F80.3) autism(F84.0, F84.1)
dysphasiaandaphasia,NOS(R47.0) or expressive type (F80.1) elective mutism(F94.0) language delay
due to deafness(H90-H91) mental retardation(F70-F79)
F80.3 Acquiredaphasiawithepilepsy[Landau-Kleffnersyndrome] A disorderinwhichthe child,having
previouslymade normal progressinlanguage development,losesbothreceptiveandexpressive
language skillsbutretainsgeneral intelligence. Onsetof the disorderisaccompaniedbyparoxysmal
abnormalitiesonthe EEG (almostalwaysfromthe temporal lobes,usuallybilateral,butoftenwithmore
widespreaddisturbance),andinthe majorityof casesalsobyepilepticseizures. Typicallythe onsetis
betweenthe agesof 3 and 7 years butthe disordercan arise earlierorlaterinchildhood. Ina quarterof
casesthe lossof language occursgraduallyovera periodof some months,butmore oftenthe lossis
abrupt,withskillsbeinglostoverdaysorweeks. The temporal associationbetweenonset of
- 188-
seizuresandlossof language israthervariable,witheitherone precedingthe otherbyafew monthsto
2 years. It ishighlycharacteristicthatthe impairmentof receptive languageisprofound,withdifficulties
inauditorycomprehensionoftenbeingthe firstmanifestationof the condition. Some childrenbecome
mute,some are restrictedtojargon-like sounds,andsome show milderdeficitsinwordfluencyand](https://image.slidesharecdn.com/icd-161127112927/85/Icd-169-320.jpg)














![184
F88 Otherdisordersof psychologicaldevelopment
Includes: developmentalagnosia
- 204-
F89 Unspecifieddisorderof psychological development
Includes: developmentaldisorderNOS
F90-F98 Behavioural andemotionaldisorderswithonsetusually occurringinchildhoodand
adolescence
F99 Unspecifiedmentaldisorder
Overviewof thissection
F90 HyperkineticdisordersF90.0 Disturbance of activityandattentionF90.1Hyperkineticconduct
disorderF90.8 OtherhyperkineticdisordersF90.9 Hyperkineticdisorder,unspecified F91Conduct
disordersF91.0 Conductdisorderconfinedtothe familycontextF91.1Unsocializedconductdisorder
F91.2 SocializedconductdisorderF91.3 Oppositional defiantdisorderF91.8Otherconduct disorders
F91.9 Conductdisorder,unspecified F92Mixeddisordersof conductandemotionsF92.0 Depressive
conduct disorderF92.8 Othermixeddisordersof conductandemotionsF92.9 Mixeddisorderof conduct
and emotions,unspecified F93Emotional disorderswithonsetspecifictochildhoodF93.0Separation
anxietydisorderof childhoodF93.1Phobicanxietydisorderof childhoodF93.2Social anxietydisorderof
childhoodF93.3 SiblingrivalrydisorderF93.8 Otherchildhoodemotional disordersF93.9 Childhood
emotional disorder,unspecified F94Disordersof social functioningwithonsetspecifictochildhoodand
adolescence F94.0Elective mutismF94.1Reactive attachmentdisorderof childhoodF94.2Disinhibited
attachmentdisorderof childhoodF94.8Otherchildhooddisordersof social functioningF94.9Childhood
disorderof social functioning,unspecified F95Tic disordersF95.0 Transienttic disorderF95.1 Chronic
motor or vocal tic disorderF95.2 Combinedvocal andmultiplemotorticdisorder [de laTourette's
syndrome]
- 205-
F95.8 Othertic disordersF95.9 Tic disorder,unspecified F98 Otherbehavioural andemotional disorders
withonsetusuallyoccurringinchildhoodandadolescenceF98.0 NonorganicenuresisF98.1Nonorganic
encopresis F98.2Feedingdisorderof infancyandchildhoodF98.3Pica of infancyandchildhoodF98.4
StereotypedmovementdisordersF98.5Stuttering[stammering] F98.6ClutteringF98.8Otherspecified
behavioural andemotional disorderswithonsetusuallyoccurringinchildhoodandadolescence
F98.9Unspecifiedbehaviouralandemotionaldisorderswithonsetusuallyoccurringinchildhoodand
adolescence F99Mental disorder,nototherwise specified](https://image.slidesharecdn.com/icd-161127112927/85/Icd-184-320.jpg)


![187
- 208-
present,andthe hyperactivityispervasiveandsevere,"hyperkineticconductdisorder"(F90.1) should
be the diagnosis.
A furtherproblemstemsfromthe factthat overactivityandinattention,of arather differentkindfrom
that whichischaracteristicof a hyperkineticdisorder,mayarise asa symptomof anxietyordepressive
disorders. Thus,the restlessnessthatistypicallypartof an agitateddepressive disordershouldnotlead
to a diagnosisof a hyperkineticdisorder. Equally,the restlessnessthatisoftenpartof severe anxiety
shouldnotleadto the diagnosisof ahyperkineticdisorder. If the criteriaforone of the anxiety
disorders(F40.-,F41.-,F43.-, or F93.-) are met,thisshouldtake precedence overhyperkineticdisorder
unlessthere isevidence,apartfromthe restlessnessassociatedwithanxiety,forthe additional presence
of a hyperkineticdisorder. Similarly,if the criteriaforamooddisorder(F30-F39) are met,hyperkinetic
disordershouldnotbe diagnosedinadditionsimplybecauseconcentrationisimpairedandthere is
psychomotoragitation. The double diagnosisshouldbe made onlywhensymptomsthatare notsimply
part of the mooddisturbance clearlyindicate the separate presence of ahyperkineticdisorder.
