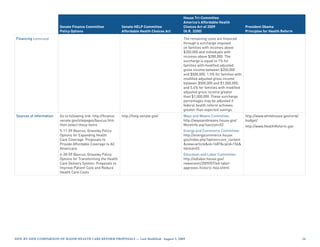
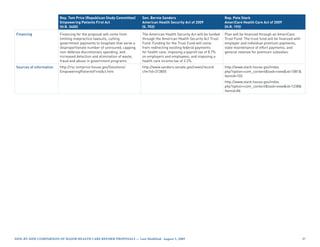
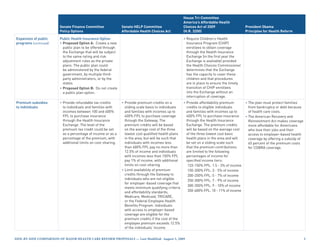
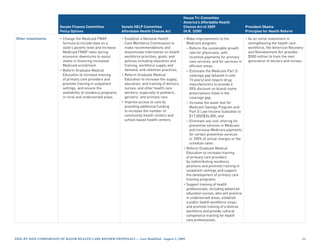
This document provides a side-by-side comparison of major health care reform proposals from the Senate Finance Committee, Senate HELP Committee, House Tri-Committee, and President Obama. It summarizes key aspects of each including the date announced, overall approach, individual and employer mandates, Medicaid/CHIP expansion, a public option, and premium subsidies. The table is regularly updated to incorporate new proposals and changes to existing proposals.
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
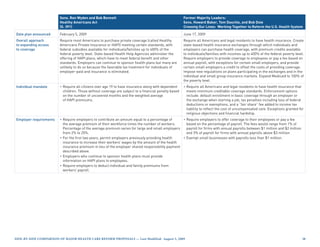
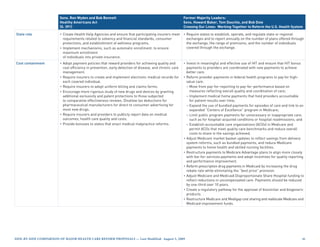
Individual mandate • Require all individuals to have • Require individuals to have • Require all individuals to have • The plan must put the country
insurance that meets minimum qualifying health coverage. “acceptable health coverage”. on a clear path to cover all
coverage standards. Enforced Enforced through a minimum Those without coverage pay Americans.
through an excise tax equal to a tax penalty of no more than a penalty of 2.5% of modified
percentage of the premium for $750 per year. Exemptions to the adjusted gross income up to
the lowest cost option available individual mandate will be granted the cost of the average national
through the Health Insurance to residents of states that do not premium for self-only or
Exchange in the area where the establish an American Health family coverage under a basic
individual resides. Exemptions will Benefit Gateway, members of plan in the Health Insurance
be granted for financial hardship; Indian tribes, those for whom Exchange. Exceptions granted for
if the lowest cost plan option affordable coverage is not dependents, religious objections,
exceeds 10% of an individual’s available, and those without and financial hardship.
income; and if the individual has coverage for fewer than 90 days.
income below 100% of the poverty
level.
Employer requirements • Proposed Option A: Require • Require employers to offer health • Require employers to offer Not specified.
employers with more than coverage to their employees and coverage to their employees and
$500,000 in total payroll per contribute at least 60% of the contribute at least 72.5% of the
year to offer coverage to their premium cost or pay $750 for premium cost for single coverage
employees and contribute at each uninsured full-time and 65% of the premium cost for
least 50% of the premium or pay employee and $375 for each family coverage of the lowest cost
an assessment. The employer uninsured part-time employee plan that meets the essential
assessment could be structured who is not offered coverage. For benefits package requirements or
in several ways: 1) a set fee per employers subject to the pay 8% of payroll into the Health
enrollee per month based on total assessment, the first 25 workers Insurance Exchange Trust Fund.
annual payroll; 2) a tiered penalty are exempted. [EL Committee amendment:
calculated as a percentage of • Exempt employers with 25 or Provide hardship exemptions
payroll; or 3) a larger penalty only fewer employees from the for employers that would be
on firms with annual payroll of requirement to provide coverage. negatively affected by job losses
more than $1,500,000. as a result of requirement.]
• Proposed Option B: No employer
“pay or play” requirement.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 2](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-2-320.jpg)
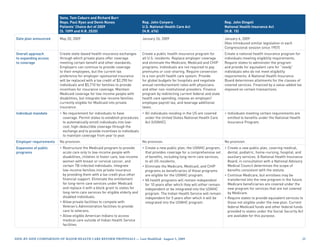
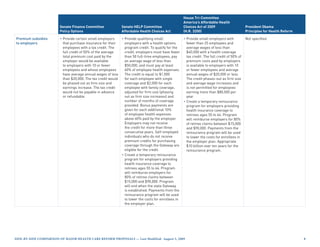
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
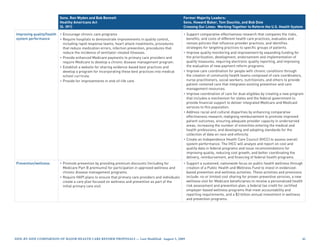
Employer requirements • Eliminate or reduce the pay
(continued) or play assessment for small
employers with annual payroll of
less than $400,000:
– Annual payroll less than
$250,000: exempt
– Annual payroll between
$250,000 and $300,000: 2% of
payroll;
– Annual payroll between
$300,000 and $350,000: 4% of
payroll;
– Annual payroll between
$350,000 and $400,000: 6% of
payroll.
