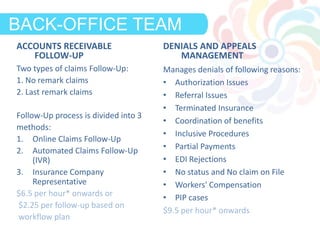
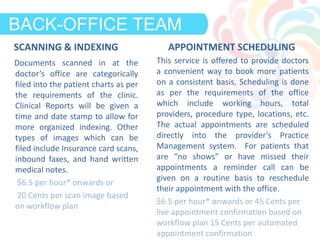
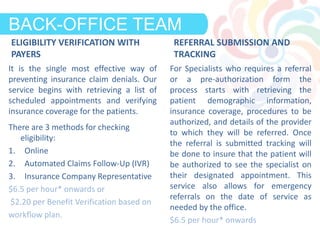
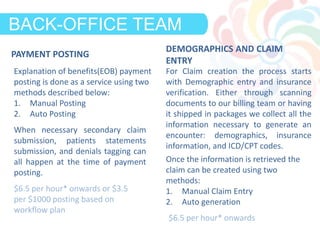
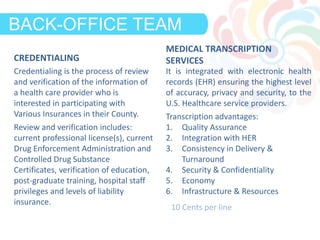
Clinicspectrum provides a hybrid workflow model that combines technology and human services to enhance healthcare operations, aiming to increase revenue by 15% and reduce costs by 30%. The model includes a back-office team that offers various services such as accounts receivable follow-up, denials management, and appointment scheduling, while leveraging a technology platform for automation and efficiency. Their comprehensive approach ensures streamlined processes in patient management, eligibility verification, credentialing, and billing, ensuring effective healthcare delivery.