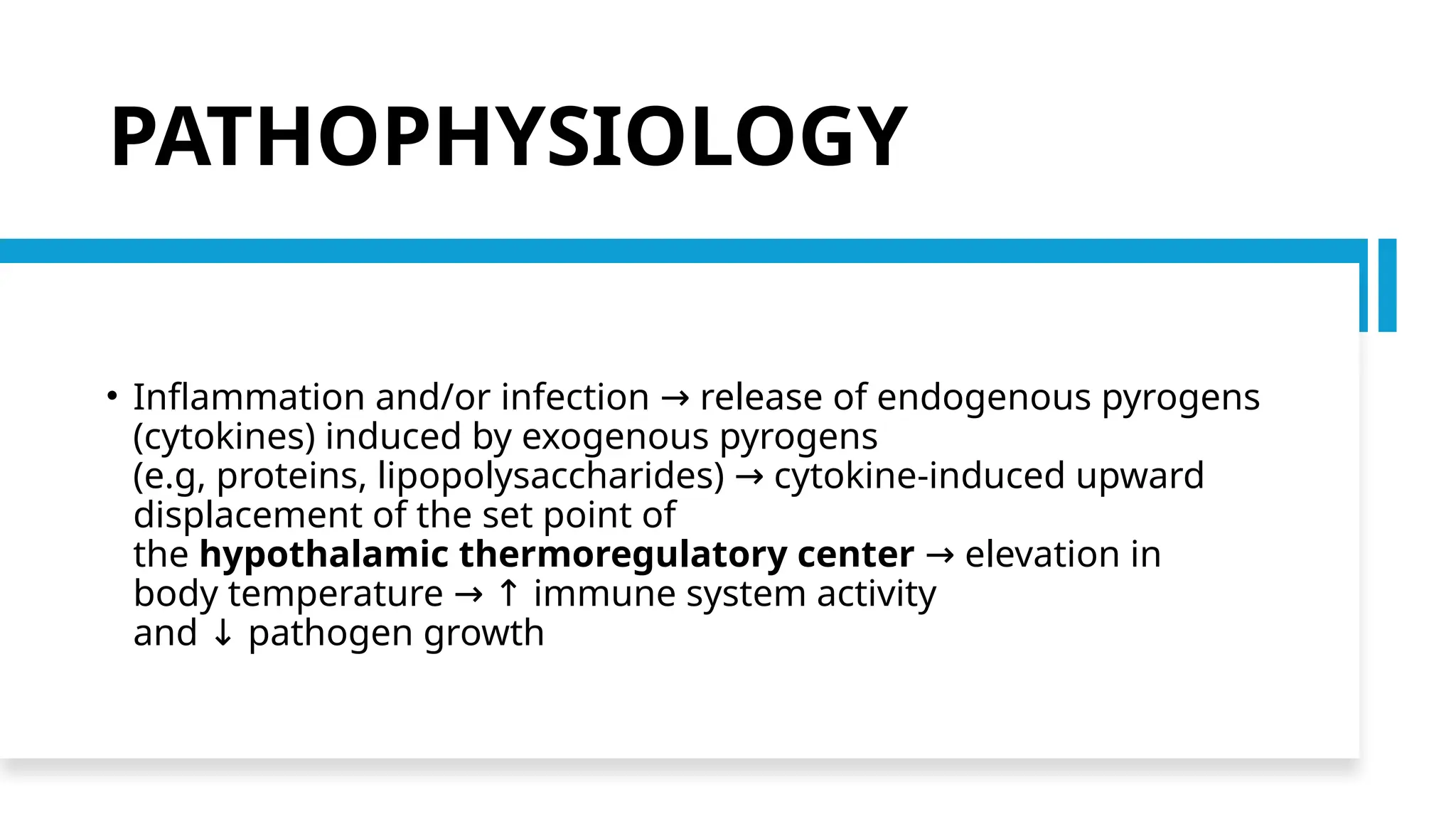
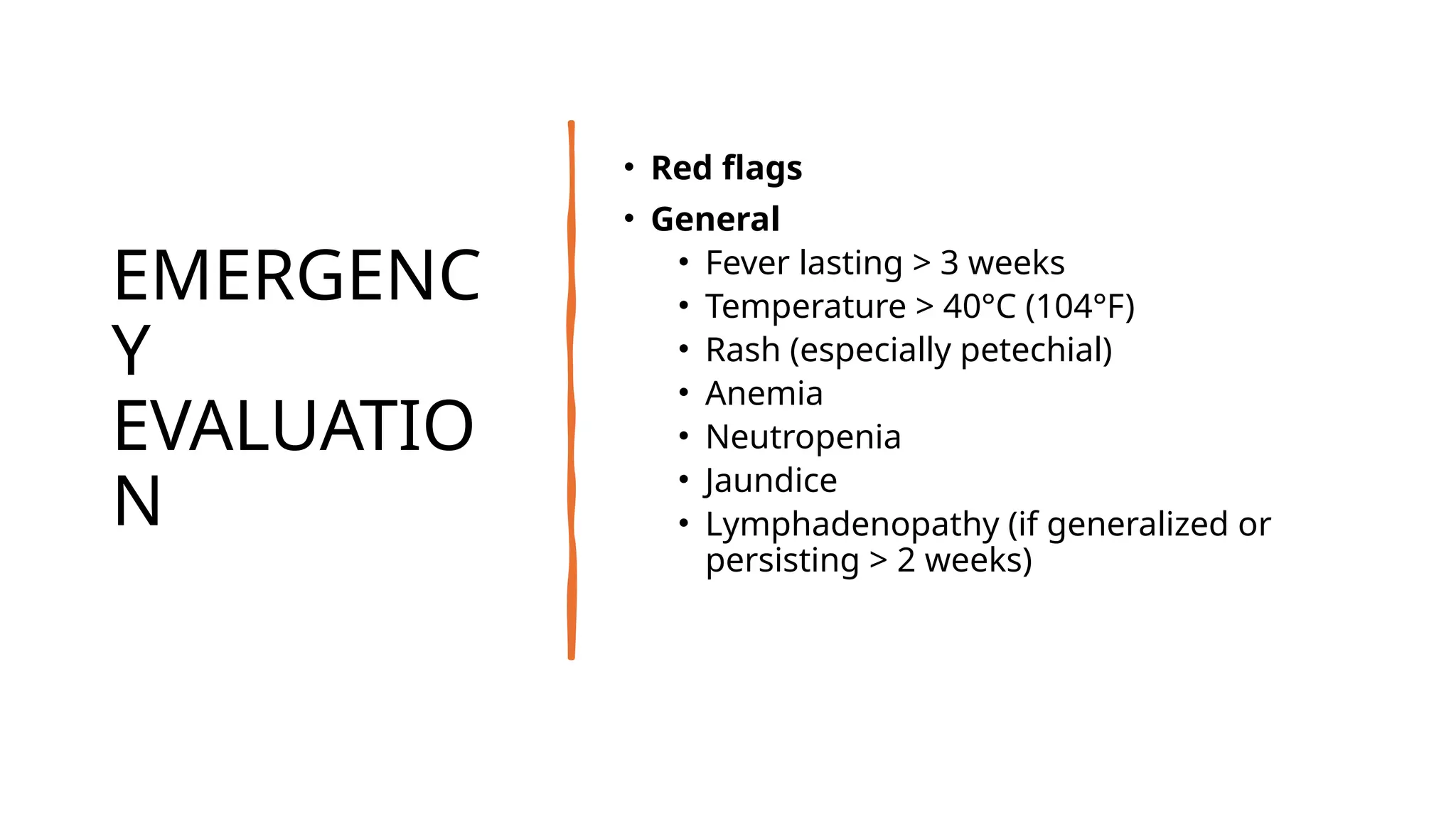
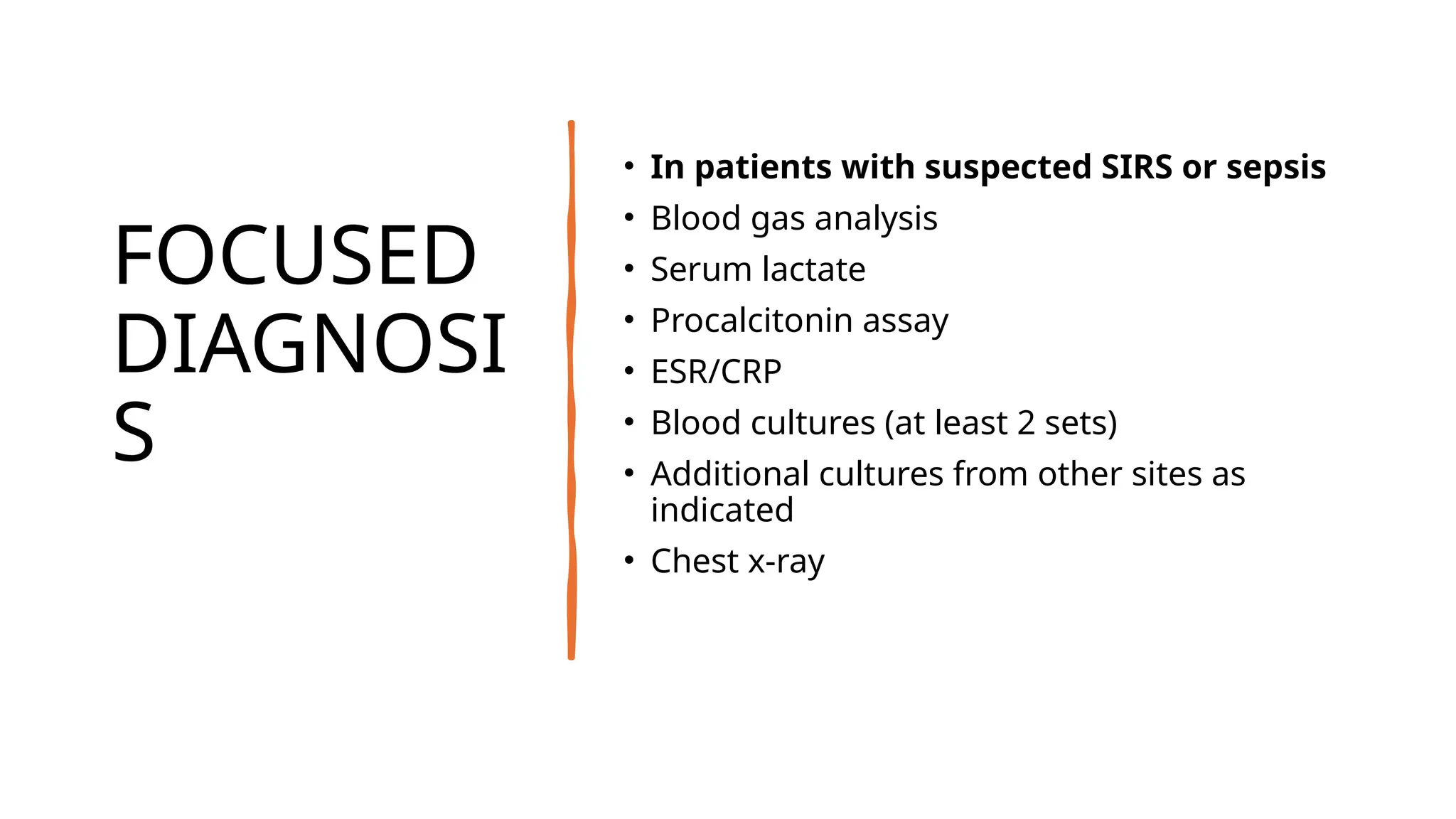