[EC Committee amendment:
Extend the reduction in the pay
or play assessment for small
employers with annual payroll of
less than $750,000 and replace
the above schedule with the
following:
– Annual payroll less than
$500,000: exempt
– Annual payroll between
$500,000 and $585,000: 2% of
payroll;
– Annual payroll between
$585,000 and $670,000: 4% of
payroll;
– Annual payroll between
$670,000 and $750,000: 6% of
payroll.]
• Require employers that offer
coverage to automatically enroll
into the employer’s lowest cost
premium plan any individual who
does not elect coverage under the
employer plan or does not opt out
of such coverage.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-3-320.jpg)
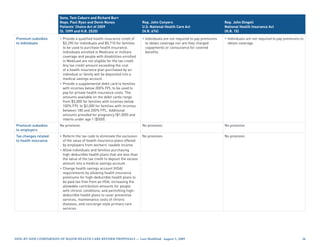
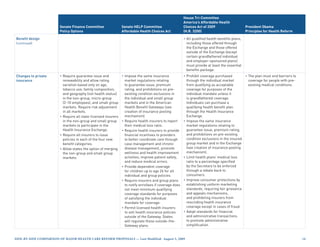
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
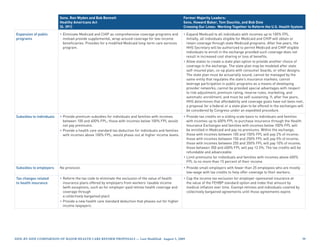
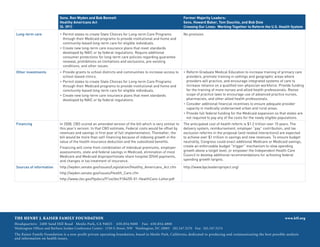
Expansion of public Medicaid • Expand Medicaid to all individuals • Expand Medicaid to all individuals • As a foundation for health
programs • Expand Medicaid to all individuals (children, pregnant women, (children, pregnant women, reform, the President signed
with incomes up to 115% FPL, parents, and adults without parents, and adults without the Children’s Health Insurance
with a possible increase in dependent children) with incomes dependent children) with incomes Program Reauthorization
eligibility for parents, pregnant up to 150% FPL. Individuals up to 133% FPL. Newly eligible, Act (CHIPRA), which provides
women, and children to a eligible for Medicaid will be non-traditional (childless adults) coverage to 11 million children.
higher level. Coverage could be covered through state Medicaid Medicaid beneficiaries may
provided through the current programs and will not be eligible enroll in coverage through the
program structure or by enrolling for credits to purchase coverage Exchange if they were enrolled
children, pregnant women, through American Health Benefit in qualified health coverage
parents, and childless adults in Gateways. during the six months before
the Health Insurance Exchange. • Grant individuals eligible for becoming Medicaid eligible.
Another alternative is to enroll the Children’s Health Insurance Provide Medicaid coverage for all
all populations except childless Program (CHIP) the option of newborns who lack acceptable
adults in Medicaid. Under this enrolling in CHIP or enrolling in coverage and provide optional
approach, childless adults would a qualified health plan through a Medicaid coverage to low-income
not be eligible for Medicaid but Gateway. HIV-infected individuals and for
would be given tax credits to family planning services to certain
purchase coverage through the low-income women. In addition,
Exchange or to buy-in to Medicaid. increase Medicaid payment
Children’s Health Insurance rates for primary care providers
Program to 100% of Medicare rates.
• After September 30, 2013, expand [EC Committee amendment:
CHIP eligibility to 275% FPL. Once Require states to submit a state
the Health Insurance Exchange is plan amendment specifying the
fully operational, CHIP enrollees payment rates to be paid under
would obtain coverage through the state’s Medicaid program.]
the Exchange and states would The coverage expansions (except
be required to continue to provide the optional expansions) and the
services not covered by plans in enhanced provider payments
the Exchange, including Early and will be fully financed with
Periodic Screening, Diagnosis, federal funds. [EC Committee
and Treatment (EPSDT) services. amendment: Replace full federal
financing for Medicaid coverage
Medicare expansions with 100% federal
• Until the Health Insurance financing through 2014 and 90%
Exchange is underway, allow federal financing beginning in year
individuals aged 55-64 without 2015.]
coverage to buy-in to Medicare at
full-cost.
