This document provides guidelines on hospital safety from disasters in India. It aims to ensure that hospitals are structurally sound and able to continue functioning during and after disasters by being prepared. The guidelines apply to all government and private hospitals in India. Key objectives include taking a multi-hazard approach to hospital safety and ensuring structural safety, staff preparedness, and that each hospital has a disaster management plan. The guidelines cover awareness generation, hospital preparedness and response, structural and fire safety design, maintenance, licensing/accreditation, and a national action framework. The overall vision is for all Indian hospitals to be safer with minimized risks to life and infrastructure during disasters.








































![Design and Safety of Hospital Buildings
33
Hospital Safety
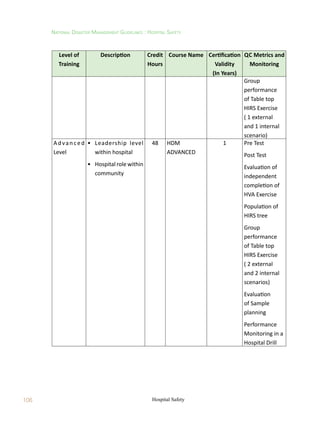
Table 5.2: Applicable Standards for ensuring Safety of Non-Structural Elements (NSEs) of
buildings
S.No. Standard or Guideline Comment
1 Design of NSEs of New
Hospitals
This Guideline addresses additional DESIGN
requirements (over and above those prescribed by
relevant national standards), but does NOT provide
specifications for DETAILING of connections between
structural and non-structural members.
Detailedclausesandcommentariesneedtobedeveloped
on design and detailing of connection between SEs and
NSEs.
2 Pre-Disaster Safety
Assessment of NSEs
Currently, no formal standard is available.
Detailed documents need to be developed, which shall
comply with the requirements laid down in this Chapter
also.
3 Design of Retrofit of Non-
Structural Systems and
Elements in Hospitals
This Guideline addresses the additional
requirements.
Detailed documents need to be developed, which shall
comply with the requirements laid down in this Chapter
also.
4 Post-Disaster Damage
Assessment of NSEs
Currently, no standard is available.
Detailed documents need to be developed, which shall
comply with the requirements laid down in this Chapter
also.
Note: Basic guidance on these four aspects is available in some national and international
documents [e.g., ‘Reducing Earthquake Risk in Hospitals from Equipment, Contents,
Architectural Elements and Building Utility Systems.’ Geo-Hazards International. 2009].
5.2 Expected Performance Of Hospitals
Building Units of a Hospital Campus shall be classified under two groups, namely,
a. Critical Units of Hospital Buildings – Buildings and Structures (and therefore SEs and
NSEs) that provide medical services essential in the immediate aftermath of disasters ;
and](https://image.slidesharecdn.com/hospitalsafety-220628060654-a6b2b215/85/Hospital-Safety-pdf-47-320.jpg)












![Design and Safety of Hospital Buildings
49
Hospital Safety
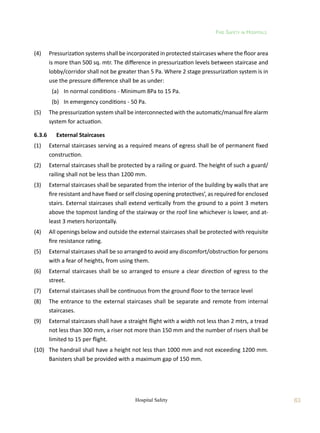
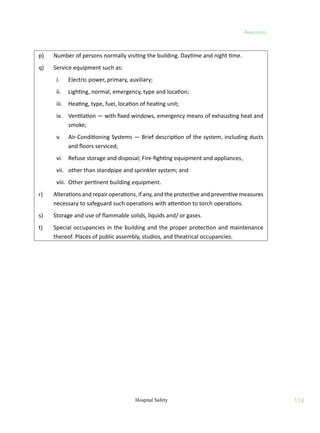
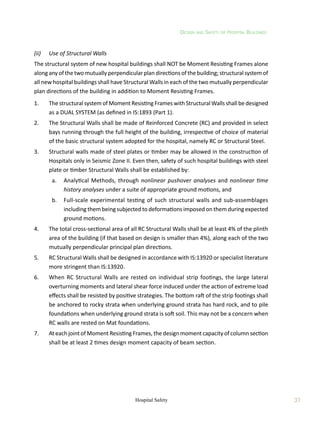
5.5.4 Design Guidelines – Acceleration-Sensitive NSEs
The design lateral force Fp
for the design of acceleration-sensitive NSEs may be taken as:
p
p
p
p
p W
I
R
a
h
x
1
Z
F
where Z is the Seismic Zone Factor (as defined in IS:1893 (Part 1)), Ip
the Importance Factor
of the NSE (Table 3.5), Rp
the Component Response Modification Factor (Table 3.6), ap
the
Component Amplification Factor (Table 5.6), Wp
the Weight of the NSE, x the height of point
of attachment of the NSE above top of the foundation of the building, and h the overall height
of the building.
Table 5.5: Proposed Importance Factors Ip
of NSEs
NSE Ip
Component containing hazardous contents 2.5
Life safety component required to function after an earthquake (e.g., fire
protection sprinklers system)
2.5
Storage racks in structures open to the public 2.5
All other components 2.0
Table5.6:Coefficientsap
andRp
ofArchitectural,MechanicalandElectricalNSEs[FEMA369,2001]
S. No. Item ap
Rp
1 Architectural Component or Element
Interior Non-structural Walls and Partitions
Plain (unreinforced) masonry walls 1.0 1.5
All other walls and partitions 1.0 2.5
Cantilever Elements (Unbraced or braced to structural frame below its
center of mass)
Parapets and cantilever interior non-structural walls 2.5 2.5
Chimneys and stacks where laterally supported by structures. 2.5 2.5
Cantilever elements (Braced to structural frame above its center of
mass)
Parapets 1.0 2.5
Chimneys and stacks 1.0 2.5
Exterior Non-structural Walls 1.0 2.5
Exterior Non-structural Wall Elements and Connections
Wall Element 1.0 2.5
Body of wall panel connection 1.0 2.5
Fasteners of the connecting system 1.25 1.0](https://image.slidesharecdn.com/hospitalsafety-220628060654-a6b2b215/85/Hospital-Safety-pdf-63-320.jpg)