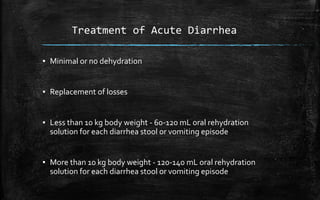
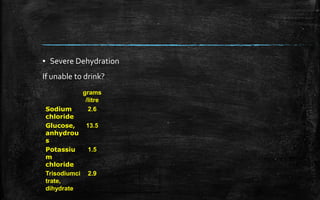
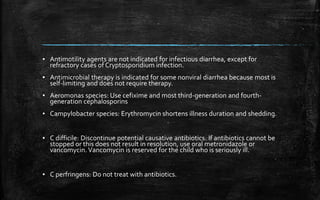
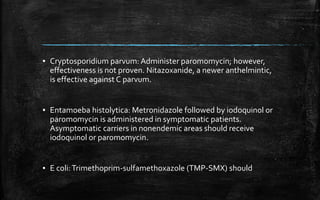
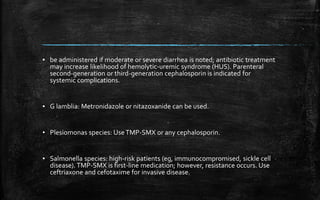
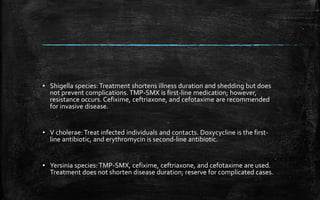
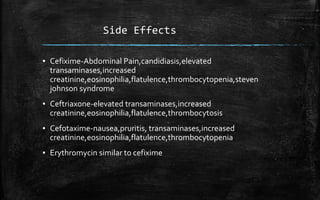
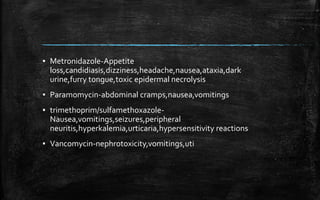
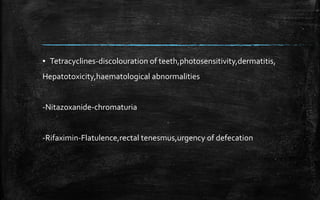
This document discusses diarrhea, including its definition, types, causes, clinical presentation, treatment, and side effects of treatments. It defines diarrhea as a reversal of normal water and electrolyte absorption to secretion, resulting in loose stools. There are two types: acute lasting less than 14 days and chronic lasting more than 14 days. Causes include various pathogens like rotavirus or bacteria. Treatment depends on severity of dehydration and involves oral rehydration. Antimicrobial therapy may be used for infectious causes like Campylobacter, with specific antibiotics recommended. Side effects of antibiotics used to treat various pathogens are also outlined.