• Phase-out or reduce the two-
year waiting period for Medicare
eligibility for people with
disabilities.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-4-320.jpg)
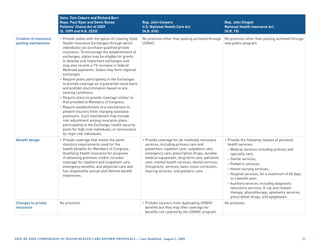
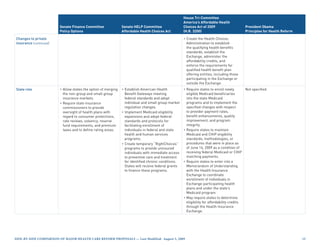
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
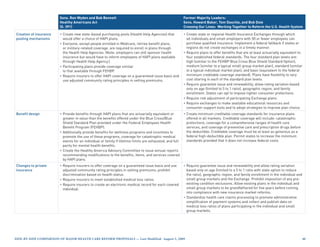
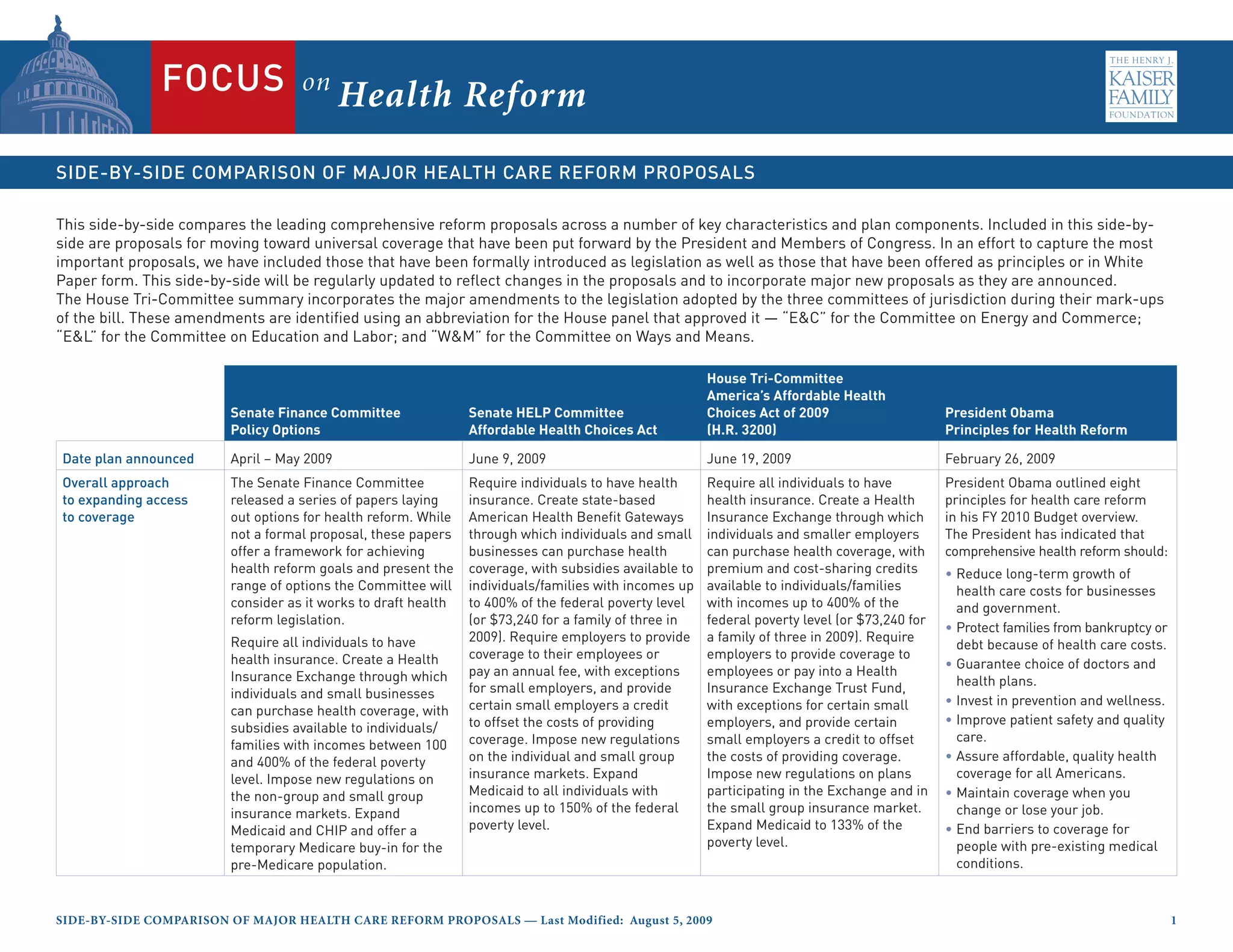
Premium subsidies [EC Committee amendment:
to individuals (continued) Replaces the above subsidy
schedule with the following:
133-150% FPL: 1.5 - 3% of income
150-200% FPL: 3 – 5.5% of income
200-250% FPL: 5.5 - 8% of income
250-300% FPL: 8 - 10% of income
300-350% FPL: 10 - 11% of income
350-400% FPL: 11 - 12% of income]
[EC Committee amendment:
Increase the affordability credits
annually by the estimated savings
achieved through adopting a
formulary in the public health
insurance option, pharmacy
benefit manager transparency
requirements, developing
accountable care organization
pilot programs in Medicaid, and
administrative simplification.]
[EC Committee amendment:
Increase the affordability credits
annually by the estimated
savings achieved through limiting
increases in premiums for plans
in the Exchange to no more than
150% of the annual increase in
medical inflation and by requiring
the Secretary to negotiate
directly with prescription drug
manufacturers to lower the prices
for Medicare Part D plans.]