Acute onsetof hyperactive behaviourinachildof school age is more probablydue tosome type of
reactive disorder(psychogenicororganic),manicstate,schizophrenia,orneurological disease(e.g.
rheumaticfever).
Excludes: anxietydisorders(F41.- orF93.0) mood[affective] disorders(F30-F39) pervasive
developmental disorders(F84.-) schizophrenia(F20.-)
F90.0 Disturbance of activityandattentionThere iscontinuinguncertaintyoverthe mostsatisfactory
subdivisionof hyperkineticdisorders. However,follow-upstudiesshow thatthe outcome in
adolescence andadultlife ismuchinfluencedbywhetherornotthere isassociatedaggression,
delinquency,ordissocialbehaviour. Accordingly,the mainsubdivisionismade according tothe
presence orabsence of these associatedfeatures. The code usedshouldbe F90.0 whenthe overall
criteriaforhyperkineticdisorder(F90.-) are metbut those forF91.- (conductdisorders) are not.
Includes: attentiondeficitdisorderorsyndrome withhyperactivity attentiondeficithyperactivity
disorder
Excludes:hyperkineticdisorderassociatedwithconductdisorder(F90.1)
F90.1 HyperkineticconductdisorderThiscodingshouldbe usedwhenboththe overall criteriafor
hyperkineticdisorders(F90.-) and the overall criteriaforconductdisorders(F91.-) are met.
F90.8 Otherhyperkineticdisorders
F90.9 Hyperkineticdisorder,unspecified](https://image.slidesharecdn.com/icd-161127112927/85/Icd-187-320.jpg)

![189
Differential diagnosis. Conductdisorderoverlapswithotherconditions. The coexistence of emotional
disordersof childhood(F93.-) shouldleadtoadiagnosisof mixeddisorderof conductandemotions
(F92.-). If a case also meetsthe criteriaforhyperkineticdisorder(F90.-),thatconditionshouldbe
diagnosedinstead. However,milderormore situation-specificlevelsof overactivityandinattentiveness
are commoninchildrenwithconductdisorder,asare low self-esteemandminoremotional upsets;
neitherexcludesthe diagnosis.
Excludes: conductdisordersassociatedwithemotional disorders(F92.-) or hyperkineticdisorders
(F90.-) mood[affective] disorders(F30-F39) pervasive developmental disorders(F84.-) schizophrenia
(F20.-)
F91.0 Conductdisorderconfinedtothe familycontextThiscategorycomprisesconductdisorders
involvingdissocialoraggressive behaviour(andnotmerelyoppositional,defiant,disruptive behaviour)
inwhichthe abnormal behaviourisentirely,oralmostentirely,confinedtothe home and/orto
interactionswithmembersof the nuclearfamilyorimmediate household. The disorderrequiresthat
the overall criteriaforF91 be met;evenseverelydisturbedparent-childrelationshipsare notof
themselvessufficientfordiagnosis. There maybe stealingfromthe home,oftenspecificallyfocusedon
the moneyor possessionsof one ortwo particularindividuals. Thismaybe accompaniedbydeliberately
destructive behaviour,againoftenfocusedonspecificfamilymembers - suchasbreakingof toysor
ornaments,tearingof clothes,carvingonfurniture,ordestructionof prizedpossessions. Violence
againstfamilymembers(butnotothers) anddeliberate fire-settingconfinedtothe home are also
groundsfor the diagnosis.
Diagnosticguidelines
Diagnosisrequiresthatthere be nosignificantconductdisturbance outside the familysettingand that
the child'ssocial relationshipsoutside the familybe withinthe normal range.
In mostcasesthese family-specificconductdisorderswill have ariseninthe contextof some formof
markeddisturbance inthe child'srelationshipwithone ormore membersof the nuclearfamily. Insome
cases,for example,the disordermayhave ariseninrelationtoconflictwithanewlyarrivedstep-parent.
The nosological validityof thiscategoryremainsuncertain,butitispossible thatthese highlysituation-
specificconductdisordersdonotcarry the generally poorprognosisassociatedwithpervasive conduct
disturbances.
F91.1 UnsocializedconductdisorderThistype of conductdisorderischaracterizedbythe combinationof
persistentdissocial oraggressivebehaviour(meetingthe overall criteriaforF91 and not merely
comprisingoppositional,defiant,disruptivebehaviour),withasignificantpervasive abnormalityinthe
individual'srelationshipswithotherchildren.
