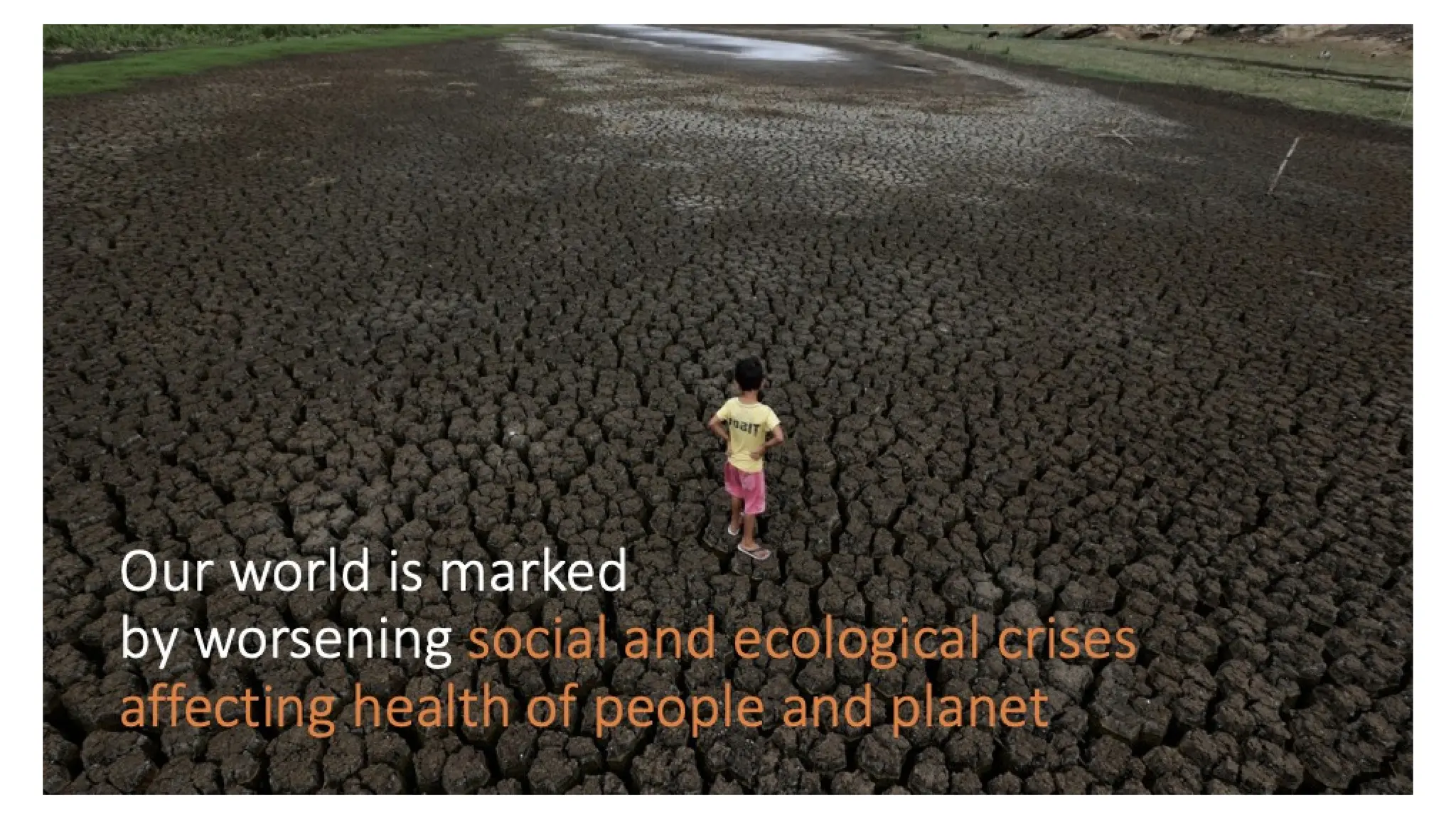
The document discusses the integration of environmental considerations within physiotherapy, emphasizing the interconnectedness of health, environment, and society. It advocates for a shift towards sustainable and low-carbon practices in healthcare, highlighting the importance of education and the role of health professionals in fostering ecological awareness. Additionally, it addresses social justice and equity in health, suggesting that health equity is tied to environmental justice and sustainability.