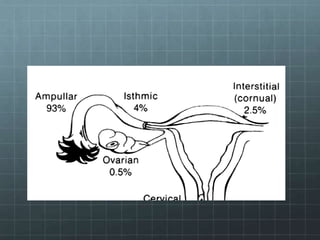
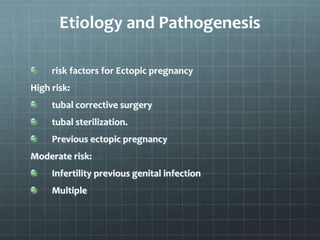
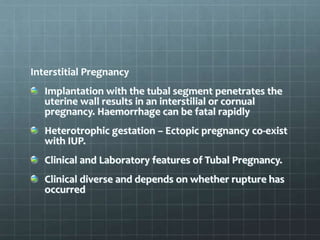
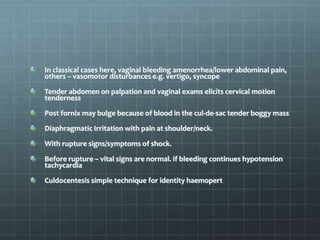
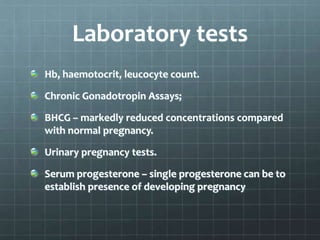
This document discusses ectopic pregnancy, which occurs when a fertilized egg implants and grows outside the uterus, most commonly in one of the fallopian tubes. It outlines the risk factors and causes, signs and symptoms, methods of diagnosis using ultrasound, lab tests, and laparoscopy/laparotomy. Treatment options discussed include surgical interventions like salpingostomy/salpingotomy or salpingectomy, as well as medical treatment with methotrexate. The aim of treatment is definitive management of an unruptured ectopic pregnancy to allow for improved reproductive outcomes.