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-6-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Premium subsidies • Provide affordability cost-sharing
to individuals (continued) credits to eligible individuals and
families with incomes up to 400%
FPL. The cost-sharing credits
reduce the cost-sharing amounts
and annual cost-sharing limits
and have the effect of increasing
the actuarial value of the basic
benefit plan to the following
percentages of the full value of the
plan for the specified income tier:
133-150% FPL: 97%
150-200% FPL: 93%
200-250% FPL: 85%
250-300% FPL: 78%
300-350% FPL: 72%
350-400% FPL: 70%
• Limit availability of premium and
cost-sharing credits to US citizens
and lawfully residing immigrants
who meet the income limits
and are not enrolled in qualified
or grandfathered employer or
individual coverage, Medicare,
Medicaid (except those eligible
to enroll in the Exchange),
TRICARE, or VA coverage (with
some exceptions). Individuals
with access to employer-based
coverage are eligible for the
premium and cost-sharing
credits if the cost of the employee
premium exceeds 11% of
the individuals’ income [EC
Committee amendment: To be
eligible for the premium and cost-
sharing credits, the cost of the
employee premium must exceed
12% of individuals’ income.].
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-7-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
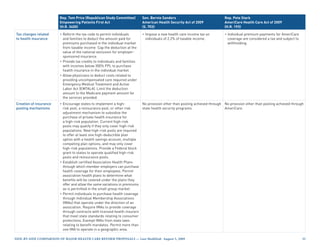
Tax changes related • Considers several health • Impose a minimum tax on • Impose a tax on individuals Not specified.
to health insurance insurance-related tax changes individuals without qualifying without acceptable health care
affecting the tax preference for health care coverage of no more coverage of 2.5% of modified
employer-sponsored insurance, than $750 per year. adjusted gross income.
health savings accounts,
flexible spending accounts, and
deductions for medical expenses.
Creation of insurance • Create one national or multiple • Create state-based American • Create a National Health Insurance • The plan should provide portability
pooling mechanisms regional Health Insurance Health Benefit Gateways, Exchange, through which individuals of coverage and should offer
Exchanges through which administered by a governmental and employers (phasing-in eligibility Americans a choice of health
individuals and small employers agency or non-profit organization, for employers starting with smallest plans.
can purchase qualified insurance. through which individuals and employers) can purchase qualified
• Require all state-licensed insurers small employers can purchase insurance, including from private
in the non-group and small group qualified coverage. States may health plans and the public health
markets to participate in the form regional Gateways or allow insurance option.
Health Insurance Exchange(s). more than one Gateway to operate • Restrict access to coverage
• Require guarantee issue and in a state as long as each Gateway through the Exchange to
renewability and allow rating serves a distinct geographic area. individuals who are not enrolled
variation based only on age, • Restrict access to coverage in qualified or grandfathered
tobacco use, family composition, through the Gateways to employer or individual coverage,
and geography (not health status) individuals who are not Medicare, Medicaid (with some
in the Exchange(s). incarcerated and who are not exceptions), TRICARE, or VA
• Require the Exchange(s) to eligible for employer-sponsored coverage (with some exceptions).
develop a standardized format coverage that meets minimum [EC Committee amendment:
for presenting insurance qualifying criteria and affordability Permit members of the armed
options, create a web portal to standards, Medicare, Medicaid, forces and those with coverage
help consumers find insurance, TRICARE, or the Federal Employee through TRICARE or the VA to
maintain a call center for Health Benefits Program. enroll in a health benefits plan
customer service, and establish offered through the Exchange.]
procedures for enrolling • Create a new public health
individuals and businesses and insurance option to be offered
for determining eligibility for tax through the Health Insurance
credits. Exchange that must meet the same
requirements as private plans
regarding benefit levels, provider
networks, consumer protections,
and cost-sharing. Require the
public plan to offer basic, enhanced,
and premium plans, and permit it to
offer premium plus plans. Finance
the costs of the public plan through
revenues from premiums.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 9](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-9-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Creation of insurance • Create a community health For the first three years, set
pooling mechanisms insurance option to be offered provider payment rates in the
(continued) through state Gateways that public plan at Medicare rates
complies with the requirements and allow bonus payments of
of being a qualified health plan. 5% for providers that participate
Require that the costs of the in both Medicare and the public
community health insurance plan plan and for pediatricians
be financed through revenues and other providers that don’t
from premiums, require the typically participate in Medicare.
plan to negotiate payment rates In subsequent years, permit the
with providers, and contract Secretary to establish a process
with qualified nonprofit entities for setting rates. [EC Committee
to administer the plan. Permit amendment: Require the public
the plan to develop innovative health insurance option to
payment policies to promote negotiate rates with providers so
quality, efficiency, and savings to that the rates are not lower than
consumers. Require each State to Medicare rates and not higher
establish a State Advisory Council than the average rates paid by
to provide recommendations on other qualified health benefit
policies and procedures for the plan offering entities.] Health
community health insurance care providers participating
option. in Medicare are considered
• Create three benefit tiers of participating providers in the
plans to be offered through the public plan unless they opt out.