- 211-
Diagnosticguidelines](https://image.slidesharecdn.com/icd-161127112927/85/Icd-189-320.jpg)




![194
multiple situations. The anxietymaytake the formof: (a)anunrealistic,preoccupyingworryabout
possible harmbefallingmajorattachmentfiguresorafearthat theywill leave andnotreturn; (b)an
unrealistic,preoccupyingworrythatsome untowardevent,suchasthe child beinglost,kidnapped,
admittedtohospital,orkilled,willseparate himorherfroma major attachmentfigure; (c)persistent
reluctance orrefusal togo to school because of fearabout separation(ratherthanforotherreasons
such as fearaboutevents at school); (d)persistentreluctance orrefusal togoto sleepwithoutbeing
nearor nexttoa majorattachmentfigure; (e)persistentinappropriate fearof beingalone,orotherwise
withoutthe majorattachmentfigure,athome duringthe day; (f)repeatednightmaresabout
separation; (g)repeatedoccurrence of physical symptoms(nausea,stomachache,headache,vomiting,
etc.) on occasionsthatinvolve separationfromamajor attachmentfigure,suchasleavinghome togoto
school; (h)excessive,recurrent distress(asshownbyanxiety,crying,tantrums,misery,apathy,orsocial
withdrawal) inanticipationof,during,orimmediatelyfollowingseparationfromamajorattachment
figure. Many situationsthatinvolve separationalsoinvolveotherpotential stressorsorsourcesof
anxiety. The diagnosisrestsonthe demonstrationthatthe commonelementgivingrise toanxietyinthe
varioussituationsisthe circumstance of separationfromamajorattachmentfigure. Thisarisesmost
commonly,perhaps,inrelationtoschool refusal (or"phobia"). Often,thisdoesrepresentseparation
anxietybutsometimes(especiallyinadolescence) itdoesnot. School refusal arisingforthe firsttime in
adolescence shouldnotbe codedhere unlessitisprimarilyafunctionof separationanxiety,andthat
anxietywasfirstevidenttoanabnormal degree duringthe preschool years. Unlessthose criteriaare
met,the syndrome shouldbe codedinone of the othercategoriesinF93 or underF40-F48.
- 216-
Excludes: mood[affective]disorders(F30-F39) neuroticdisorders(F40-F48) phobicanxietydisorder
of childhood(F93.1) social anxietydisorderof childhood(F93.2) F93.1 Phobicanxietydisorderof
childhood Children,like adults,candevelopfearthat isfocusedona wide range of objectsorsituations.
Some of these fears(orphobias),forexampleagoraphobia,are nota normal part of psychosocial
development. Whensuchfearsoccur inchildhoodtheyshouldbe codedunderthe appropriate
categoryin F40-F48.However,some fearsshow amarkeddevelopmental phase specificityandarise (in
some degree) inamajorityof children;thiswouldbe true,forexample,of fearof animalsinthe
preschool period. Diagnosticguidelines This categoryshouldbe usedonlyfordevelopmental phase-
specificfearswhentheymeetthe additional criteriathatapplytoall disordersinF93,namelythat:
(a)the onsetisduringthe developmentallyappropriate age period; (b)thedegreeof anxietyisclinically
abnormal;and (c)the anxietydoesnotformpart of a more generalizeddisorder. Excludes:
generalizedanxietydisorder(F41.1) F93.2 Social anxietydisorderof childhood A warinessof strangers
isa normal phenomenoninthe secondhalf of the firstyear of life anda degree of social apprehension
or anxietyisnormal duringearlychildhoodwhenchildrenencounternew,strange,orsocially
threateningsituations. Thiscategoryshouldtherefore be usedonlyfordisordersthatarise before the
age of 6 years,that are both unusual indegree andaccompaniedbyproblemsinsocial functioning,and
that are notpart of some more generalizedemotionaldisturbance. Diagnosticguidelines Children
withthisdisordershowapersistentorrecurrentfearand/or avoidance of strangers;suchfearmay](https://image.slidesharecdn.com/icd-161127112927/85/Icd-194-320.jpg)





![200
vocal and multiple motorticdisorder[de laTourette'ssyndrome] A formof tic disorderinwhichthere
are,or have been,multiplemotorticsandone or more vocal tics,althoughthese neednothave
occurredconcurrently. Onsetisalmostalwaysinchildhoodoradolescence. A historyof motor tics
before developmentof vocal ticsiscommon; the symptomsfrequentlyworsenduringadolescence,and
it iscommonfor the disordertopersistintoadultlife. The vocal tics are oftenmultiple withexplosive
repetitivevocalizations,throat-clearing,andgrunting,andthere maybe the use of obscene wordsor
phrases. Sometimesthere isassociatedgestural echopraxia,whichalsomaybe of an obscene nature
(copropraxia). Aswithmotortics,the vocal tics maybe voluntarilysuppressedforshortperiods,be
exacerbatedbystress,anddisappearduringsleep. F95.8 Othertic disorders F95.9 Tic disorder,
unspecified A non-recommendedresidual categoryforadisorderthatfulfilsthe generalcriteriaforatic
disorderbutinwhichthe specificsubcategoryisnotspecifiedorinwhichthe featuresdonotfulfil the
criteriaforF95.0, F95.1 or F95.2.