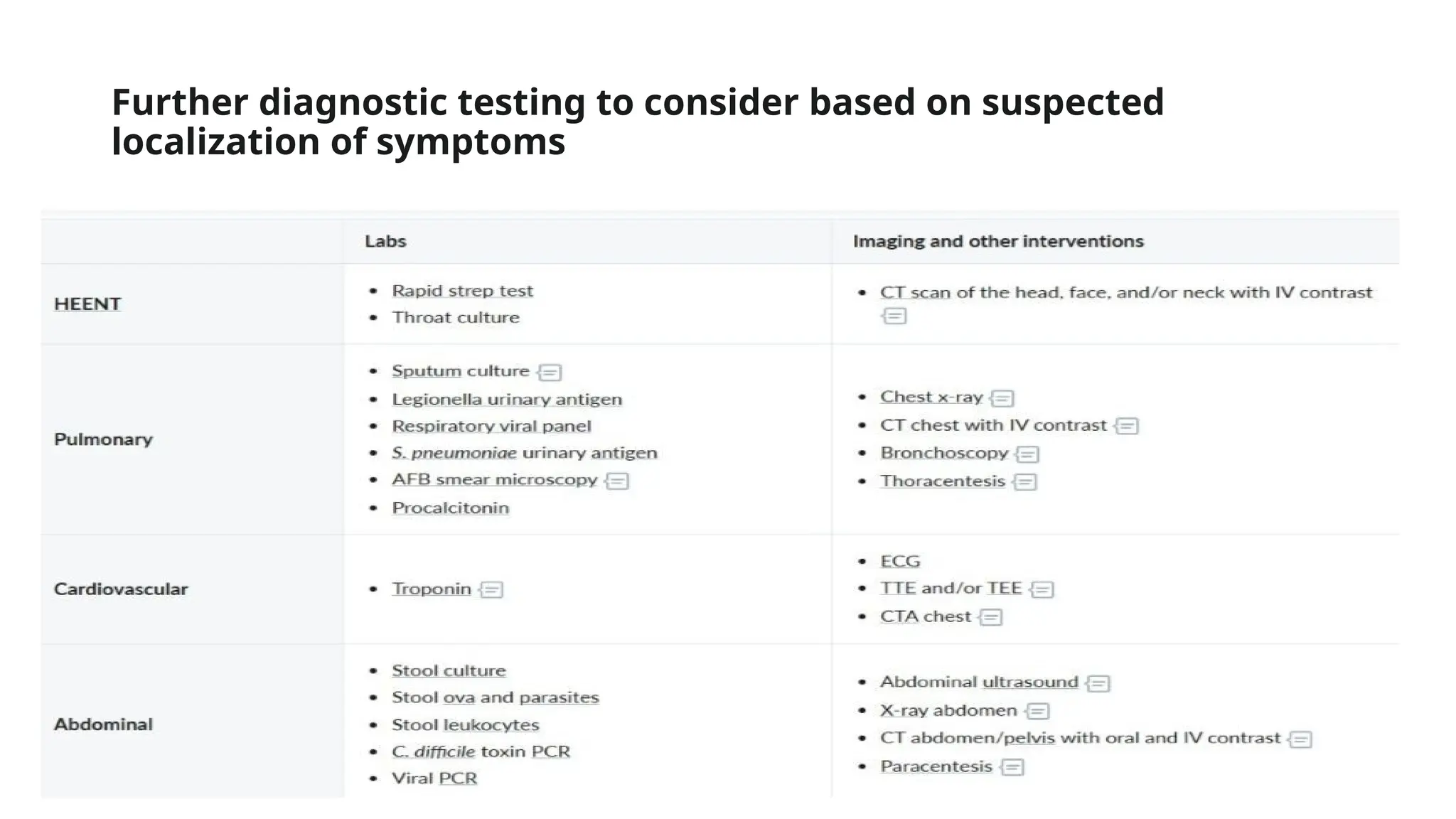
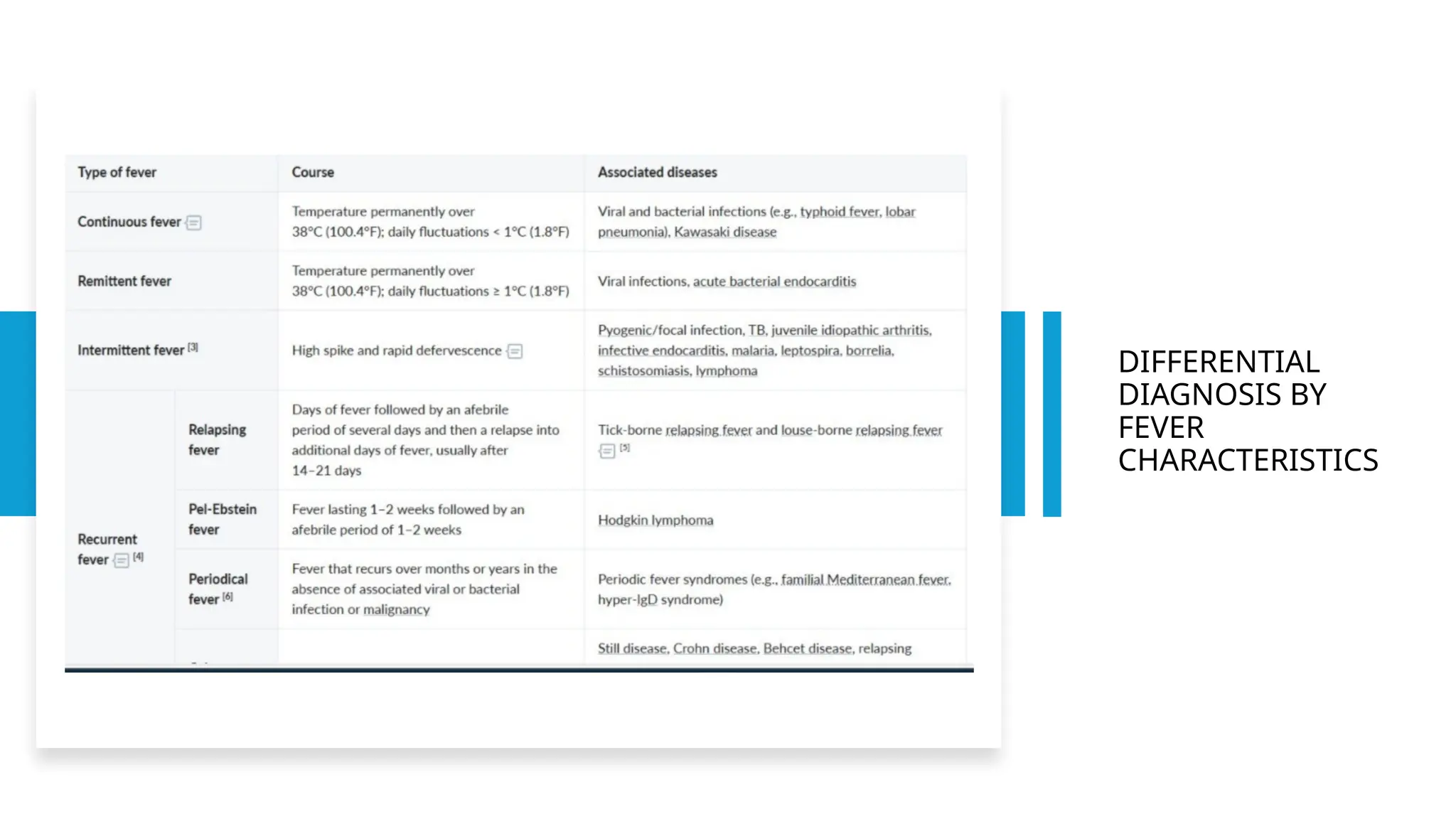
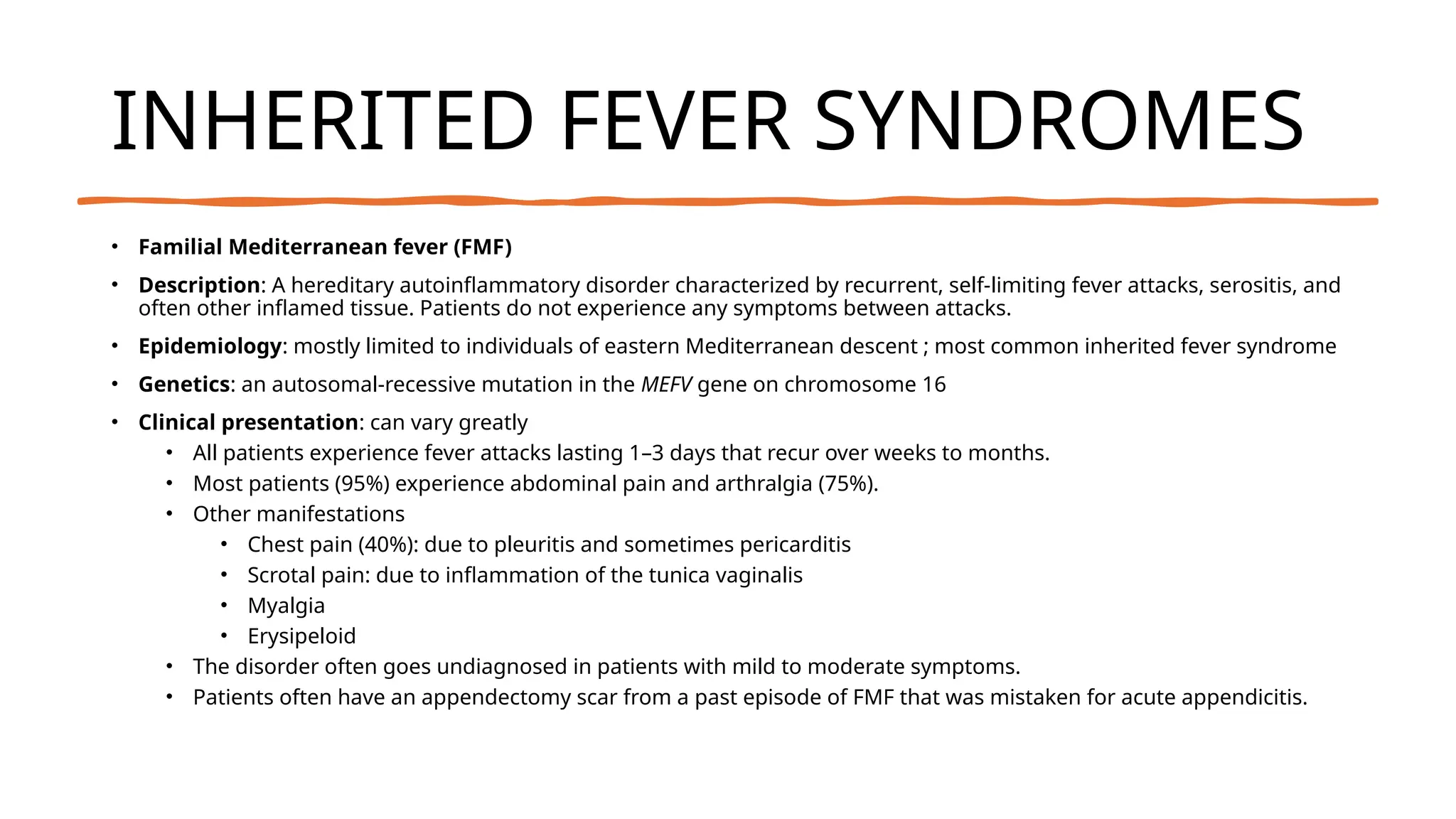
