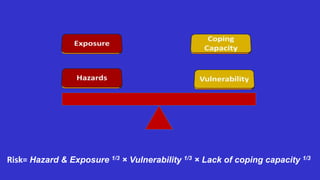
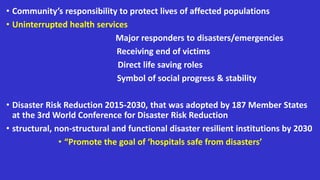
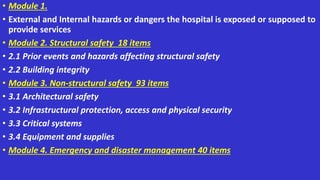
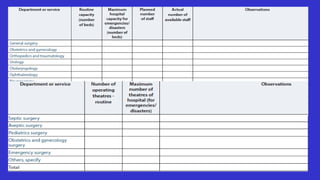
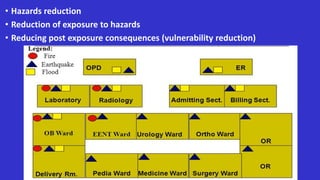
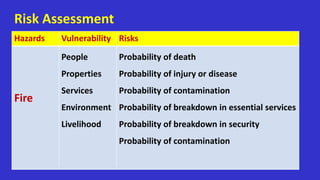
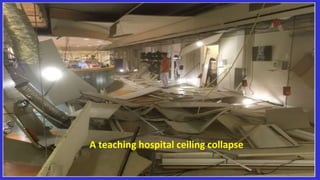
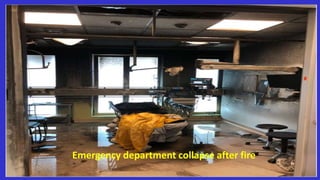
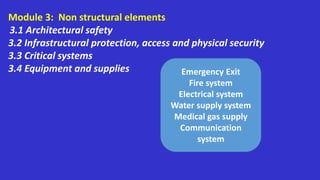
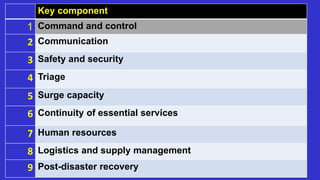
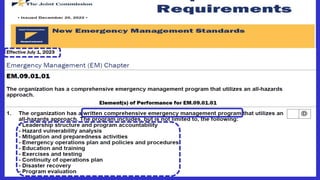
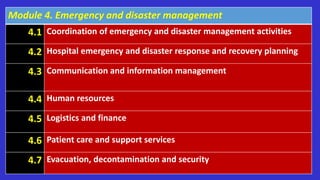
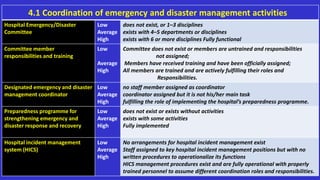
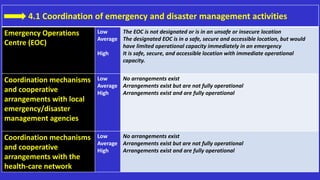
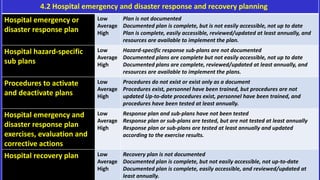
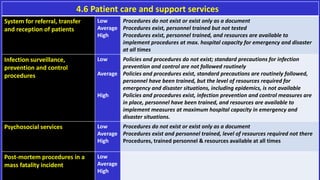
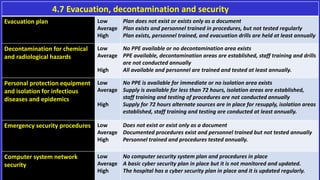
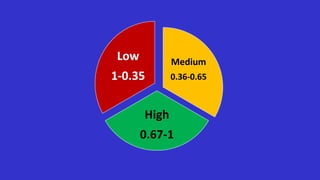
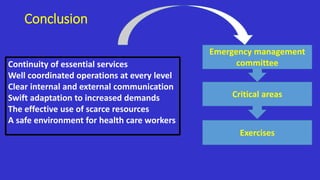
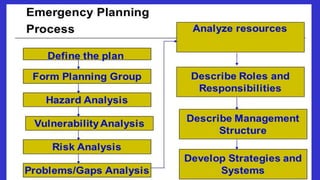
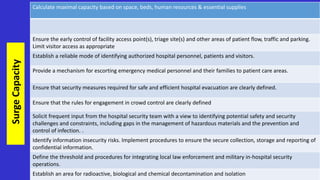
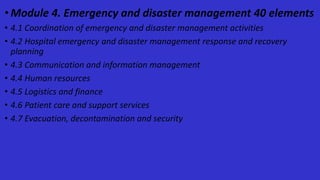
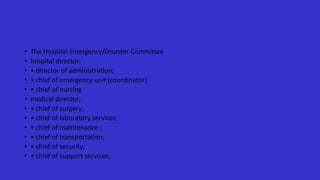
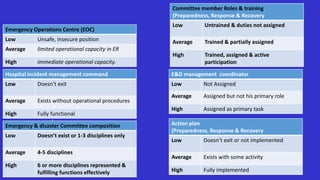
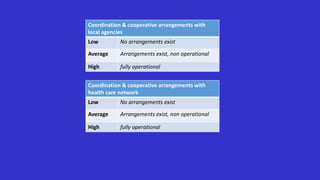
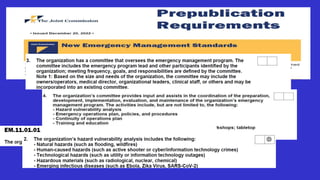
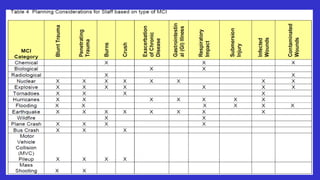
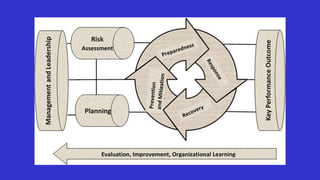
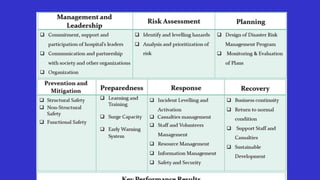
This document provides information on disaster preparedness for hospitals. It discusses key concepts like disasters, risks, major responders, and outlines a framework for hospital preparedness including structural safety, non-structural safety, emergency management, and hospital safety index. The framework includes 4 modules that assess hazards, building integrity, emergency planning, and more. It emphasizes the importance of preparedness, reducing risks and vulnerabilities, and maintaining essential health services during disasters.