F98Other behavioural andemotional disorderswithonsetusuallyoccurringinchildhoodand
adolescence Thisrubric comprisesaheterogeneousgroupof disordersthatshare the characteristicof
onsetinchildhoodbutotherwisedifferinmanyrespects. Some of the conditionsrepresentwell defined
syndromes,butothersare nomore thansymptomcomplexeswhichlacknosological validity,butwhich
are includedbecauseof theirfrequencyandassociationwithpsychosocial problems,andbecause they
cannot be incorporatedintoothersyndromes. Excludes: breath-holdingattacks(R06.8) gender
identitydisorderof childhood(F64.2) hypersomnolence andmegaphagia(Kleine-Levinsyndrome)
(G47.8) obsessive-compulsivedisorder(F42.-) sleepdisorders(F51.-) F98.0 Nonorganicenuresis A
disordercharacterizedbyinvoluntaryvoidingof urine,bydayand/orbynight,whichisabnormal in
relationtothe individual'smental age andwhichisnota consequence of alack of bladdercontrol due to
any neurological disorder,toepilepticattacks,or to anystructural abnormalityof the urinarytract. The
enuresismayhave beenpresentfrombirth(i.e.anabnormal extensionof the normal infantile
incontinence) oritmayhave arisenfollowingaperiodof acquired
- 224-
bladdercontrol. The lateronset(orsecondary) varietyusuallybeginsaboutthe age of 5 to 7 years. The
enuresismayconstitute amonosymptomaticconditionoritmaybe associatedwithamore widespread
emotional orbehaviouraldisorder. Inthe lattercase there isuncertaintyoverthe mechanismsinvolved
inthe association. Emotional problemsmayarise asa secondaryconsequence of the distressorstigma
that resultsfromenuresis,the enuresismayformpartof some otherpsychiatricdisorder,orboththe
enuresisandthe emotional/behavioural disturbance mayarise inparallelfromrelatedetiological
factors. There isno straightforward,unambiguouswayof decidingbetweenthesealternativesinthe
individualcase,andthe diagnosisshouldbe made onthe basisof whichtype of disturbance (i.e.
enuresisoremotional/behaviouraldisorder) constitutesthe mainproblem. Diagnosticguidelines
There isno clear-cutdemarcationbetweenanenuresisdisorderandthe normal variationsinthe age of
acquisition of bladdercontrol. However,enuresiswouldnotordinarilybe diagnosedinachildunderthe
age of 5 yearsor witha mental age under4 years. If the enuresisisassociatedwithsome (other)](https://image.slidesharecdn.com/icd-161127112927/85/Icd-200-320.jpg)


![203
partial blindness) occur,bothshouldbe coded:eye-pokingunderF98.4 and the visual conditionunder
the appropriate somaticdisordercode.
- 227-
Excludes: abnormal involuntarymovements(R25.-) movementdisordersof organicorigin(G20-G26)
nail-biting,nose-picking,thumb-sucking(F98.8) obsessive-compulsive disorder(F42.-) stereotypies
that are part of a broaderpsychiatriccondition(suchas pervasive developmental disorder) tic
disorders(F95.-) trichotillomania(F63.3) F98.5 Stuttering[stammering] Speechthatischaracterized
by frequentrepetitionorprolongationof soundsorsyllablesorwords,or byfrequenthesitationsor
pausesthatdisruptthe rhythmicflowof speech. Minordysrhythmiasof thistype are quite commonas
a transientphase inearlychildhood,orasa minorbut persistentspeechfeatureinlaterchildhoodand
adultlife. Theyshouldbe classifiedasa disorderonlyif theirseverityissuchasmarkedlytodisturbthe
fluencyof speech. There maybe associatedmovementsof the face and/orotherpartsof the bodythat
coincide intime withthe repetitions,prolongations,orpausesinspeechflow. Stutteringshouldbe
differentiatedfromcluttering(seebelow) andfromtics. Insome casesthere may be an associated
developmental disorderof speechorlanguage,inwhichcase thisshouldbe separatelycodedunder
F80.-. Excludes: cluttering(F98.6) neurological disordergivingrise tospeechdysrhythmias(Chapter
VI of ICD-10) obsessive-compulsive disorder(F42.-) tic disorders(F95.-) F98.6 Cluttering A
rapidrate of speechwithbreakdowninfluency,butnorepetitionsorhesitations,of aseveritytogive
rise to reducedspeech intelligibility. Speechiserraticanddysrhythmic,withrapid,jerkyspurtsthat
usuallyinvolve faultyphrasingpatterns(e.g.alternatingpausesandburstsof speech,producinggroups
of wordsunrelatedtothe grammatical structure of the sentence). Excludes: neurological disorder
givingrise tospeechdysrhythmias(ChapterVI of ICD-10) obsessive-compulsive disorder(F42.-)
stuttering(F98.5) tic disorders(F95.-) F98.8 Otherspecifiedbehaviouralandemotionaldisorders
withonsetusuallyoccurringinchildhoodandadolescence Includes: attentiondeficitdisorderwithout
hyperactivity (excessive)masturbation nail-biting nose-picking
- 228-
thumb-sucking F98.9Unspecifiedbehavioural andemotional disorderswithonsetusuallyoccurringin
childhoodandadolescence
F99 Mental disorder,nototherwise specified
Non-recommendedresidual category,whennoothercode fromF00-F98 can be used.](https://image.slidesharecdn.com/icd-161127112927/85/Icd-203-320.jpg)
![204
- 229-
ANNEX OTHER CONDITIONSFROMICD-10 OFTEN ASSOCIATEDWITH MENTAL AND BEHAVIOURAL
DISORDERS
Thisappendix containsalistof conditionsinotherchaptersof ICD-10that are oftenfoundin
associationwiththe disordersinChapterV(F)itself. Theyare providedhere sothatpsychiatrists
recordingdiagnosesbymeansof the Clinical DescriptionsandDiagnosticGuidelineshave immediately
to handthe ICD termsandcodesthat cover the associateddiagnosesmostlikelytobe encounteredin
ordinaryclinical practice. The majorityof the conditions coveredare givenonlyatthe three-character
level,butfour-charactercodesare givenforaselectionof those diagnosesthatwill be usedmost
frequently.
