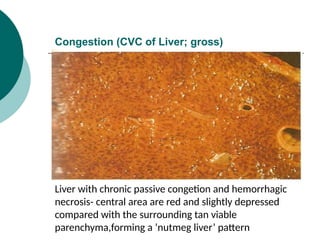
The document discusses haemodynamics and shock, detailing the importance of uninterrupted circulation for cell and organ health, and the pathophysiological classification of edema, hyperemia, and congestion. It explores the mechanisms of hemostasis, types of hemorrhage, causes of thrombosis, and defines shock along with its three categories: cardiogenic, hypovolemic, and septic shock. The document emphasizes the stages of shock and the underlying causes leading to different types of circulatory failures.