Gateways based on the percentage Permit the public plan to develop
of allowed benefit costs covered by innovative payment mechanisms,
the plan: including medical home and other
– Tier 1: includes the essential care management payments,
health benefits and covers 76% value-based purchasing, bundling
of the benefit costs of the plan; of services, differential payment
– Tier 2: includes the essential rates, performance based
health benefits and covers 84% payments, or partial capitation
of the benefit costs of the plan; and modify cost sharing and
payment rates to encourage use
– Tier 3: includes the essential
of high-value services. [EC
health benefits and covers 93%
Committee amendment: Clarify
of the benefit costs of the plan.
that the public health insurance
option must meet the same
requirements as other plans
relating to guarantee issue and
renewability, insurance rating
rules, network adequacy, and
transparency of information.]
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 0](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-10-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Creation of insurance • Require guarantee issue and [EC Committee amendment:
pooling mechanisms renewability of health insurance Require the public health
(continued) policies in the individual and small insurance option to adopt a
group markets; prohibit pre- prescription drug formulary.]
existing condition exclusions; and • Create four benefit categories of
allow rating variation based only plans to be offered through the
on family structure, geography, Exchange:
the actuarial value of the health – Basic plan includes essential
plan benefit, tobacco use, and age benefits package and covers
(with only 2 to 1 variation). 70% of the benefit costs of the
• Require plans participating in plan;
the Gateway to provide coverage – Enhanced plan includes
for at least the essential health essential benefits package,
care benefits, meet network reduced cost sharing compared
adequacy requirements, and to the basic plan, and covers
make information regarding plan 85% of benefit costs of the plan;
benefits service area, premium – Premium plan includes essential
and cost sharing, and grievance benefits package with reduced
and appeal procedures available cost sharing compared to the
to consumers. enhanced plan and covers 95%
• Require states to adjust payments of the benefit costs of the plan;
to health plans based on the – Premium plus plan is a premium
actuarial risk of plan enrollees plan that provides additional
using methods established by the benefits, such as oral health and
Secretary. vision care.
• Require the Gateway to certify • Require guarantee issue and
participating health plans, provide renewability; allow rating variation
consumers with information based only on age (limited to 2 to
allowing them to choose among 1 ratio), premium rating area, and
plans (including through a family enrollment; and limit the
centralized website), contract with medical loss ratio to a specified
navigators to conduct outreach percentage.
and enrollment assistance, create
a single point of entry for enrolling
in coverage through the Gateway
or through Medicaid, CHIP or
other federal programs, and assist
consumers with the purchase
of long-term care services and
supports.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-11-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Creation of insurance • Following initial federal support, • Require plans participating
pooling mechanisms the Gateway will be funded by in the Exchange to be state
(continued) a surcharge of no more than licensed, report data as required,
4% of premiums collected by implement affordability credits,
participating health plans. meet network adequacy
standards, provide culturally and
linguistically appropriate services,
contract with essential community
providers, and participate in risk
pooling. Require participating
plans to offer one basic plan for
each service area and permit
them to offer additional plans.
[EC Committee amendment:
Require plans to provide
information related to end-of-life
planning to individuals and provide
the option to establish advance
directives and physician’s order
for life sustaining treatment.]
• Require risk adjustment of
participating Exchange plans.
• Provide information to consumers
to enable them to choose among
plans in the Exchange, including
establishing a telephone hotline
and maintaining a website and
provide information on open
enrollment periods and how to
enroll.
• [EC Committee amendment:
Prohibit plans participating in the
Exchange from discriminating
against any provider because of
a willingness or unwillingness to
provide abortions.] .
• [EC Committee amendment:
Facilitate the establishment of
non-for-profit, member-run
health insurance cooperatives
to provide insurance through the
Exchange.]
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 2](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-12-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Creation of insurance • Allow states to operate state-
pooling mechanisms based exchanges if they
(continued) demonstrate the capacity to
meet the requirements for
administering the Exchange.
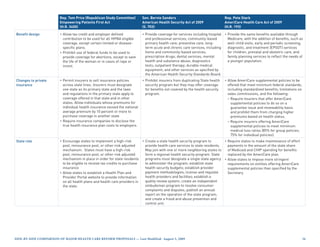
Benefit design • Create four benefit categories • Create the essential health care • Create an essential benefits Not specified.
(lowest, low, medium, and high). benefits package that provides a package that provides a
Require all plans to provide a comprehensive array of services comprehensive set of services,
comprehensive set of services and and prohibits inclusion of lifetime covers 70% of the actuarial value
prohibit inclusion of lifetime limits or annual limits on the dollar of the covered benefits, limits
on coverage or annual limits on value of the benefits. The essential annual cost-sharing to $5,000/
benefits. health benefits must be included individual and $10,000/family,
• All policies (except certain in all qualified health plans and and does not impose annual or
grandfathered employer- must be equal to the scope of lifetime limits on coverage. The
sponsored plans) must comply benefits provided by a typical Health Benefits Advisory Council,
with one of the four benefit employer plan. Create a chaired by the Surgeon General,
categories, including those offered temporary, independent will make recommendations on
through the Exchange and those commission to advise the specific services to be covered by
offered outside of the Exchange. Secretary in the development of the essential benefits package as
the essential health benefit well as cost-sharing levels. [EL
package. Committee amendment: Require
• Specify the criteria for minimum early and periodic screening,
qualifying coverage for purposes diagnostic, and treatment
of meeting the individual mandate (EPSDT) services for children
for coverage, and an affordability under age 21 be included in the
standard such that coverage is essential benefits package.] [EC
deemed unaffordable if the Committee amendment: Prohibit
premium exceeds 12.5% of an abortion coverage from being
individual’s adjusted gross income. required as part of the essential
benefits package; require
segregation of public subsidy
funds from private premiums
payments for plans that choose
to cover abortion services beyond
Hyde—which allows coverage for
abortion services to save the life
of the woman and in cases of rape
or incest; and require there be no
effect on state or federal laws on
abortions.]