ChapterI Certaininfectiousandparasiticdiseases(A00-B99) A50 Congenital syphilis A50.4 Late
congenital neurosyphilis[juvenile neurosyphilis] A52 Late syphilis A52.1 Symptomaticneurosyphilis
Includes: tabesdorsalis
A81 Slowvirusinfectionsof central nervoussystem A81.0 Creutzfeldt-Jakobdisease A81.1 Subacute
sclerosingpanencephalitis A81.2 Progressive multifocal leukoencephalopathy B22Human
immunodeficiencyvirus(HIV) diseaseresultinginotherspecifieddiseases B22.0 HIV disease resulting
inencephalopathy Includes: HIV dementia
ChapterII Neoplasms(C00-D48) C70.- Malignantneoplasmof meninges C71.- Malignantneoplasmof
brain C72.-Malignantneoplasmof spinal cord,cranial nervesandotherpartsof central nervoussystem
D33.-Benignneoplasmof brainandotherpartsof central nervoussystem
- 230-
D42.-Neoplasmof uncertainandunknownbehaviourof meninges D43.-Neoplasmof uncertainand
unknownbehaviourof brainandcentral nervoussystem
ChapterIV Endocrine,nutritional andmetabolicdiseases(E00-E90) E00.- Congenital iodine-deficiency
syndrome E01.- Iodine-deficiency-relatedthyroiddisordersandalliedconditions E02 Subclinical
iodine-deficiencyhypothyroidism E03 Otherhypothyroidism E03.2 Hypothyroidismdue to
medicamentsandotherexogenoussubstances E03.5 Myxoedemacoma E05.- Thyrotoxicosis
[hyperthyroidism] E15 Nondiabetichypoglycaemiccoma E22 Hyperfunctionof pituitarygland E22.0
Acromegalyandpituitarygigantism E22.1 Hyperprolactinaemia Includes: drug-induced
hyperprolactinaemia E23.- Hypofunctionandotherdisordersof pituitarygland E24.- Cushing's
syndrome E30 Disordersof puberty,not elsewhere classified E30.0 Delayedpuberty E30.1
Precociouspuberty E34 Otherendocrine disorders E34.3 Shortstature,not elsewhereclassified E51
Thiamine deficiency E51.2 Wernicke'sencephalopathy E64.- Sequelaeof malnutritionand other
nutritional deficiencies E66.- Obesity E70 Disordersof aromaticamino-acidmetabolism E70.0](https://image.slidesharecdn.com/icd-161127112927/85/Icd-204-320.jpg)
![205
Classical phenylketonuria E71Disordersof branched-chainamino-acidmetabolismandfatty-acid
metabolism
- 231-
E71.0 Maple-syrup-urinedisease E74.- Otherdisordersof carbohydrate metabolism E80.- Disorders
of porphyrinandbilirubinmetabolism
ChapterVI Diseasesof the nervoussystem(G00-G99) G00.- Bacterial meningitis,notelsewhere
classified Includes: haemophilus,pneumococcal,streptococcal,staphylococcal andother
bacterial meningitis G02.- Meningitisinotherinfectiousandparasiticdiseasesclassifiedelsewhere
G03.- Meningitisdue tootherandunspecifiedcauses G04.- Encephalitis,myelitis and
encephalomyelitis G06 Intracranial and intraspinal abscessandgranuloma G06.2 Extradural and
subdural abscess,unspecified G10 Huntington'sdisease G11.- Hereditaryataxia G20 Parkinson's
disease G21 Secondaryparkinsonism G21.0 Malignantneurolepticsyndrome G21.1 Otherdrug-
inducedsecondaryparkinsonism G21.2 Secondaryparkinsonismdue tootherexternal agents G21.3
Postencephaliticparkinsonism G24 Dystonia Includes: dyskinesia
G24.0 Drug-induceddystonia G24.3 Spasmodictorticollis G24.8 Otherdystonia Includes: tardive
dyskinesia G25.- Otherextrapyramidal andmovementdisorders Includes:restlesslegssyndrome,
drug-inducedtremor,myoclonus,chorea,tics
- 232-
G30 Alzheimer's disease G30.0 Alzheimer'sdisease withearlyonset G30.1 Alzheimer'sdisease with
late onset G30.8 OtherAlzheimer'sdisease G30.9 Alzheimer'sdisease,unspecified G31 Other
degenerative diseasesof nervoussystem, notelsewhere classified G31.0 Circumscribedbrainatrophy
Includes: Pick'sdisease
G31.1 Senile degenerationof brain,notelsewhere classified G31.2 Degenerationof nervoussystem
due to alcohol Includes: alcoholiccerebellarataxiaanddegeneration,cerebral degeneration and
encephalopathy;dysfunctionof the autonomicnervous systemdue toalcohol G31.8 Other
specifieddegenerativediseasesof the nervoussystem Includes: Subacute necrotizing
encephalopathy[Leigh] grey-matter degeneration[Alpers] G31.9 Degenerative diseaseof nervous
system,unspecified G32.-Otherdegenerativedisordersof nervoussystemindiseasesclassified
