1) A stroke occurs when blood flow to the brain is interrupted, depriving brain tissue of oxygen and nutrients. It is a medical emergency.
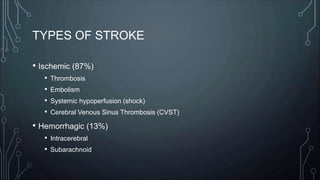
2) Risk factors for stroke include hypertension, diabetes, smoking, obesity, heart disease, and atrial fibrillation. Common symptoms include weakness, numbness, difficulty speaking, and vision changes.
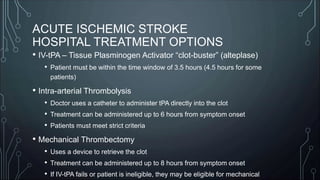
3) Stroke centers are designated as acute stroke ready, primary, or comprehensive depending on available resources and capabilities for stroke treatment. Early recognition and rapid transport to the appropriate facility improves outcomes.


























![SOURCES
• American Stroke Association (www.strokeassociation.org)
• MIEMSS 2019 Maryland Medical Protocols (www.miemss.org)
• Western Maryland Health System Stroke Center (www.wmhs.com)
• The Joint Commission [formerly JCAHO] (www.jointcommission.org)
• Wikipedia (www.wikipedia.org)](https://image.slidesharecdn.com/dm1912-230412090319-bba1c4c7/85/DM_1912-ppt-31-320.jpg)