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-13-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
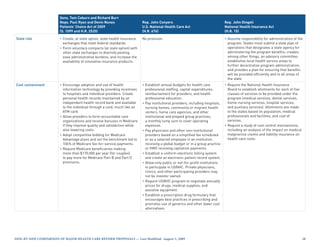
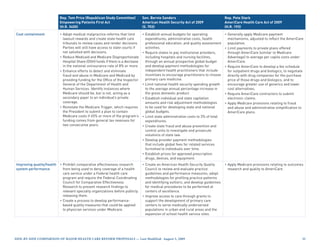
Cost containment • Encourage adoption and use of • Establish a Health Care Program • Simplify health insurance • The plan should reduce high
health information technology Integrity Coordinating Council administration by adopting administrative costs, unnecessary
by expanding eligibility for and two new federal department standards for financial and tests and services, waste, and
the Medicare HIT incentives positions to oversee policy, administrative transactions, other inefficiencies that consume
in the American Recovery and program development, and including timely and transparent money with no added benefit.
Reinvestment Act to include oversight of health care fraud, claims and denial management
additional providers. waste, and abuse in public and processes and use of standard
• Eliminate fraud, waste, and abuse private coverage. electronic transactions.
in public programs through more • Simplify health insurance • [EC Committee amendment:
intensive screening of providers, administration by adopting Limit annual increases in the
the development of the “One PI standards for financial and premiums charged under any
database” to capture and share administrative transactions, health plans participating in the
data across federal and state including timely and transparent Exchange to no more than 150%
programs, increased penalties claims and denial management of the annual percentage increase
for submitting false claims and processes and use of standard in medical inflation. Provide
violating EMTALA, and increase electronic transactions. exceptions if this limit would
funding for anti-fraud activities. threaten a health plan’s financial
• Restructure payments to Medicare viability.]
Advantage plans to promote • Modify provider payments under
efficiency and quality. Medicare including:
• Require drug or device – Modify market basket updates
manufacturers to disclose to account for productivity
payments and incentives given improvements for inpatient
to providers and any investment hospital, home health, skilled
interest held by a physician. nursing facility, and other
• Improve transparency of Medicare providers; and
information about skilled nursing – Reduce payments for
facilities. potentially preventable hospital
• Allow providers organized as readmissions.
accountable care organizations • Restructure payments to Medicare
that voluntarily meet quality Advantage plans, phasing to 100%
thresholds to share in the cost- of fee-for-services payments, with
savings they achieve for the bonus payments for quality.
Medicare program. • Increase the Medicaid drug
rebate percentage and extend
the prescription drug rebate to
Medicaid managed care plans.
Require drug manufacturers to
provide drug rebates for dual
eligibles enrolled in Part D plans.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-16-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Cost containment • [EC Committee amendment:
(continued) Require the Secretary to negotiate
directly with pharmaceutical
manufacturers to lower drug
prices for Medicare Part D plans
and Medicare Advantage Part D
plans.]
• Reduce Medicaid DSH payments
by $6 billion in 2019, imposing the
largest percentage reductions in
state DSH allotments in states
with the lowest uninsured rates
and those that do not target DSH
payments.
• Require hospitals and ambulatory
surgical centers to report on
health care-associated infections
to the Centers for Disease Control
and Prevention and refuse
Medicaid payments for certain
health care-associated conditions.
• Reduce waste, fraud, and abuse
in public programs by allowing
provider screening, enhanced
oversight periods, and enrollment
moratoria in areas identified as
being at elevated risk of fraud
in all public programs, and by
requiring Medicare and Medicaid
program providers and suppliers
to establish compliance programs.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-17-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
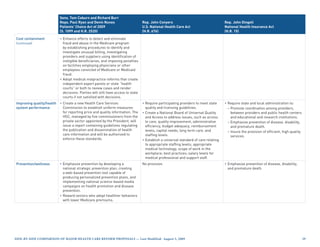
Improving quality/health • Strengthen primary care and • Develop a national strategy to • Support comparative effectiveness • The plan must ensure the
system performance chronic care management by improve the delivery of health research by establishing a Center implementation of patient safety
providing bonus payments to care services, patient health for Comparative Effectiveness measures and provide incentives
certain primary care providers outcomes, and population Research within the Agency for changes in the delivery
and providing reimbursement for health that includes publishing for Healthcare Research and system to reduce unnecessary
certain care management activities an annual national health care Quality to conduct, support, and variability in patient care. It must
for patients with hospital stays quality report card. Create an synthesize research on outcomes, support the widespread use of
related to a major chronic condition. inter-agency Working Group on effectiveness, and appropriateness health information technology
• Establish a framework to set Health Care Quality to coordinate of health care services and and the development of data
national priorities for comparative and streamline federal quality procedures. An independent on the effectiveness of medical
clinical effectiveness research. activities related to the national CER Commission will oversee interventions to improve the
• Create a Chronic Care quality strategy. the activities of the Center. [EC quality of care delivered.
