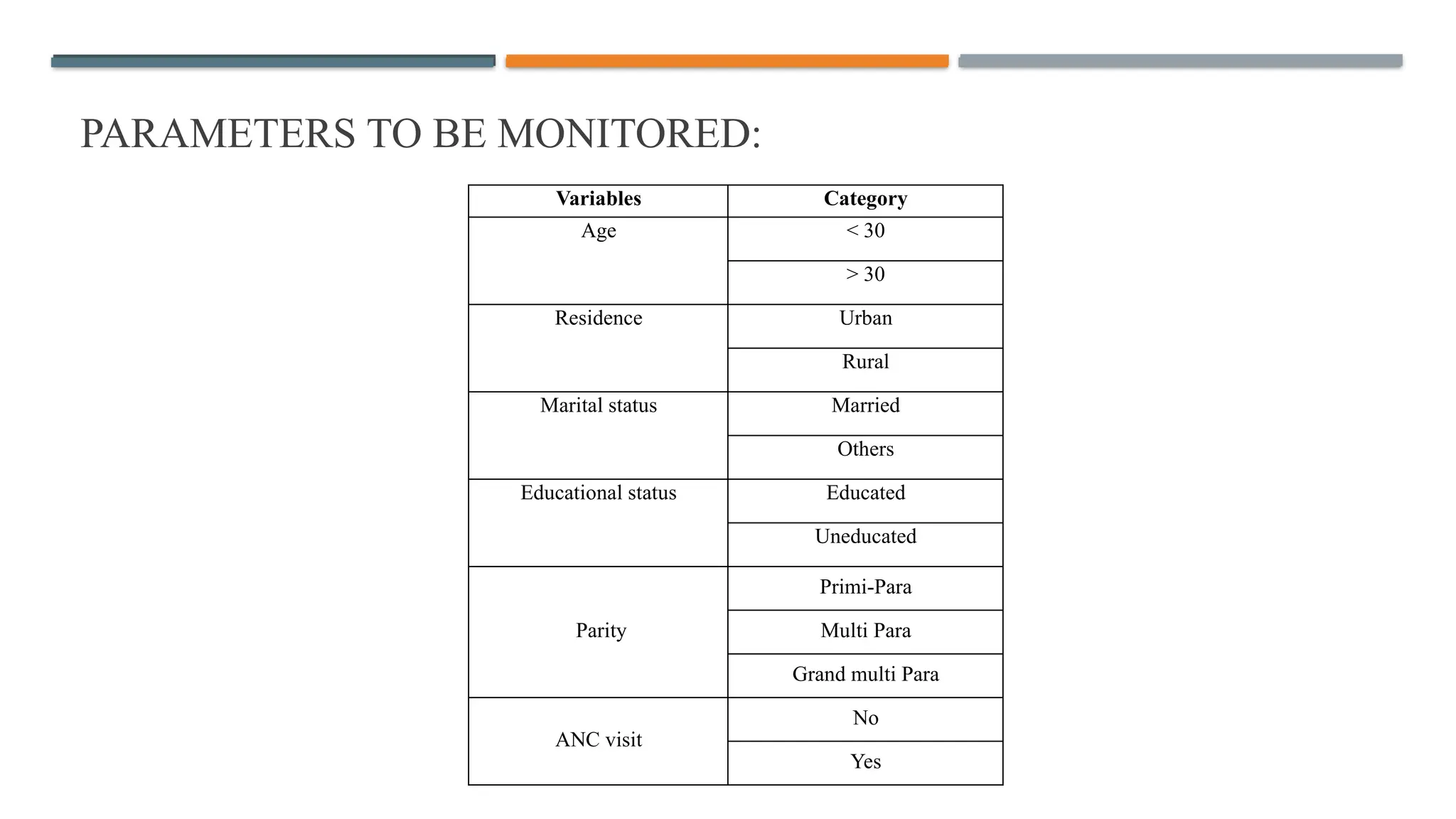
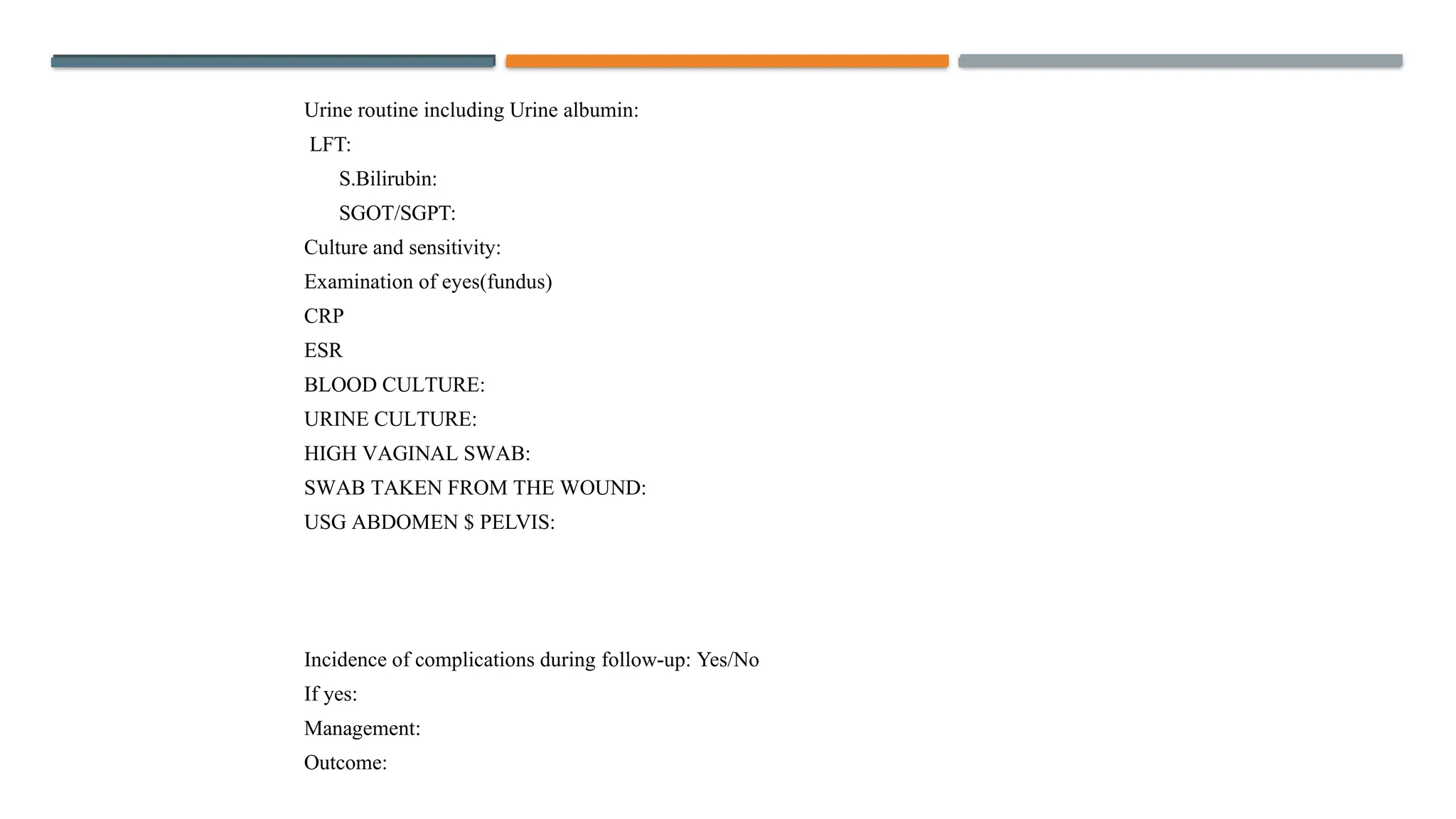
This study investigates the incidence of post-cesarean surgical site infections (SSIs), their associated risk factors, and effective management strategies. The primary objective is to assess the incidence rate, while secondary objectives include identifying risk factors and evaluating preventive measures. Results indicate that SSIs can significantly impact maternal health, with a focus on early diagnosis and adherence to best practices to reduce complications.