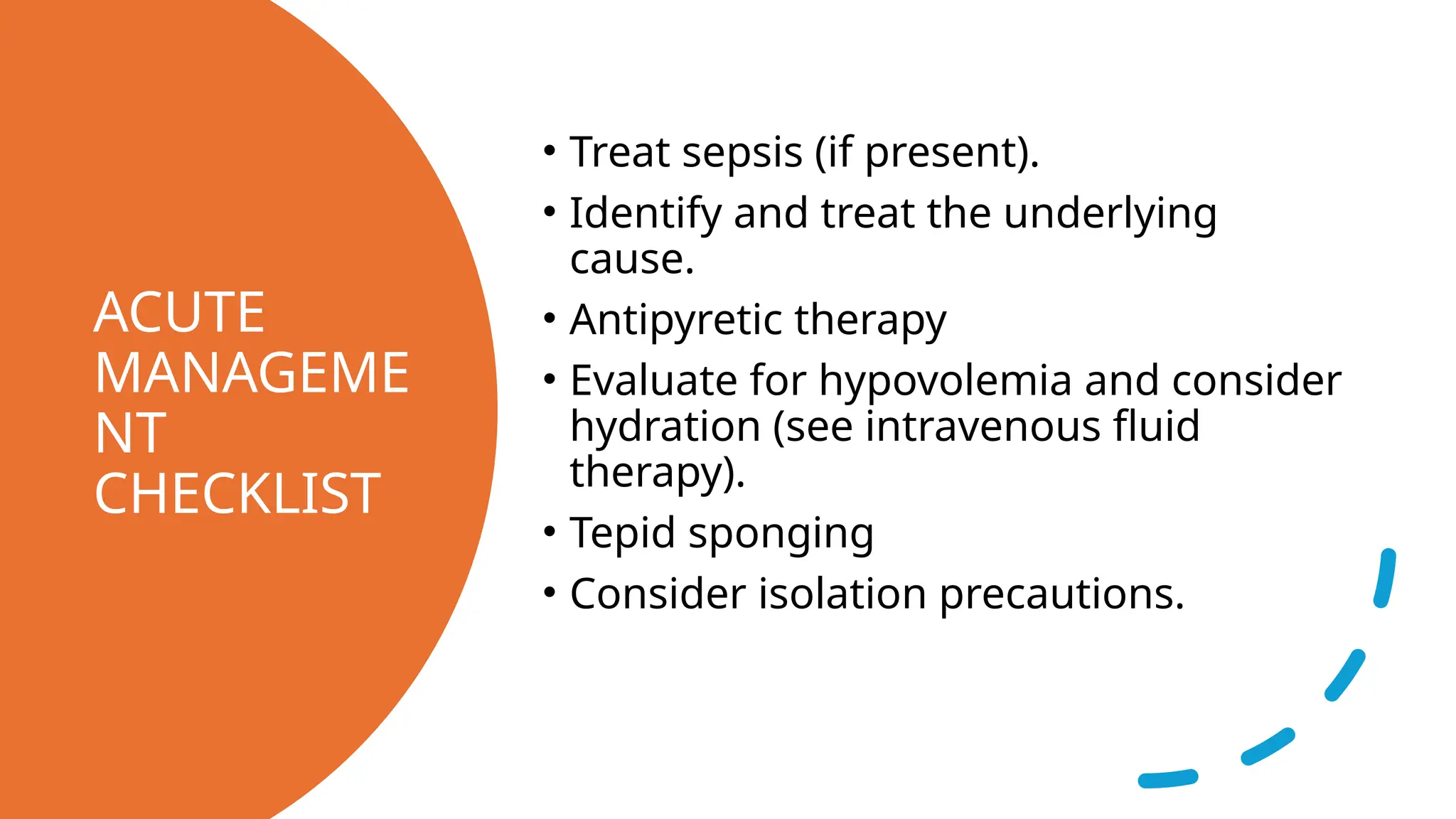
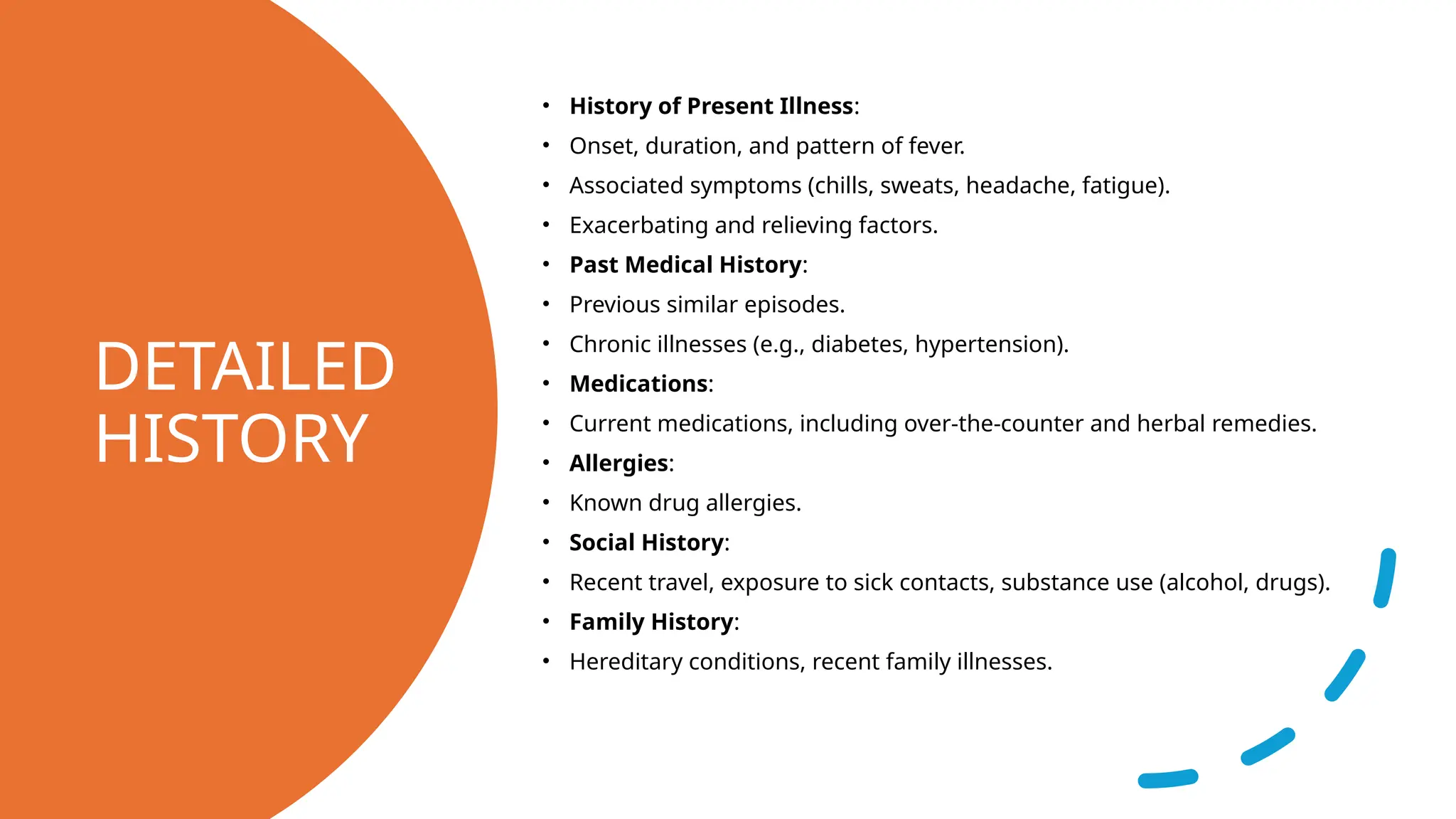
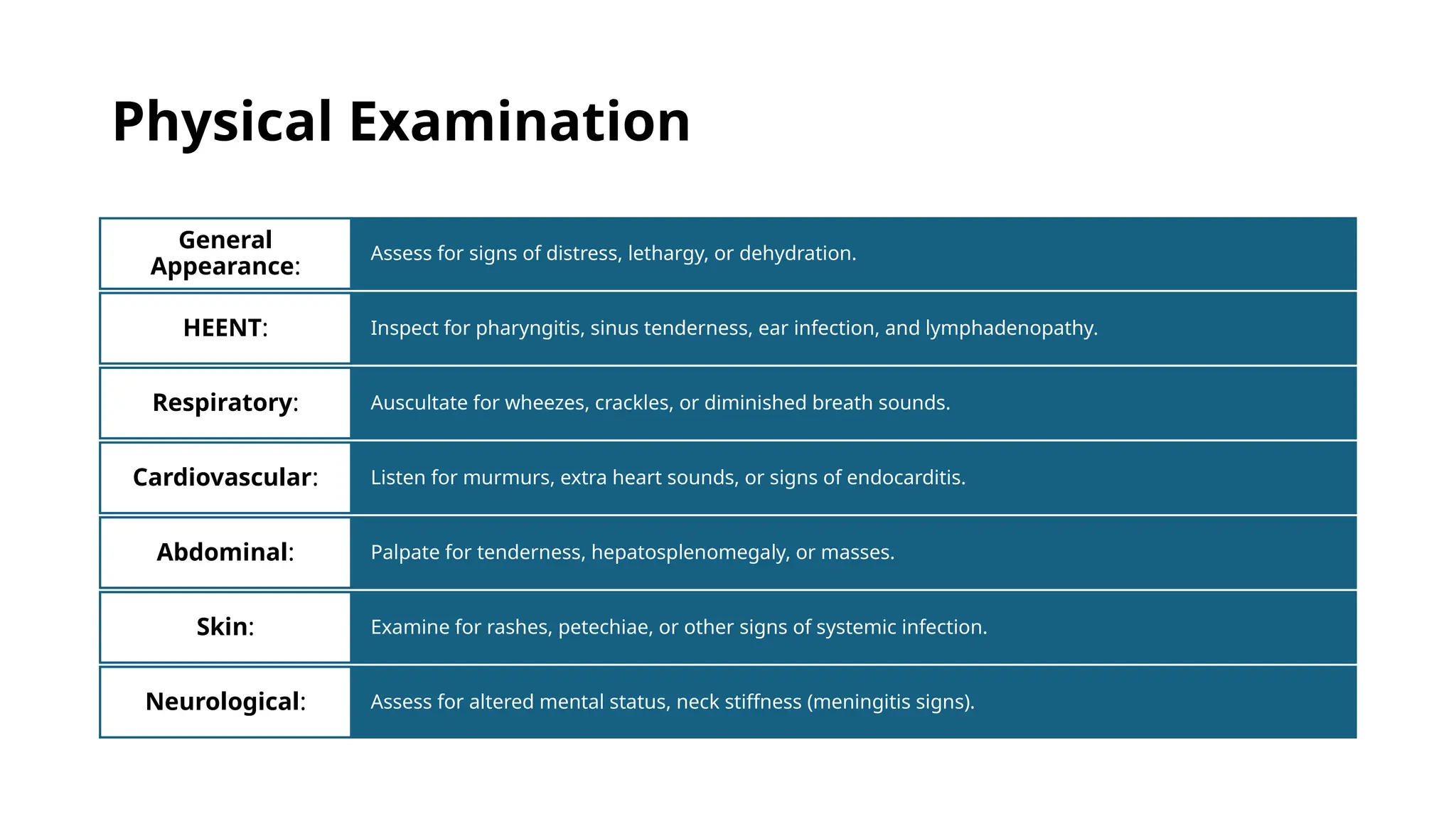