Management Innovation Center • Develop, through a multi- Committee amendment: Prohibit • To lay the foundation for improving
within CMS to disseminate stakeholder process, quality use of comparative effectiveness the health care delivery system
innovations that foster patient- measures that allow assessments research findings to deny or and quality of care, the American
centered care coordination of health outcomes; continuity ration care or to make coverage Recovery and Reinvestment
innovations for high-cost, and coordination of care; safety, decisions in Medicare.] Act invests $19 billion in health
chronically ill Medicare effectiveness and timeliness • Strengthen primary care and information technology, including
beneficiaries. of care; health disparities; care coordination by increasing $17 billion in incentives to
• Bundle payments for acute, and appropriate use of health Medicaid payments for primary providers to encourage their use
inpatient hospital services and care resources. Require public care providers, providing Medicare of electronic medical records,
post-acute care services occurring reporting on quality measures bonus payments to primary care and provides $1.1 billion for
within 30 days of discharge from a through a user-friendly website. practitioners (with larger bonuses comparative effectiveness
hospital. • Create a Center for Health paid to primary care practitioners research.
• Establish a hospital value-based Outcomes Research and serving in health professional
purchasing program to pay Evaluation within the Agency shortage areas).
hospitals based on performance for Healthcare Research and • Conduct Medicare pilot programs
on quality measures. Quality to conduct and synthesize to test payment incentive models
• Develop a strategy for the research on the effectiveness for accountable care organizations
development, selection, and of health care services and and bundling of post-acute
implementation of quality procedures to provide providers care payments, and conduct
measures that involves input from and patients with information on pilot programs in Medicare and
multiple stakeholders. Improve the most effective therapies for Medicaid to assess the feasibility
public reporting of quality and preventing and treating health of reimbursing qualified patient-
performance information that conditions. centered medical homes. [EC
includes making information • Provide grants for improving health Committee amendment: Adopt
available on the web. system efficiency, including grants accountable care organization,
to establish community health bundled payment, and medical
• Require enhanced collection
teams to support a medical home home models on a large scale if
and reporting of data on race,
model; to implement medication pilot programs prove successful at
ethnicity, and primary language.
management services; to design reducing costs.]
Also require collection of access
and treatment data for people with and implement regional emergency
disabilities. care and trauma systems.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-18-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Improving quality/health • Require hospitals to report [EC Committee amendment:
system performance preventable readmission rates; Conduct accountable care
(continued) hospitals with high re-admission organization pilot programs in
rates will be required to work with Medicaid.]
local patient safety organizations • [EC Committee amendment:
to improve their rates. Establish the Center for
• Create a Patient Safety Research Medicare and Medicaid Payment
Center charged with identifying, Innovation Center to test
evaluating, and disseminating payment models that address
information on best practices for populations experiencing poor
improving health care quality. clinical outcomes or avoidable
• Create an inter-agency expenditures. Evaluate all models
Working Group to coordinate and expand those models that
and streamline federal quality improve quality without increasing
activities. spending or reduce spending
• Develop interoperable standards without reducing quality, or both.]
for using HIT to enroll individuals • [WM Committee amendment:
in public programs and provide Require the Institute of Medicine
grants to states and other to conduct a study on geographic
governmental entities to adopt variation in health care spending
and implement enrollment and recommend strategies for
technology. addressing this variation by
promoting high-value care.]
• Improve coordination of care
for dual eligibles by creating a
new office or program within
the Centers for Medicare and
Medicaid Services.
• Establish the Center for Quality
Improvement to identify, develop,
evaluate, disseminate, and
implement best practices in the
delivery of health care services.
Develop national priorities for
performance improvement and
quality measures for the delivery
of health care services.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 9](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-19-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Improving quality/health • Require disclosure of financial
system performance relationships between health
(continued) entities, including physicians,
hospitals, pharmacists, and other
providers, and manufacturers
and distributors of covered drugs,
devices, biologicals, and medical
supplies.
• Reduce racial and ethnic
disparities by conducting a study
on the feasibility of developing
Medicare payment systems for
language services, providing
Medicare demonstration grants
to reimburse culturally and
linguistically appropriate services
and developing standards for
the collection of data on race,
ethnicity, and primary language.
• [EC Committee amendment:
Conduct a national public
education campaign to raise
awareness about the importance
of planning for care near the end
of life.]
