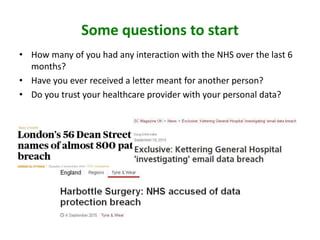
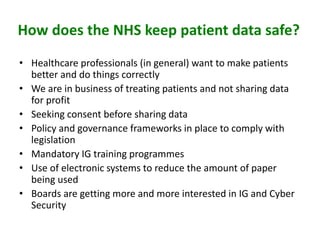
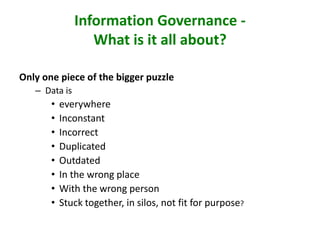
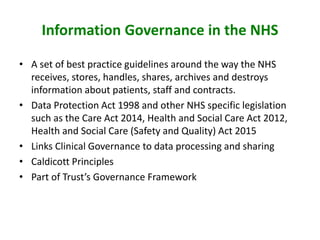
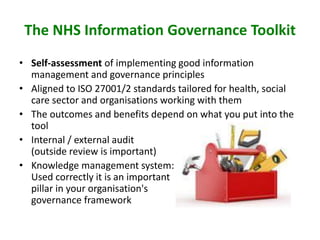
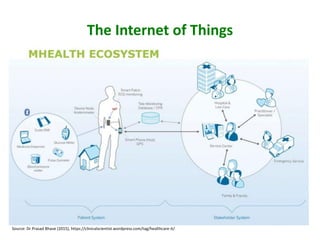
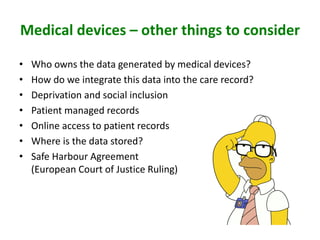
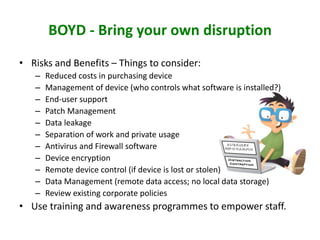
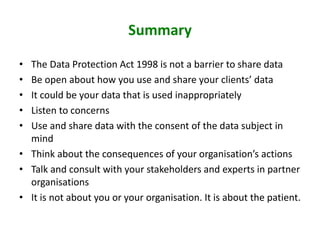
The document discusses data governance in the NHS, emphasizing the importance of protecting patient information while ensuring it is shared appropriately for effective care. Key points include the necessity of consent, adherence to legislation, and the principles of data governance that guide how patient data is managed. It also highlights the challenges posed by inaccurate data and the evolving landscape of healthcare data sharing, underscoring the need for flexibility and patient involvement in data handling practices.