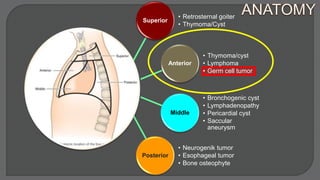
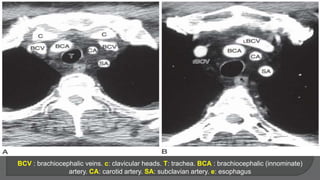
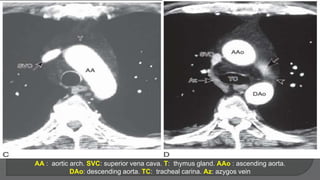
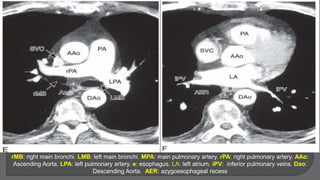
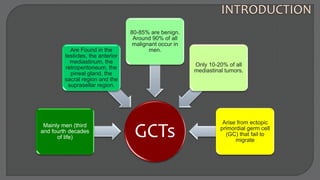
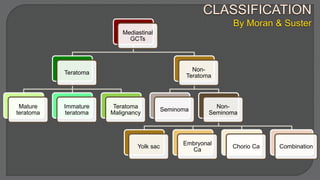
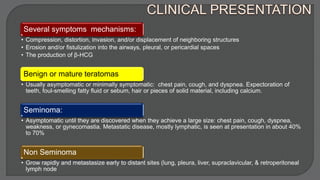
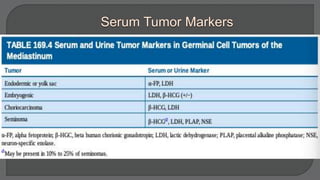
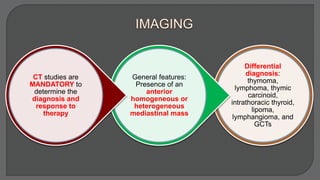
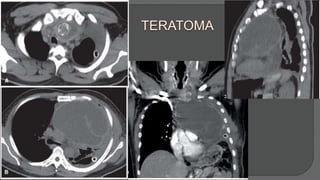
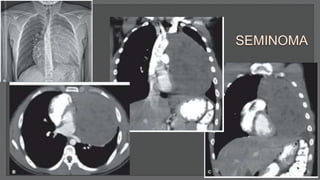
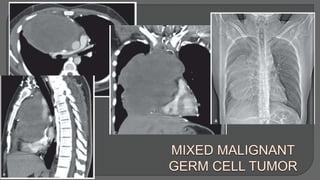
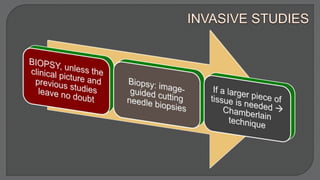
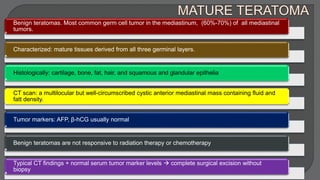
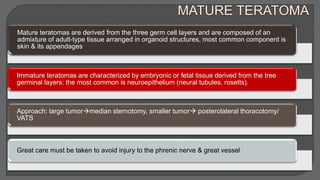
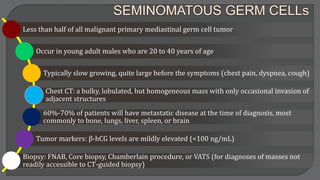
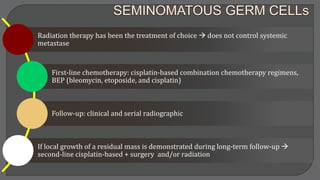
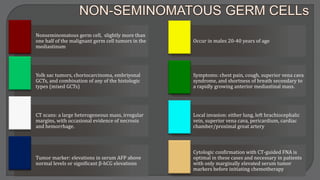
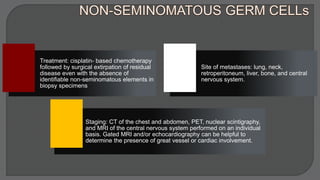
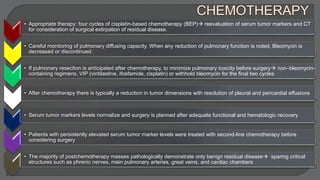
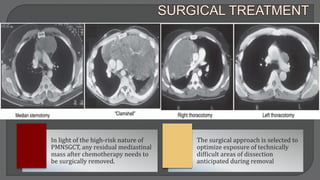
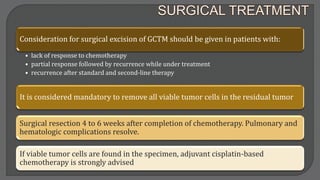
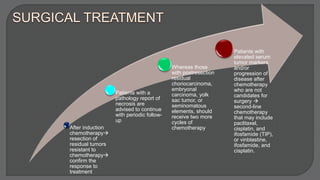
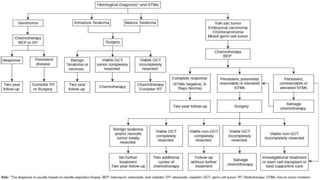
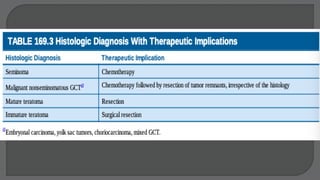
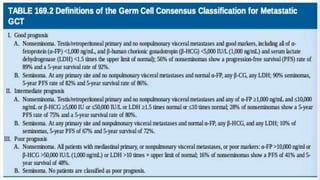
This document discusses mediastinal germ cell tumors (GCTs), including their anatomy, classification, pathologic features, diagnosis, and management. It notes that GCTs mainly affect young men and can be benign or malignant. Diagnosis involves imaging such as CT scans and tumor marker tests. Management depends on tumor type but commonly involves chemotherapy, surgery, and monitoring for recurrence. The document provides detailed information on diagnostic criteria and treatment approaches for specific GCT subtypes such as teratomas, seminomas, and non-seminomas.