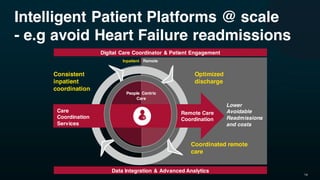
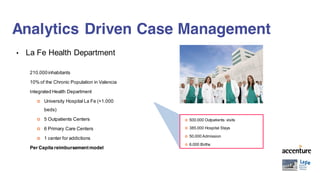
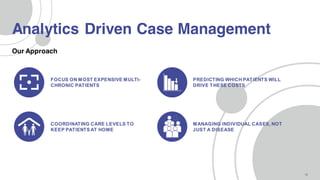
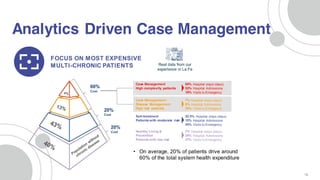
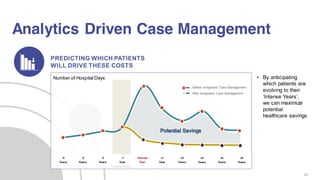
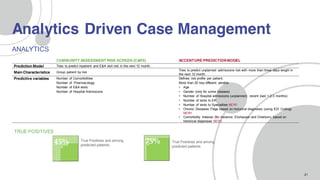
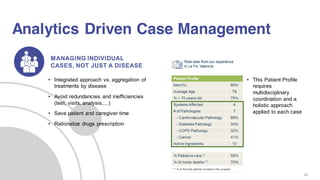
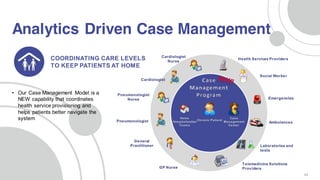
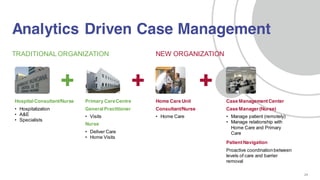
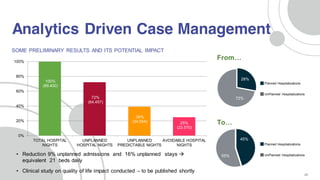
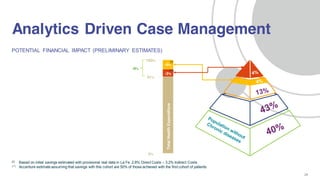
This document discusses how predictive analytics and intelligent service platforms can transform healthcare delivery at scale by leveraging data and technology while keeping people at the center. It highlights Accenture's digital health technology vision which focuses on five trends: intelligent automation, liquid workforce, platform economy, digital trust, and predictable disruption. The trends emphasize the importance of people - both patients and healthcare workers. The document also provides a case study of analytics-driven case management in Valencia, Spain that has led to reductions in unplanned hospital admissions and stays through risk stratification, coordinated care, and a holistic patient approach.