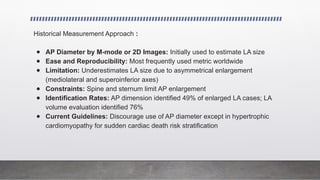
The document provides an extensive assessment of left atrial size and function, highlighting its critical roles in cardiac function and its predictive significance in various cardiovascular conditions. It discusses advanced imaging techniques for evaluating left atrial volume and emphasizes the importance of proper measurement methods, including the recent preference for three-dimensional echocardiography. The document also addresses the impact of various factors, such as age and body size, on left atrial volume, and outlines current guidelines for its evaluation and prognostic relevance.
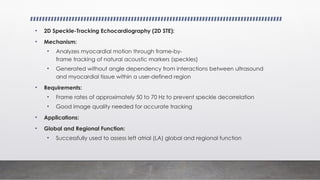
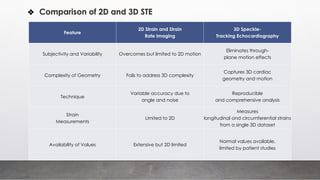
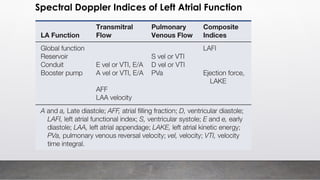
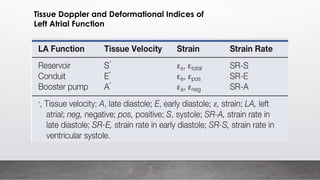
![⮚ Volumetric Indices for LA Function
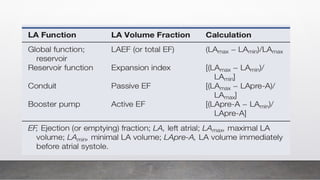
Index Description Function
Maximum Volume Volume at end-systole, just before mitral valve opening Represents reservoir capacity
Minimum Volume Volume at end-diastole, when mitral valve closes Represents emptied LA
Pre-Atrial
Systole Volume
Volume just before atrial systole, before ECG P wave Represents pre-atrial contraction
Expansion Index
Normalizes total LA emptying volume to minimum LA
volume
Related to reservoir function
LAFI (LA
Functional
Index)
Incorporates LAEF, LVOTvti, and LAVi(maximum LA
volume indexed to body surface area)
[LAFI = (LAEF × LVOTvti)/LAVi]
Comprehensive functional measure
Conduit Volume
Volume passing through LA not accounted by other
functions
Conduit volume = [LV stroke volume − (LAmax − LAmin)]
Requires simultaneous LV and LA volumes](https://image.slidesharecdn.com/leftatriumsizeandfunction-241116150019-890b74bd/85/ECHOCARDIOGRAPHY-left-atrium-size-and-function-pptx-42-320.jpg)
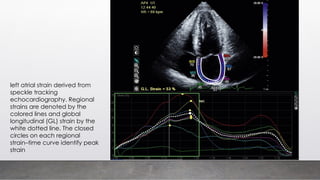
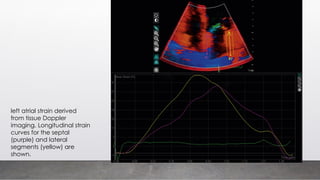
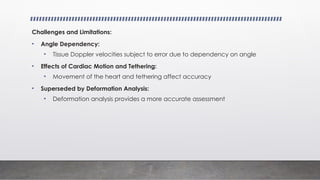
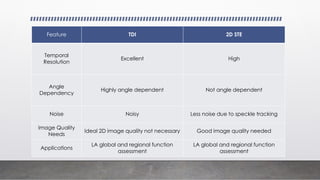
![⮚ Deformation Analysis (Strain and Strain Rate Imaging)
Strain and Strain Rates:
• Represent the magnitude and rate of myocardial deformation
• Assessed using either tissue Doppler velocities (TDI) or 2D echocardiographic
techniques (2D speckle-tracking echocardiography [2D STE])
Tissue Doppler Imaging (TDI):
• Advantages:
• Excellent temporal resolution
• Ideal 2D image quality not necessary
• Challenges:
• Highly angle dependent
• Noisy, which can impact accuracy](https://image.slidesharecdn.com/leftatriumsizeandfunction-241116150019-890b74bd/85/ECHOCARDIOGRAPHY-left-atrium-size-and-function-pptx-52-320.jpg)