elsewhere G35 Multiple sclerosis G37 Otherdemyelinatingdiseasesof central nervoussystem
G37.0 Diffuse sclerosis Includes: periaxial encephalitis;Schilder'sdisease G40 Epilepsy
G40.0Localization-related(focal)(partial) idiopathicepilepsyandepilepticsyndromeswithseizuresof
localizedonset Includes: benignchildhoodepilepsywithcentrotemporal EEGspikesor occipital
EEG paroxysms G40.1Localization-related(focal) (partial)symptomaticepilepsyandepileptic
syndromeswithsimple partial seizures Includes: attacks withoutalterationof consciousness](https://image.slidesharecdn.com/icd-161127112927/85/Icd-205-320.jpg)


![208
Q04.- Othercongenital malformationsof brain Q05.- Spinabifida Q75.- Othercongenital
malformationsof skull andface bones Q85 Phakomatoses,notelsewhere classified Q85.0
Neurofibromatosis (nonmalignant) Q85.1 Tuberoussclerosis Q86Congenital malformation
syndromesdue toknownexogenouscauses,notelsewhere classified Q86.0 Fetal alcohol syndrome
(dysmorphic) Q90 Down'ssyndrome Q90.0 Trisomy21, meioticnondisjunction Q90.1 Trisomy21,
mosaicism(mitoticnondisjunction) Q90.2 Trisomy21, translocation Q90.9 Down's syndrome,
unspecified Q91.- Edwards' syndrome andPatau'ssyndrome Q93 Monosomiesanddeletionsfrom
the autosomes,notelsewhereclassified Q93.4 Deletionof shortarm of chromosome 5 Includes:
cri-du-chatsyndrome Q96.- Turner's syndrome Q97.-Othersex chromosome abnormalities,female
phenotype,notelsewhereclassified Q98Other sex chromosome abnormalities,malephenotype,not
elsewhere classified Q98.0 Klinefelter'ssyndromekaryotype47,XXY Q98.1 Klinefelter'ssyndrome,
male withmore thantwo X chromosomes Q98.2 Klinefelter'ssyndrome,malewith46,XXkaryotype
Q98.4 Klinefelter'ssyndrome,unspecified Q99.- Otherchromosome abnormalities,notelsewhere
classified
ChapterXVIII Symptoms,signsandabnormal clinical andlaboratoryfindings,notelsewhere classified
(R00-R99) R55 Syncope andcollapse R56 Convulsions,notelsewhereclassified R56.0 Febrile
convulsions R56.8 Otherand unspecifiedconvulsions
- 238-
R62 Lack of expectednormal physiological development R62.0 Delayedmilestone R62.8 Otherlackof
expectednormal physiological development R62.9Lack of expectednormal physiological development,
unspecified R63 Symptomsandsignsconcerningfoodandfluidintake R63.0 Anorexia R63.1
Polydipsia R63.4 Abnormal weightloss R63.5 Abnormal weightgain R78.- Findingsof drugsand
othersubstances,normallynotfoundinblood Includes:alcohol (R78.0); opiate drug(R78.1); cocaine
(R78.2); hallucinogen(R78.3);otherdrugsof addictive potential (R78.4); psychotropicdrug(R78.5);
abnormal level of lithium(R78.8) R83 Abnormal findingsincerebrospinal fluid R90.- Abnormal
findingsondiagnosticimagingof central nervoussystem R94 Abnormal resultsof functionstudies
R94.0 Abnormal resultsof functionstudiesof central nervoussystem Includes: abnormal
electroencephalogram[EEG]
ChapterXIX Injury,poisoningandcertainotherconsequencesof externalcauses(S00-T98) S06
Intracranial injury S06.0 Concussion S06.1 Traumaticcerebral oedema S06.2 Diffuse braininjury
S06.3 Focal brain injury S06.4 Epidural haemorrhage S06.5 Traumaticsubdural haemorrhage S06.6
Traumatic subarachnoidhaemorrhage S06.7 Intracranial injurywithprolongedcoma
ChapterXX External causesof morbidityandmortality(V0I-Y98) Intentional self-harm(X60-X84)
Includes: purposelyself-inflictedpoisoningorinjury;suicide](https://image.slidesharecdn.com/icd-161127112927/85/Icd-208-320.jpg)
![209
- 239 -
X60Intentional self-poisoningbyandexposure tononopioidanalgesics,antipyreticsandantirheumatics
X61Intentional self-poisoningbyandexposure toantiepileptic,sedative-hypnotic,antiparkinsonismand
psychotropicdrugs,notelsewhere classified Includes: antidepressants,barbiturates,neuroleptics,
psychostimulants X62Intentional self-poisoningbyandexposure tonarcoticsandpsychodysleptics
[hallucinogens],not elsewhereclassified Includes: cannabis(derivatives),cocaine,codeine,heroin,
lysergide [LSD], mescaline,methadone,morphine,opium(alkaloids) X63Intentional self-poisoningby
