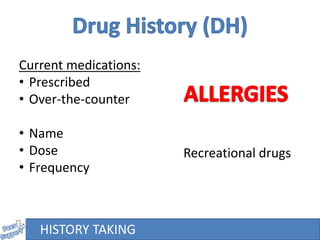
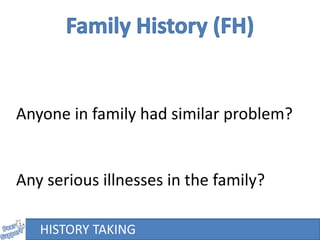
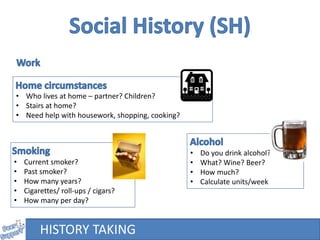
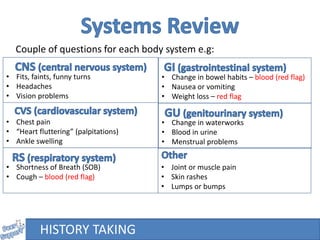
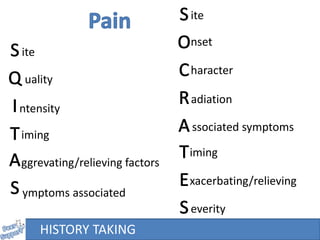
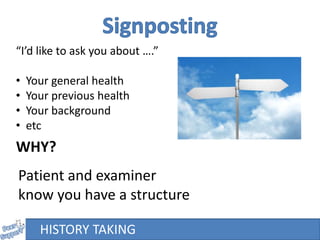
A 24-year-old female presents to her GP with abdominal pain. The document provides guidance on taking a thorough patient history, including asking open-ended questions about the chief complaint, conducting a review of systems, enquiring about medical/surgical history, medications, lifestyle/social factors, and family history. It emphasizes asking follow-up questions to fully characterize the patient's symptoms and assess for potential serious underlying conditions.