This document discusses cardiovascular disease and dyslipidemia. It notes that:
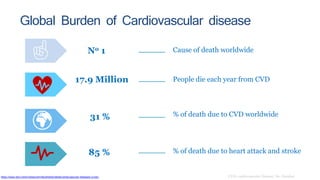
- CVD is the leading cause of death worldwide, responsible for 17.9 million deaths per year.
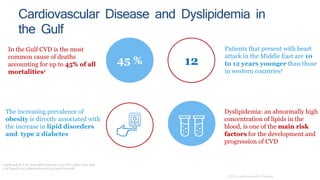
- In the Gulf region, CVD is the most common cause of death, accounting for up to 45% of all mortalities.
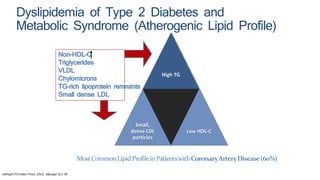
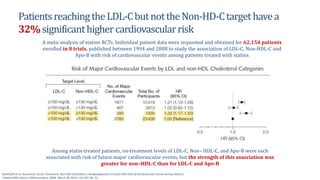
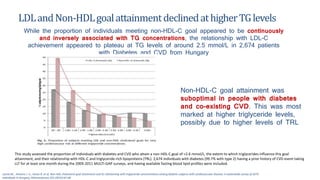
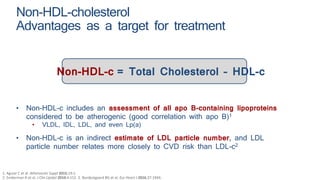
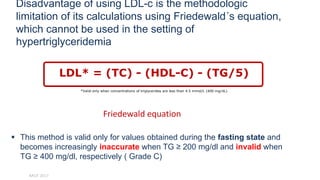
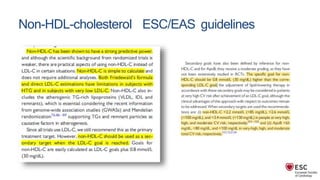
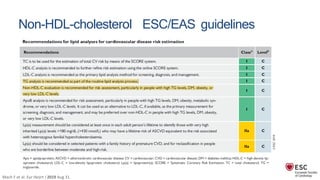
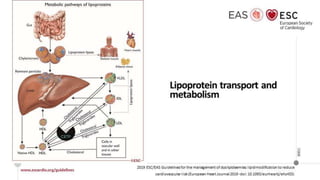
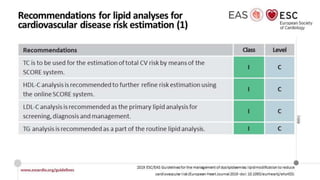
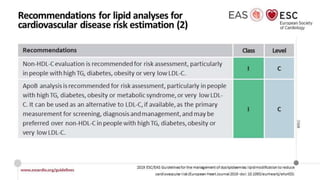
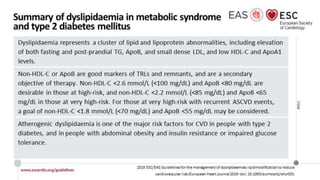
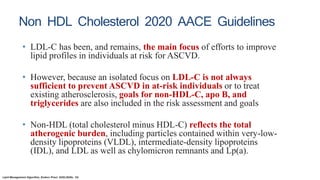
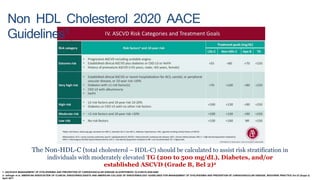
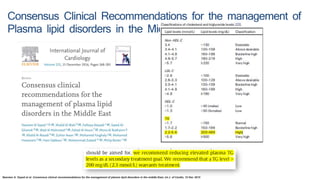
- Dyslipidemia, an abnormally high concentration of lipids in the blood, is a main risk factor for CVD. The most common dyslipidemia profile in patients with coronary artery disease involves high non-HDL cholesterol, triglycerides, and small, dense LDL particles with low HDL cholesterol.
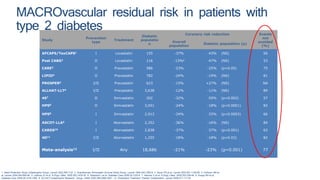
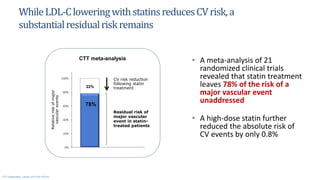
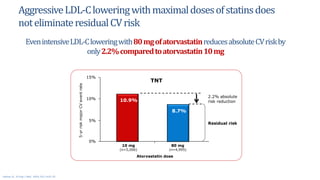
- While statin treatment lowers LDL-C and reduces CV