and exposure tootherdrugsactingon the autonomicnervoussystems X64Intentional self-poisoning
by andexposure tootherand unspecifieddrugsandbiological substances X65Intentional self-
poisoningbyandexposure toalcohol X66Intentional self-poisoningbyandexposure toorganic
solventsandhalogenated hydrocarbonsandtheirvapours X67Intentional self-poisoningbyand
exposure toothergasesandvapours Includes: carbon monoxide;utilitygas X68 Intentional self-
poisoningbyandexposure topesticides X69Intentional self-poisoningbyand exposure tootherand
unspecifiedchemicalsandnoxioussubstances Includes: corrosive aromatics,acidsandcaustic alkalis
X70 Intentional self-harmbyhanging,strangulationandsuffocation X71 Intentional self-harmby
drowningandsubmersion X72 Intentional self-harmbyhandgundischarge X73 Intentional self-harm
by rifle,shotgunandlargerfirearmdischarge X74 Intentionalself-harmbyotherandunspecified
firearmdischarge X75 Intentionalself-harmbyexplosivematerial X76 Intentional self-harmbyfire
and flames X77 Intentional self-harmbysteam, hotvapoursandhot objects X78 Intentional self-
harm by sharpobject
- 240-
X79 Intentional self-harmbybluntobject X80 Intentional self-harmbyjumpingfrom ahighplace
X81 Intentional self-harmbyjumpingorlyingbefore movingobject X82 Intentional self-harmby
crashingof motorvehicle X83 Intentional self-harmbyotherspecifiedmeans
Includes: crashingof aircraft, electrocution,caustic substances (exceptpoisoning) X84
Intentional self-harmbyunspecifiedmeans
Assault(X85-Y09) Includes: homicide;injuriesinflictedbyanotherpersonwithintenttoinjure or
kill,byanymeans X93 Assaultbyhandgundischarge X99 Assaultbysharpobject Y00 Assaultby
bluntobject Y04 Assaultbybodilyforce Y05 Sexual assaultbybodilyforce Y06.- Neglectand
abandonment Y07.- Othermaltreatmentsyndromes Includes: mental cruelty;physical abuse;
sexual abuse;torture
Drugs,medicamentsandbiological substancescausingadverse effectsintherapeuticuse (Y40-Y59)
Y46 Antiepilepticsandantiparkinsonismdrugs Y46.7 Antiparkinsonismdrugs Y47.- Sedatives,
hypnoticsandantianxietydrugs Y49 Psychotropicdrugs,notelsewhere classified Y49.0 Tricyclicand
tetracyclicantidepressants Y49.1 Monoamine-oxidase-inhibitorantidepressants Y49.2 Otherand
unspecifiedantidepressants Y49.3 Phenothiazineantipsychoticsandneuroleptics](https://image.slidesharecdn.com/icd-161127112927/85/Icd-209-320.jpg)
![210
- 241-
Y49.4 Butyrophenone andthioxanthene neuroleptics Y49.5 Other antipsychoticsandneuroleptics
Y49.6 Psychodysleptics[hallucinogens] Y49.7 Psychostimulantswithabusepotential Y49.8 Other
psychotropicdrugs,notelsewhere classified Y49.9 Psychotropicdrug,unspecified Y50.- Central
nervoussystemstimulants,notelsewhereclassified Y51.- Drugsprimarilyaffectingthe autonomic
nervoussystem Y57.- Otherand unspecifieddrugsandmedicaments ChapterXXI Factors
influencinghealthstatusandcontact withhealthservices(Z00-Z99) Z00General examinationand
investigationof personswithoutcomplaintandreporteddiagnosis Z00.4General psychiatric
examination,notelsewhere classified Z02Examinationandencounterforadministrativepurposes
Z02.3Examinationforrecruitmenttoarmedforces Z02.4Examinationfordrivinglicence
Z02.6Examinationforinsurance purposes Z02.7Issue of medical certificate Z03Medical observation
and evaluationforsuspecteddiseasesand conditions Z03.2Observationforsuspectedmentaland
behavioural disorders Includes:observationfordissocial behaviour,fire-setting,gangactivity,and
shoplifting,withoutmanifestpsychiatricdisorder Z04Examinationandobservation forotherreasons
Includes:examinationformedicolegalreasons Z04.6General psychiatricexamination,requestedby
authority Z50Care involvinguse of rehabilitationprocedures Z50.2Alcohol rehabilitation Z50.3Drug
rehabilitation Z50.4Psychotherapy,notelsewhere classified Z50.7Occupational therapyandvocational
rehabilitation,notelsewhereclassified Z50.8Care involvinguse of otherspecifiedrehabilitation
procedures Includes:tobacco abuse rehabilitation
- 242-
trainingin activitiesof dailyliving[ADL] Z54Convalescence Z54.3Convalescence following