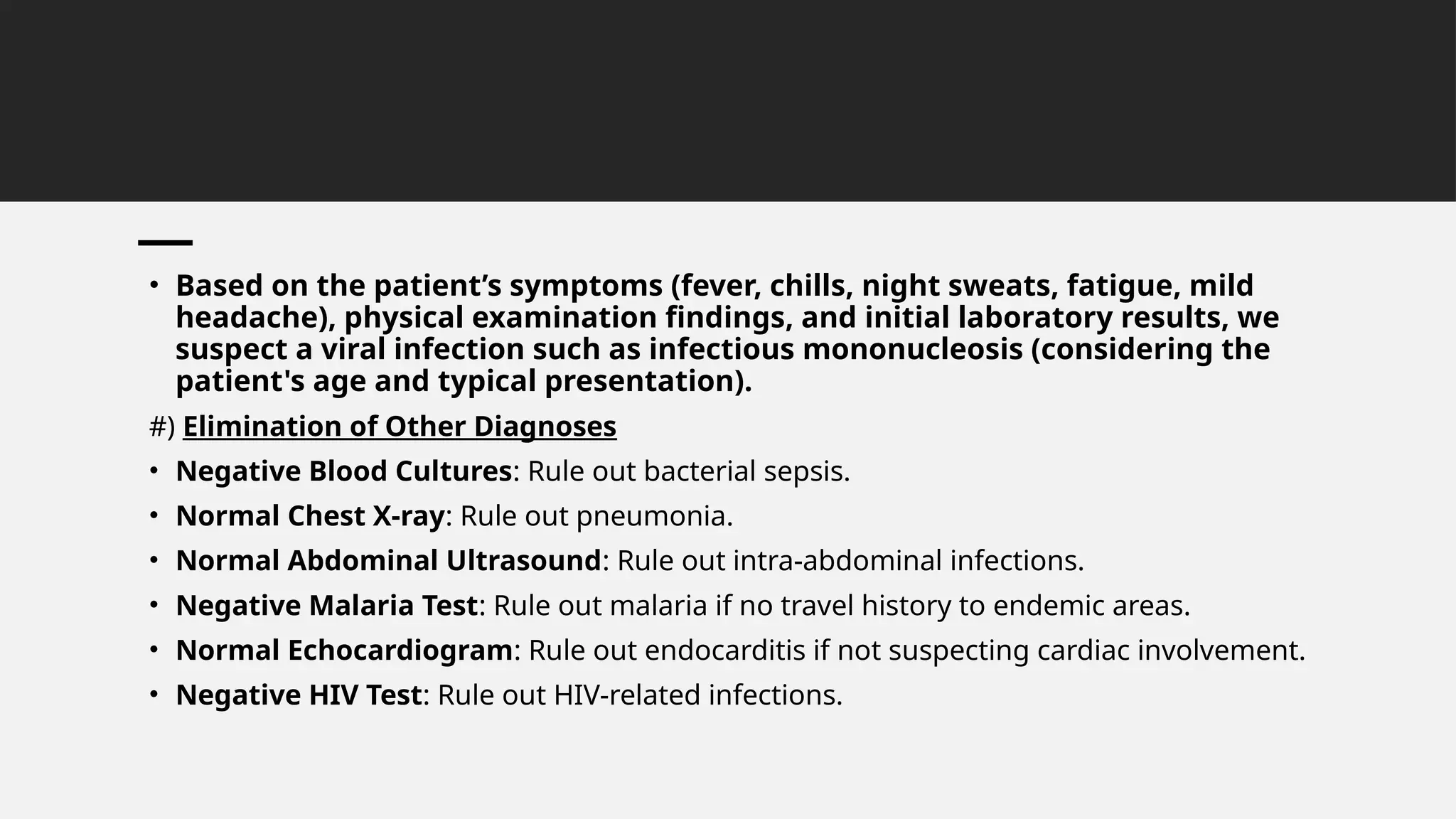
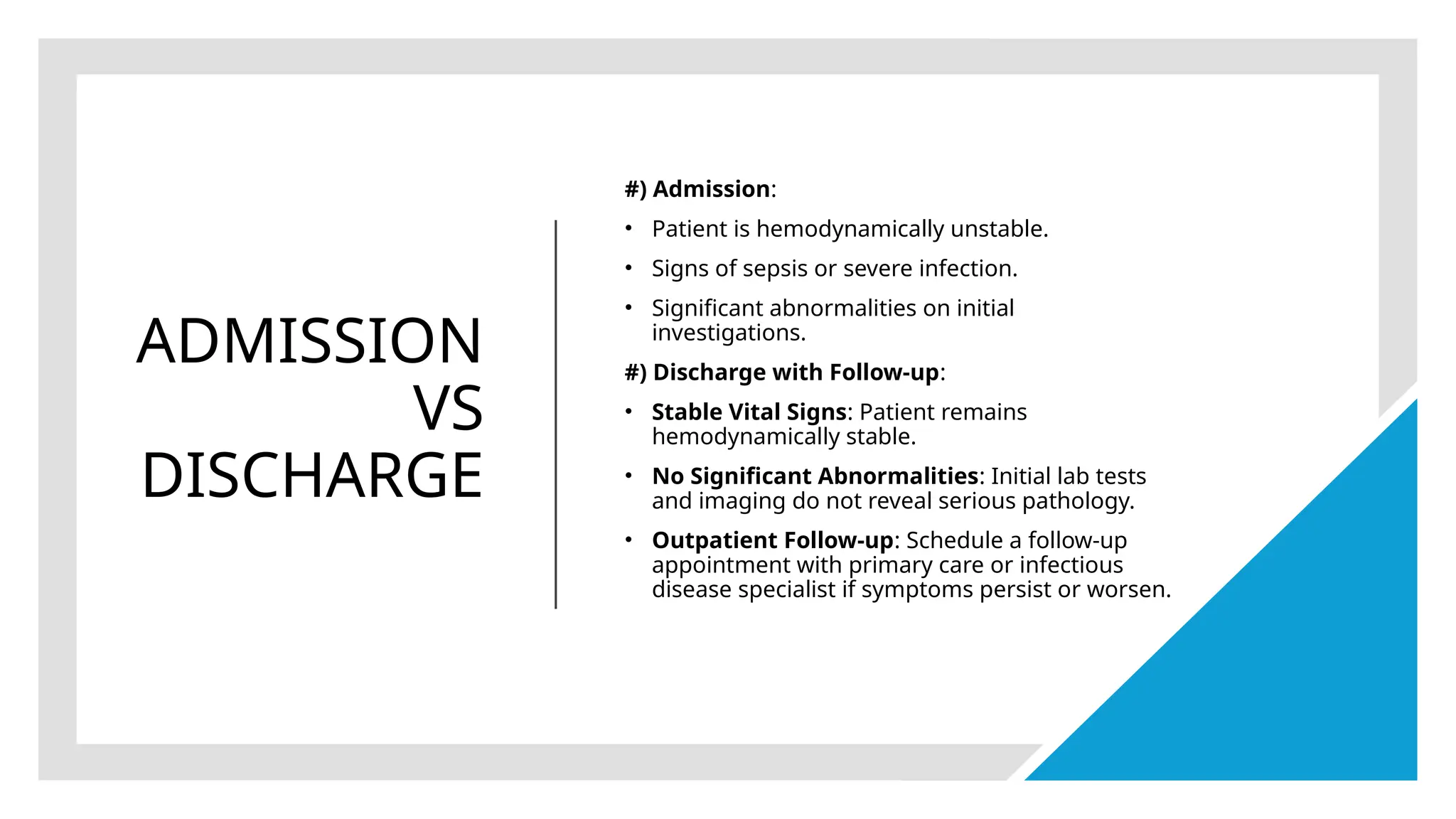
The document outlines the pathophysiology and emergency evaluation of fever, highlighting the causes, diagnostic approach, and treatment options. It emphasizes the need to identify and address underlying conditions, provide supportive care, and consider inherited fever syndromes like familial Mediterranean fever. A specific case study of a 22-year-old male with continuous fever is presented, detailing his assessment, management, and considerations for admission or discharge.