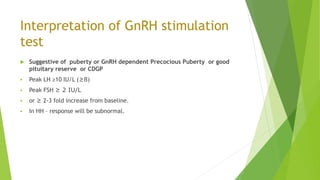
The document discusses various dynamic tests used in endocrinology, detailing their purposes, protocols, and interpretations. Key tests include the Insulin Tolerance Test, ACTH Stimulation Test, Growth Hormone Provocative Test, Water Deprivation Test, and others aimed at diagnosing endocrine dysfunction. Emphasis is placed on the importance of methodical execution, accuracy in hormonal assays, and careful interpretation of results.