psychotherapy Z55.-Problemsrelatedtoeducationandliteracy Z56.-Problemsrelatedto
employmentandunemployment Z59.-Problemsrelatedtohousingandeconomiccircumstances
Z60Problemsrelatedtosocial environment Z60.0Problemsof adjustmenttolife-cycle transitions
Z60.1Atypical parentingsituation Z60.2Livingalone Z60.3Acculturationdifficulty Z60.4Social exclusion
and rejection Z60.5Targetof perceivedadverse discriminationandpersecution Z60.8Other specified
problemsrelatedtosocial environment Z61Problemsrelatedtonegative life eventsinchildhood
Z61.0Loss of love relationshipinchildhood Z61.1Removal fromhome inchildhood Z61.2Altered
patternof familyrelationshipsinchildhood Z61.3Eventsresultinginlossof self-esteeminchildhood
Z61.4Problemsrelatedtoallegedsexual abuseof childbypersonwithinprimarysupportgroup
Z61.5Problemsrelatedtoallegedsexual abuseof childbypersonoutside primarysupportgroup
Z61.6Problemsrelatedtoallegedphysical abuse of child Z61.7Personal frighteningexperience in
childhood Z61.8Other negative lifeeventsinchildhood Z62Other problemsrelatedtoupbringing
Z62.0Inadequate parental supervisionandcontrol Z62.1Parental overprotection Z62.2Institutional
upbringing Z62.3Hostilitytowardsandscapegoatingof child Z62.4Emotional neglectof child
Z62.5Other problemsrelatedtoneglectinupbringing Z62.6Inappropriate parental pressure andother](https://image.slidesharecdn.com/icd-161127112927/85/Icd-210-320.jpg)
![211
abnormal qualitiesof upbringing Z62.8Other specifiedproblemsrelatedtoupbringing Z63Other
problemsrelatedtoprimarysupportgroup,includingfamilycircumstances Z63.0Problemsin
relationshipwithspouseorpartner Z63.1Problemsinrelationshipwithparentsandin-laws
Z63.2Inadequate familysupport Z63.3Absence of familymember
- 243-
Z63.4Disappearance and deathof familymember Z63.5Disruptionof familybyseparationanddivorce
Z63.6Dependentrelativeneedingcare at home Z63.7Other stressful lifeeventsaffectingfamilyand
household Z63.8Other specifiedproblemsrelatedtoprimarysupportgroup Z64Problemsrelatedto
certainpsychosocial circumstances Z64.0Problemsrelatedtounwantedpregnancy Z64.2Seekingand
acceptingphysical,nutritional andchemical interventionsknowntobe hazardousandharmful
Z64.3Seekingandacceptingbehavioural andpsychologicalinterventionsknowntobe hazardousand
harmful Z64.4Discord withcounsellors Includes:probationofficer;social worker Z65Problems
relatedtootherpsychosocial circumstances Z65.0Convictionincivil andcriminal proceedingswithout
imprisonment Z65.1Imprisonmentandotherincarceration Z65.2Problemsrelatedtorelease from
prison Z65.3Problemsrelatedtootherlegal circumstances Includes:arrest childcustodyor support
proceedings
Z65.4Victimof crime andterrorism(includingtorture) Z65.5Exposure todisaster,warandother
hostilities Z70.-Counsellingrelatedtosexual attitude,behaviourandorientation Z71Persons
encounteringhealthservicesforothercounsellingandmedical advice,notelsewhere classified
Z71.4Alcohol abuse counsellingandsurveillance Z71.5Drug abuse counsellingandsurveillance
Z71.6Tobacco abuse counselling Z72Problemsrelatingtolifestyle Z72.0Tobacco use Z72.1Alcohol use
Z72.2Drug use Z72.3Lack of physical exercise Z72.4Inappropriate dietandeatinghabits Z72.5High-
risksexual behaviour Z72.6Gambling andbetting Z72.8Other problemsrelatedtolifestyle Includes:
self-damagingbehaviour
- 244-
Z73Problemsrelatedtolife-managementdifficulty Z73.0Burn-out Z73.1Accentuationof personality
traits
Includes:type A behaviourpattern Z73.2Lack of relaxationorleisure Z73.3Stress,notelsewhere
classified Z73.4Inadequate social skills,notelsewhere classified Z73.5Social role conflict,notelsewhere
classified Z75Problemsrelatedtomedical facilitiesandotherhealthcare Z75.1Person awaiting
admissiontoadequate facilityelsewhere Z75.2Other waitingperiodforaninvestigationandtreatment
Z75.5Holidayrelief care Z76Personsencounteringhealthservicesinothercircumstances Z76.0Issue
of repeatprescription Z76.5Malingerer[conscioussimulation] Includes:personsfeigningillnesswith](https://image.slidesharecdn.com/icd-161127112927/85/Icd-211-320.jpg)