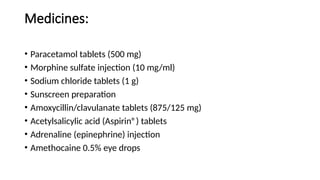
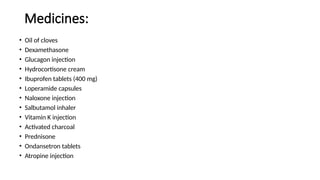
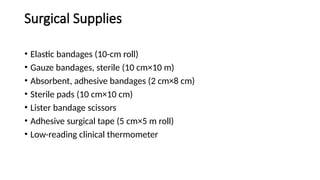
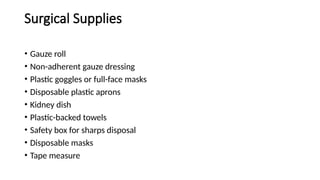
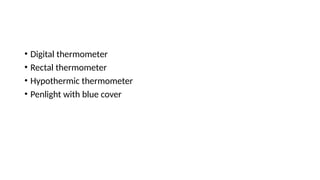
The document outlines the essential contents of first aid kits required by national regulations for ships, emphasizing that medical supplies must be adequate, well-maintained, and compliant with international maritime guidelines. It provides a comprehensive list of recommended medical supplies, including medicines, surgical supplies, and general medical equipment, which should be tailored based on voyage specifics and crew needs. Additionally, it highlights that vessels carrying dangerous goods must possess specific antidotes and equipment, with a reminder to consult national regulations for compliance and record-keeping.