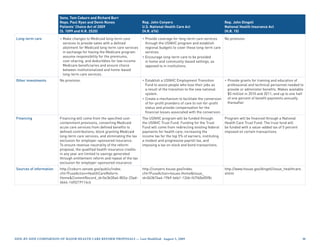
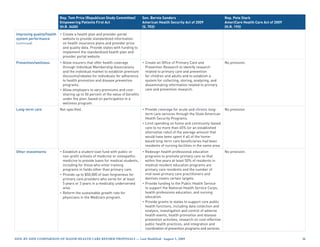
Prevention/wellness • Improve prevention by covering • Develop a national prevention and • Develop a national strategy to • The plan must invest in public
only proven preventive services health promotion strategy that improve the nation’s health health measures proven to reduce
in Medicare and Medicaid and sets specific goals for improving through evidenced-based cost drivers in our system, such as
providing incentives to Medicare health. Create a prevention and clinical and community-based obesity, sedentary lifestyles, and
and Medicaid beneficiaries to public health investment fund prevention and wellness smoking, as well as guarantee
complete behavior modification to expand and sustain funding activities. Create task forces access to proven preventive
programs. for prevention and public health on Clinical Preventive Services treatments. The American
• Promote prevention and wellness programs. and Community Preventive Recovery and Reinvestment Act
by providing grants to states to • Award competitive grants to Services to develop, update, and provides $1 billion for prevention
implement innovative approaches state and local governments and disseminate evidenced-based and wellness.
to promoting integration of health community-based organizations recommendations on the use of
care services to improve health to implement and evaluate clinical and community prevention
and wellness outcomes and proven community preventive services.
providing tax credits to small health activities to reduce chronic
businesses that implement proven disease rates and address health
wellness programs. disparities.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 20](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-20-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Prevention/wellness • Permit insurers to create • Improve prevention by covering
(continued) incentives for health promotion only proven preventive services in
and disease prevention practices. Medicare and Medicaid. Eliminate
• Encourage employers to provide any cost-sharing for preventive
wellness programs by conducting services in Medicare and increase
targeted educational campaigns Medicare payments for certain
to raise awareness of the value of preventive services to 100% of
these programs and by increasing actual charges or fee schedule
the allowable premium discount rates.
for employees who participate in
these programs from 20 percent
to 30 percent.
• Create a temporary Right Choices
Program to provide uninsured
adults with access to preventive
services.
Long-term care • Improve the availability of long- • Establish a national, voluntary • [EC Committee amendment: Not specified.
term care services by increasing insurance program for purchasing Establish a national, voluntary
access to home and community community living assistance insurance program for purchasing
based services through changes in services and supports (CLASS community living assistance
Medicaid program requirements program). The program will services and supports (CLASS
and through grants to states. provide individuals with functional program). The program will
limitations a cash benefit to provide individuals with functional
purchase non-medical services limitations a cash benefit to
and supports necessary to purchase non-medical services
maintain community residence. and supports necessary to
The program is financed through maintain community residence.
voluntary payroll deductions: The program is financed through
all working adults will be voluntary payroll deductions:
automatically enrolled in the all working adults will be
program, unless they choose to automatically enrolled in the
opt-out. program, unless they choose to
opt-out.]
• Improve transparency of
information about skilled nursing
facilities and nursing facilities.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 2](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-21-320.jpg)
![House Tri-Committee
America’s Affordable Health
Senate Finance Committee Senate HELP Committee Choices Act of 2009 President Obama
Policy Options Affordable Health Choices Act (H.R. 3200) Principles for Health Reform
Other investments [EC Committee amendment:
(continued) Support the development of
interdisciplinary mental and
behavioral health training
programs.] [EC Committee
amendment: Establish a
training program for oral health
professionals.]
• Provide grants to each state health
department to address core public
health infrastructure needs.
• Conduct a study of the feasibility of
adjusting the federal poverty level
to reflect variations in the cost of
living across different areas.
• [EL Committee amendment:
Grant waivers to requirements
related to the Employee
Retirement Income Security Act
of 1974 (ERISA) to states seeking
to establish a state single payer
system.]
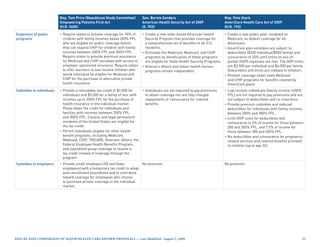
Financing Not specified. Considering a range The Congressional Budget Office The Congressional Budget President Obama dedicated $630
of options for achieving savings and estimates this proposal will cost Office estimates the net cost billion over ten years toward a
for generating new revenues. $615 billion over 10 years. Because of the proposal (less payments Health Reform Reserve Fund in his
the Senate HELP Committee does from employers and uninsured budget outline released in February
not have jurisdiction over the individuals) to be $1.042 trillion 2009 to partially offset the cost of
Medicare and Medicaid programs over ten years. Approximately half health reform.
nor revenue raising authority, of the cost of the plan is financed
mechanisms for financing the through savings from Medicare and
proposal will be developed in Medicaid, including incorporating
conjunction with the Senate Finance productivity improvements into
Committee. Medicare market basket updates,
reducing payments to Medicare
Advantage plans, changing drug
rebate provisions, reducing
potentially preventable hospital
readmissions, and cutting Medicaid
DSH payments.
Side-by-Side CompariSon of major HealtH Care reform propoSalS — last modified: august 5, 2009 2](https://image.slidesharecdn.com/healthreformsbsfull-124966720069-phpapp02/85/Healthreform-Sbs-Full-23-320.jpg)