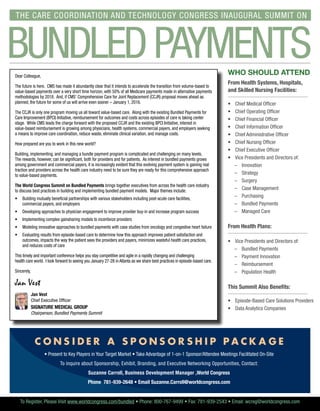
This document provides information about an opening keynote at the World Congress Summit on Bundled Payments taking place on January 27-28, 2016 in Atlanta, Georgia. The keynote will feature several speakers discussing value-based purchasing and the transformation of healthcare, including representatives from Centura, Catholic Health Initiatives, UPMC Health Plan, Golden Living, Brooks Rehabilitation, and Cleveland Clinic. Workshops will also be held on leveraging mobile technologies to reduce readmissions and creating efficient and scalable telehealth and remote patient monitoring programs. The summit aims to help healthcare organizations develop successful strategies for episode-based payment through partnerships and physician engagement.