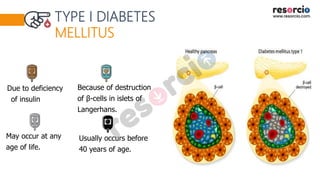
The document provides a detailed classification of diabetes mellitus, outlining its primary (Type I and Type II) and secondary forms, along with causes, symptoms, and complications. Type I diabetes is characterized by insulin deficiency, usually requiring insulin injections, while Type II involves insulin resistance and can often be managed with oral medications. Additionally, it discusses pre-diabetes, gestational diabetes, and the various complications arising from chronic hyperglycemia.