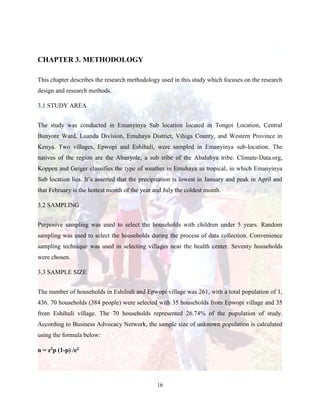
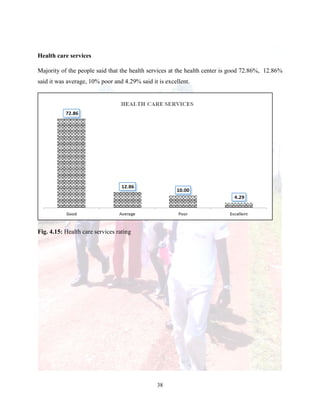
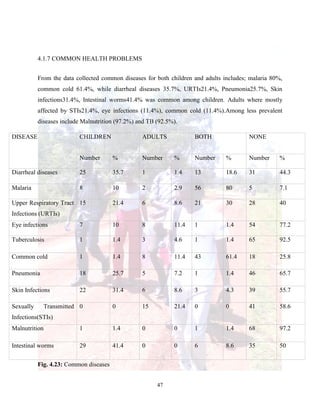
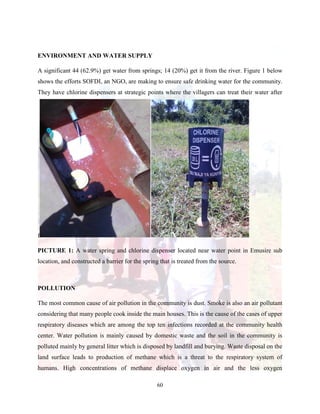
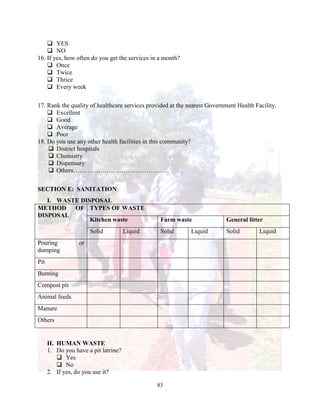
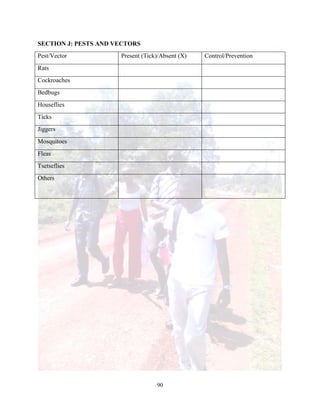
The document is a community health attachment report from Maseno University detailing a study conducted in Eshihuli and Epwopi villages in Kenya. It outlines the research methodology, community demographics, health-seeking behaviors, awareness of HIV/AIDS, nutrition practices, and common health problems observed during the data collection from September to October 2015. The findings suggest a need for greater education on health topics and improvements in community health services.