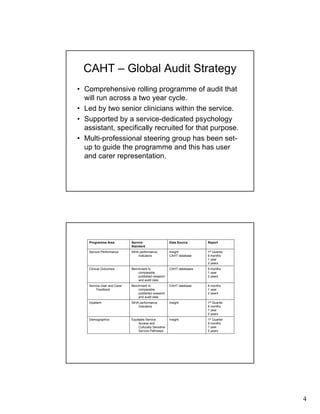
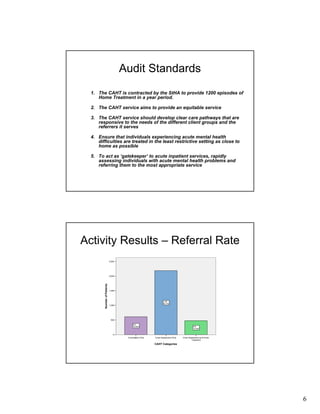
This document summarizes an audit of the Crisis Assessment and Home Treatment (CAHT) service in Sheffield, England. Some key findings include:
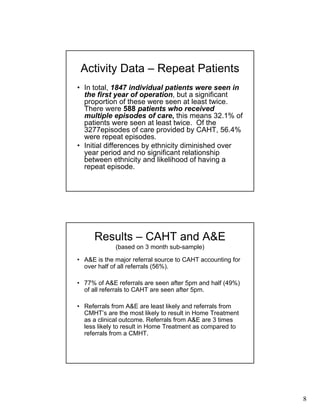
- CAHT provides 24/7 crisis assessment and home-based treatment as an alternative to hospitalization. The majority of referrals come from A&E departments.
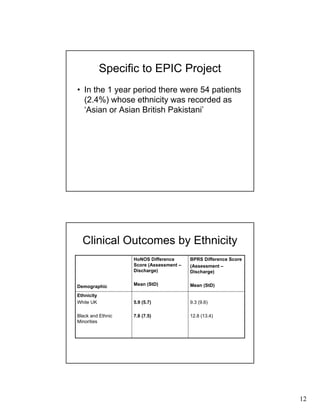
- Over half of episodes (56.4%) were for patients receiving repeated treatment. No significant differences were found in repeat episodes based on ethnicity.
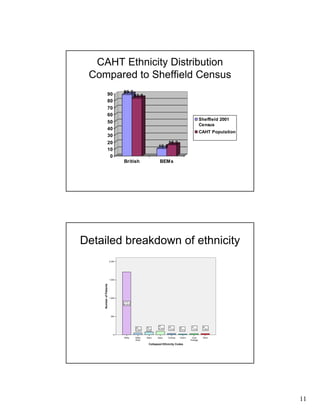
- The population served by CAHT has a higher proportion of individuals who are single, unemployed, and from Black and Ethnic Minority groups compared to Sheffield's general population.
- Significant differences were found in the ethnic distributions of patients across different